Abstract
Objectives: To compare self reported quality of life with measured exercise capacity in patients with congenital heart disease.
Design: Prospective cross sectional clinical study
Setting: Tertiary referral centre for congenital cardiology
Patients and methods: 149 patients (60 female, 14–60 years old) with various congenital heart defects completed a health related quality of life questionnaire (medical outcomes study 36 item short form). Then they performed a cardiopulmonary exercise test on a bicycle in a sitting position.
Results: Peak oxygen uptake correlated significantly with the physical functioning (r = 0.521, p < 0.0005) and general health scales (r = 0.313, p < 0.0005) but not with role-physical, bodily pain, vitality, social functioning, role-emotional, mental health, and health transition scales. Closer examination of the data showed that despite an overall good correlation a substantial number of patients overestimated their physical capabilities.
Conclusions: Exercise tests and quality of life instruments should be used together to get an appropriate overview of the health status of patients with congenital heart disease.
Keywords: congenital heart disease, quality of life, cardiopulmonary exercise test
Advances in surgical, interventional, and medical treatment have increased the life expectancy of patients with congenital heart disease substantially over the past 50 years. The main outcome criteria of clinical studies changed from mortality to functional parameters such as gradients, cardiac output, and exercise performance. However, these functional parameter are not sufficient to characterise patients in follow up studies. Medical management also has an influence on cognitive, emotional, and psychological issues. Additionally, it may be more important for the patients how they themselves characterise their situation and whether they are confident with their own situation.
For that reason, several self reported health related quality of life instruments have been evaluated. In congenital cardiology Meijboom and colleagues were the first to use a standardised, evaluated Dutch questionnaire in their follow up studies of patients after surgical closure of atrial septal defect1 and ventricular septal defect2 and of patients after surgical repair of tetralogy of Fallot3 and transposition of the great arteries.4 Other authors5–9 simply described the psychosocial situation of adults and children with congenital heart defects.
Those studies directly comparing objective parameters of exercise capacity with subjective data from quality of life questionnaires are limited to a small number of mostly selected patients,10 lack a standardised assessment of objective physical data,8,11 or are contradictory.3,4
Peak oxygen uptake is considered to be the best test parameter for exercise capacity and cardiopulmonary fitness.12 It is the best predictor for survival not only of patients with heart failure13,14 or coronary artery disease,15,16 but also of the general population.17
Therefore, we conducted a study to compare the self reported quality of life with peak oxygen uptake in patients with congenital heart disease.
METHODS
Patients
From June 2001 to March 2003, 198 patients were referred for a cardiopulmonary exercise test. If a patient was sent twice the results of only the first test were analysed.
Thirty one patients younger than 14 years were excluded, as the quality of life instrument used in this study is not validated for children younger than 14 years. Another 11 patients with a motion sensible rate response pacer were excluded, as they have to be tested on a treadmill, which results in a 10% higher peak oxygen uptake than when tested on a bicycle. Furthermore, five patients from abroad were not able to speak German. Another two patients were intellectually not able to understand the questions of the quality of life instrument and also had to be excluded from the study.
The indication for the exercise test depended on the referring cardiologist and varied from checking the indication for heart transplantation for severely disabled patients to minor defects such as mitral valve prolapse for patients who wanted to participate in competitive sport.
In total 149 patients with a median age of 23.8 years (range 14.0–59.8 years) were enrolled in the study. Sixty (40%) were female. Table 1 lists diagnoses, comprising almost the whole field of congenital cardiology. One hundred six patients (71%) underwent surgery before the study for their congenital heart disease, some of them several times.
Table 1.
