A 76 year old hypertensive male smoker with a family history of coronary artery disease was referred to the cardiac catheterisation unit after a prolonged episode of chest discomfort. Clinical examination, ECG, and laboratory tests were unremarkable, however, when performed after symptoms faded away.
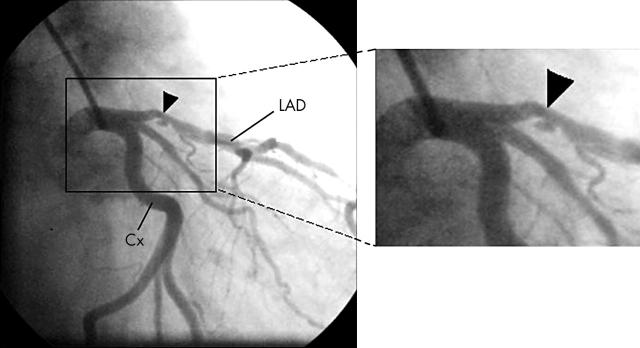
A coronary angiogram in the right anterior oblique caudal projection (right panels: Cx, circumflex artery; LAD, left anterior descending artery) revealed an ulcer with overhanging margins (arrowhead) in the proximal left anterior descending artery, most likely resulting from rupture of an atherosclerotic plaque.
Atherosclerotic lesions in native coronary arteries are contained by a fibrotic cap. Spontaneous plaque rupture occurs when this fibrous cap breaks, exposing thrombogenic lesion contents to the bloodstream. Plaque rupture is commonly associated with acute myocardial infarction or unstable angina.
Since the patient was asymptomatic at the time of coronary angiography and only a moderately stenotic lesion was found, no percutaneous coronary intervention was planned.
Dobutamine stress echocardiography was performed to discard any inducible ischaemia and the patient was discharged on aspirin, statins, and angiotensin converting enzyme inhibitors in an attempt to pursue plaque stabilisation and improve endothelial function.
Although the patient was symptom-free, coronary angiography was performed at six months, showing no changes in the aspect of the ulcer.