Diagnoses of the 149 patients studied
| Diagnosis | Number |
| Univentricular heart (8 after Fontan surgery, 1 after bidirectional Glenn anastomosis, 1 after atrioseptectomy, 3 without surgery) | 13 |
| Congenitally corrected transposition of the great arteries | 9 |
| Transposition of the great arteries (4 after arterial switch operation, 20 after Senning procedure, 23 after Mustard procedure) | 47 |
| Tetralogy of Fallot | 32 |
| Truncus arteriosus | 2 |
| Aortic coarctation | 7 |
| Aortic valve stenosis | 3 |
| Pulmonary stenosis (4 valvar, 1 infundibular, 1 peripheral) | 6 |
| Ebstein’s anomaly | 7 |
| Atrioventricular septal defect | 1 |
| Ventricular septal defect | 5 |
| Atrial septal defect | 3 |
| Persistent foramen ovale | 3 |
| With mitral valve prolapse | 3 |
| Abnormal left coronary artery originating from the pulmonary artery | 1 |
| Left ventricular aneurysm of unknown origin | 1 |
| Idiopathic dilatation of the pulmonary artery | 1 |
| Structurally normal hearts tested for the assessment of arrhythmia | 5 |
Quality of life
Patients’ quality of life was assessed by the medical outcomes study 36 item short form (SF-36). This is a generic measure of health status or health related quality of life, evaluated and used in various specialities of medicine and not specific for symptoms of any disease. It is also intended for use in international studies,18 as multiple translations are available and their comparability has been tested. This instrument consists of 36 questions that can be answered in about 10 minutes by ticking one of 3–6 given answers. It is a multidimensional instrument with eight multi-item components assessing physical functioning (the extent to which health limits daily physical activities), role functioning-physical (the extent of which physical health interferes with work or other daily activities), bodily pain (the extent of bodily pain and its effect on daily life), general health perception, vitality, social functioning (the extent to which health interferes with social activities), role functioning-emotional (the extent to which emotional problems interfere with daily activities), and mental health (a rough score for depression, affect, anxiety, etc). A single item component assesses health transition (health changes in the past year). The score of each component is converted to scales from 0–100 with higher scores representing a better quality of life. We used the self reporting questionnaire with a window of four weeks in the German translation.19,20 All questionnaires were checked for missing answers and patients were asked to fill out the form completely.
Age related reference values of both sexes (14–20 years, 21–30 years, 31–40 years, an so on to 71–93 years) were taken from the German evaluation study of the SF-36.20
Cardiopulmonary exercise test
After completing the quality of life questionnaire the patients underwent a symptom limited cardiopulmonary exercise test on an electronically braked bicycle in a sitting position according to international guidelines.12,21 Various stepwise or rampwise protocols were used. Most of the patients cycled according to a protocol with a three minute warm up at 15 W followed by a rampwise increase of load with 10 or 20 W/min depending on the individual estimation of the attending physician to reach a cycling time after warming up of 8–12 minutes.
Oxygen uptake was measured breath by breath by a metabolic chart (Vmax 229, SensorMedics, Viasys Healthcare, Yorba Linda, California, USA). Peak oxygen uptake was defined as the mean oxygen uptake in that 30 second period that was highest throughout the exercise test. Reference values for peak oxygen uptake (in ml/kg/min) were calculated from height (m), weight (kg), and age (years) according to Cooper and Storer22:
for females: = 5.8 + (62.6 × height − 45.5) × (37.03 − 0.371 ×age)/weight
for males: = 5.8 + (71.6 × height − 51.8) × (44.22 − 0.394 × age)/weight
All exercise tests were performed with the attendance and supervision of one of the authors (AH).
Statistical analysis
Data were statistically analysed with a standard statistical package (SPSS 11.0, SPSS Inc, Chicago, Illinois, USA).
The primary analysis of the study was to correlate peak oxygen uptake with the nine scales of the SF-36 health related quality of life instrument. As quality of life was expressed as a score, non-parametric Spearman’s rank correlation coefficients were calculated. Owing to multiple testing only p < 0.05/9 (that is, p < 0.0055) were accepted as significant, according to the Bonferroni correction.
Furthermore, peak oxygen uptake and scores of the SF-36 scales were compared with individual reference values by two tailed Wilcoxon’s paired signed rank tests to describe the study group.
All measured parameters are expressed as median (range).
RESULTS
Quality of life
All study patients completed the quality of life questionnaire properly and all scores could be calculated. Table 2 shows medians, quartiles, and ranges of the scores. Several scores were less than expected from the age and sex related reference values.
Table 2.
Results of the quality of life instrument (SF-36, score 0–100) and the cardiopulmonary exercise test of 149 patients with congenital heart disease and their relation to individual reference values
| Result | Reference | p Value* | |||||
| Median | Range | First, third quartile | Median | Range | First, third quartile | ||
| SF-36 | |||||||
| Physical functioning | 85 | 15–100 | 65, 95 | 96 | 83–96 | 94, 96 | <0.0005† |
| Role-physical | 100 | 0–100 | 50, 100 | 93 | 78–98 | 89, 98 | 0.001† |
| Bodily pain | 100 | 22–100 | 74, 100 | 89 | 70–92 | 84, 92 | 0.302 |
| General health | 67 | 10–100 | 47, 82 | 77 | 61–82 | 74, 80 | <0.0005† |
| Vitality | 60 | 18–100 | 42, 70 | 69 | 58–73 | 63, 73 | <0.0005† |
| Social functioning | 87 | 25–100 | 62, 100 | 92 | 85–94 | 89, 94 | 0.004† |
| Role-emotional | 100 | 0–100 | 83, 100 | 94 | 88–95 | 91, 95 | 0.159 |
| Mental health | 76 | 24–100 | 64, 84 | 76 | 70–78 | 72, 78 | 0.021 |
| Health transition | 50 | 0–100 | 50, 50 | 53 | 49–57 | 52, 53 | <0.0005† |
| Cardiopulmonary exercise test | |||||||
| Peak oxygen uptake (ml/kg/min) | 26 | 9–71 | 20, 36 | 37 | 18–68 | 33, 45 | <0.0005† |
*Calculated from a Wilcoxon test; †owing to multiple testing, only p<0.0055 is regarded as significant.
SF-36, medical outcomes study 36 item short form.
Cardiopulmonary exercise test
All cardiopulmonary exercise tests were performed without complications. No exercise test had to be stopped prematurely by the attending physician.
The median (range) respiratory exchange ratio (carbon dioxide elimination to oxygen uptake) at the end of the exercise test was 1.06 (0.88–1.25); 29 patients (19%) had a ratio less than 1.
In 13 patients (9%), minute ventilation reached the maximum voluntary ventilation, calculated as 32 times the forced expiratory volume in one second in a pre-exercise lung function test. Those patients were advised to have a pulmonary check up.
The patients reached a maximum work rate of 152 W (15–350 W). Peak oxygen uptake was 26.0 ml/kg/min (9.0–70.8 ml/kg/min). Although some patients had excellent results far above their expected values, for the total study group peak oxygen uptake was significantly lower than the calculated age, sex, height, and weight related reference values (table 2).
Correlation of quality of life scores with cardiopulmonary exercise test results
Peak oxygen uptake was correlated only with physical functioning and general health. No correlation was found with the other scales of quality of life (table 3).
Table 3.
Comparison of subjective quality of life (SF-36 scores 0–100) and objective exercise capacity (peak oxygen uptake) in 149 patients with congenital heart disease
| r | p Value | |
| Physical functioning | 0.521 | <0.0005* |
| Role-physical | 0.209 | 0.011 |
| Bodily pain | −0.039 | 0.635 |
| General health | 0.313 | <0.0005* |
| Vitality | 0.141 | 0.087 |
| Social functioning | 0.221 | 0.007 |
| Role-emotional | 0.150 | 0.067 |
| Mental health | 0.112 | 0.172 |
| Health transition | −0.175 | 0.033 |
r is the Spearman rank correlation coefficient.
*Owing to multiple testing only p<0.0055 is regarded as significant.
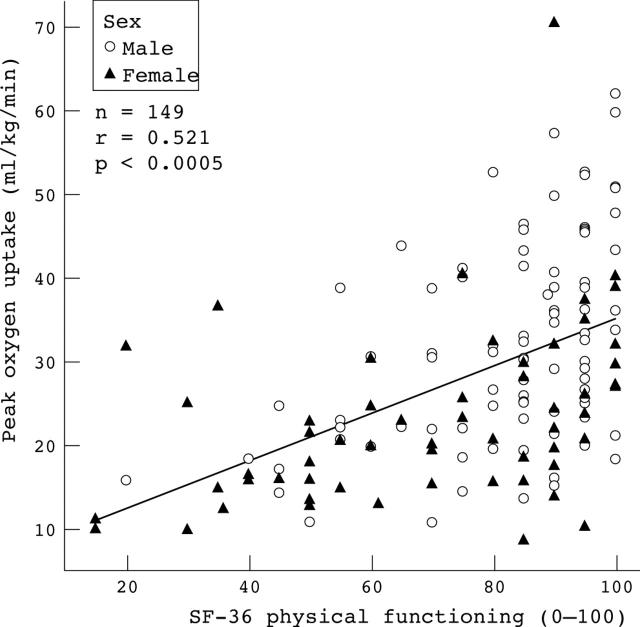
The scatter plot of the best correlation shows that most patients with a low score in self reported physical functioning also had a low peak oxygen uptake, whereas peak oxygen uptake varied very broadly among patients with a high score in the 10 questions concerning physical functioning (fig 1). This was seen in male and female patients as well as patients with and without surgery.
Figure 1.
Comparison of self reported physical functioning from the medical outcomes study 36 item short form (SF-36) quality of life instrument with peak oxygen uptake from a cardiopulmonary exercise test in 149 patients with congenital heart disease.
DISCUSSION
This study of patients with congenital heart disease clearly showed that objective exercise capacity measured in a cardiopulmonary exercise test correlates with self reported exercise capacity and self reported general health but not with other scales of quality of life.
These results are concordant with the recent study of Kamphuis and colleagues11 that found a significant correlation of the SF-36 physical functioning scale with all three scores they extracted from the medical records (New York Heart Association functional class, Somerville ability index, and a self created objective physical index scoring from 0–4). However, correlations with the other SF-36 scales were highly variable depending on the scores with which they were compared.
Studies that have used exercise tests as objective measurements did not mention other aspects of quality of life except the self (or parents’) estimation of physical capacity and classified this subjective physical capacity in only three23 or five levels.3,4 Rogers and colleagues23 reported that the parents’ estimation of their children’s exercise capacity is poor. The two studies of Meijboom and colleagues on patients after surgery for tetralogy of Fallot3 and on patients after Mustard surgery for transposition of the great arteries4 had different results and the authors did not discuss this topic in detail. This might be due to the very rough assessment of quality of life obtained by self assigning of the patients to one of five levels.
Therefore, we examined more closely the scatter plot depicting the correlation of objective exercise capacity measured as peak oxygen consumption with self reported physical capacity measured by the SF-36 physical functioning scale. We calculated a good correlation from our data, but that is at least in part due to the wide span of the data covering patients severely disabled by their heart defect and patients who wanted to be active in competitive sports. Prediction of objective exercise capacity from the 10 questions concerning physical functioning was fairly good only for patients reporting poor physical functioning. However, a substantial number of patients reporting good physical functioning had a reduced exercise capacity on the bicycle.
This overestimating of the physical capacity of patients with congenital heart disease was already mentioned by Rogers and colleagues.23 Parents were asked to classify their children’s exercise capacity as below average, average, or above average. Sixty five per cent of the parents misclassified their children with congenital heart disease; they all overestimated the exercise capacity. In our study patients were older and could estimate their own exercise capacity. They responded in the same way as the parents in the study by Rogers and colleagues.23
Recently in a study by Juenger and colleagues24 of older patients with acquired congestive heart failure this phenomenon of overestimating exercise capacity was not mentioned (but original scatter plots are not shown). Therefore a possible explanation for the phenomenon is that our patients had a congenital disease and had to cope with their diminished exercise capacity from birth onwards. They did not experience a different situation and express their situation as normal.
Study limitations
Firstly, patients were not randomly chosen for participation in the study. This might have caused a bias because of the referral practice of the cardiologists. This explains the high number of complex defects. Additionally, patients might have been referred more often if the physicians had doubts about their reported physical capacities. Furthermore, the patient distribution reflects that of our tertiary centre, which is of course different from that in the general population.
Secondly, the SF-36 is a generic instrument to assess self reported health status and quality of life. It is neither specific nor sensitive for quality of life issues of patients with congenital heart disease. But at present no well evaluated, multiply translated instrument is available for congenital heart disease as it is for heart failure or for coronary heart disease. However, this is only a minor limitation in this particular study, as we compared a generic quality of life instrument with a generic test for physical fitness. It may even be a strength of this study, as potential co-morbidity is counterbalanced. This is an important issue in longitudinal studies that aim to detect small differences in quality of life after any kind of intervention.
Conclusion
Objective exercise capacity correlates with some physical aspects of quality of life. Correlation with other aspects, especially the psychological ones, are poor; however, even the scatter of correlation with self reported physical functioning must be considered. Exercise tests and quality of life instruments should be used together to get an appropriate overview of the health status of patient with congenital heart disease.
Presented in part at the Annual Scientific Session of the American College of Cardiology, 30 March to April 2003, Chicago, Illinois, USA.
REFERENCES
- 1.Meijboom F, Hess J, Szatmari A, et al. Long-term follow-up (9 to 20 years) after surgical closure of atrial septal defect at a young age. Am J Cardiol 1993;72:1431–4. [DOI] [PubMed] [Google Scholar]
- 2.Meijboom F, Szatmari A, Utens E, et al. Long-term follow-up after surgical closure of ventricular septal defect in infancy and childhood. J Am Coll Cardiol 1994;24:1358–64. [DOI] [PubMed] [Google Scholar]
- 3.Meijboom F, Szatmari A, Deckers JW, et al. Cardiac status and health-related quality of life in the long term after surgical repair of tetralogy of Fallot in infancy and childhood. J Thorac Cardiovasc Surg 1995;110:883–91. [DOI] [PubMed] [Google Scholar]
- 4.Meijboom F, Szatmari A, Deckers JW, et al. Long-term follow-up (10 to 17 years) after Mustard repair for transposition of the great arteries. J Thorac Cardiovasc Surg 1996;111:1158–68. [DOI] [PubMed] [Google Scholar]
- 5.Kaemmerer H, Tintner H, Konig U, et al. Psychosocial problems of adolescents and adults with congenital heart defects. Z Kardiol 1994;83:194–200. [PubMed] [Google Scholar]
- 6.Casey FA, Sykes DH, Craig BG, et al. Behavioral adjustment of children with surgically palliated complex congenital heart disease. J Pediatr Psychol 1996;21:335–52. [DOI] [PubMed] [Google Scholar]
- 7.Mir TS, Eiselt M, Wallstabe B, et al. Messung der gesundheitsbezogenen Lebensqualität (LQ) von Erwachsenen mit angeborenen Herzerkrankungen mit dem SF-36 health survey. J Kardiol 2000;7:506–10. [Google Scholar]
- 8.Saliba Z, Butera G, Bonnet D, et al. Quality of life and perceived health status in surviving adults with univentricular heart. Heart 2001;86:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ternestedt BM, Wall K, Oddsson H, et al. Quality of life 20 and 30 years after surgery in patients operated on for tetralogy of Fallot and for atrial septal defect. Pediatr Cardiol 2001;22:128–32. [DOI] [PubMed] [Google Scholar]
- 10.Casey FA, Craig BG, Mulholland HC. Quality of life in surgically palliated complex congenital heart disease. Arch Dis Child 1994;70:382–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamphuis M, Ottenkamp J, Vliegen HW, et al. Health related quality of life and health status in adult survivors with previously operated complex congenital heart disease. Heart 2002;87:356–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 Guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to update the 1997 exercise testing guidelines). Circulation 2002;106:1883–92. [DOI] [PubMed] [Google Scholar]
- 13.Cahalin LP, Mathier MA, Semigran MJ, et al. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 1996;110:325–32. [DOI] [PubMed] [Google Scholar]
- 14.Myers J, Gullestad L, Vagelos R, et al. Clinical, hemodynamic, and cardiopulmonary exercise test determinants of survival in patients referred for evaluation of heart failure. Ann Intern Med 1998;129:286–93. [DOI] [PubMed] [Google Scholar]
- 15.Vanhees L, Fagard R, Thijs L, et al. Prognostic significance of peak exercise capacity in patients with coronary artery disease. J Am Coll Cardiol 1994;23:358–63. [DOI] [PubMed] [Google Scholar]
- 16.Lipinski M, Froelicher V, Atwood E, et al. Comparison of treadmill scores with physician estimates of diagnosis and prognosis in patients with coronary artery disease. Am Heart J 2002;143:650–8. [DOI] [PubMed] [Google Scholar]
- 17.Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 2002;346:793–801. [DOI] [PubMed] [Google Scholar]
- 18.Aaronson NK, Acquadro C, Alonso J, et al. International quality of life assessment (IQOLA) project. Qual Life Res 1992;1:349–51. [DOI] [PubMed] [Google Scholar]
- 19.Bullinger M . German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA project. International quality of life assessment. Soc Sci Med 1995;41:1359–66. [DOI] [PubMed] [Google Scholar]
- 20.Bullinger M, Kirchberger I. SF-36, Fragebogen zum Gesundheitszustand, Handanweisung. 1st ed. Göttingen: Hogrefe, 1998.
- 21.Washington RL, Bricker JT, Alpert BS, et al. Guidelines for exercise testing in the pediatric age group. From the Committee on Atherosclerosis and Hypertension in Children, Council on Cardiovascular Disease in the Young, the American Heart Association. Circulation 1994;90:2166–79. [DOI] [PubMed] [Google Scholar]
- 22.Cooper CB, Storer TW. Exercise testing and interpretation: a practical guide. 1st ed. Cambridge: Cambridge University Press, 2001.
- 23.Rogers R, Reybrouck T, Weymans M, et al. Reliability of subjective estimates of exercise capacity after total repair of tetralogy of Fallot. Acta Paediatr 1994;83:866–9. [DOI] [PubMed] [Google Scholar]
- 24.Juenger J, Schellberg D, Kraemer S, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart 2002;87:235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]