Longitudinal function of the left ventricle is governed by the subendocardial myocardial fibres, whereas radial function is due mainly to contraction of circumferential fibres, localised in the subepicardial layer of the myocardium.1 In patients with diabetes or hypertension the subendocardial fibres are more likely to be affected by microvascular ischaemia. This can be caused by structural changes in the coronary vasculature that reduce myocardial perfusion such as arterial wall thickening, decreased capillary density, and periarteriolar fibrosis, and by haemodynamic changes such as increased wall stress, and the microcirculatory effects of endothelial dysfunction.2 Since tissue Doppler echocardiography can now assess longitudinal and radial myocardial velocities separately, we tested the further hypothesis that subendocardial dysfunction is related to conduit arterial stiffness.
METHODS
Study group
We studied 83 subjects (mean (SD) age 54 (12) years, 59 men), including 27 normal individuals and 56 patients with varying degrees of left ventricular (LV) dysfunction caused by diabetes (35), hypertension (17), and ischaemic dilated cardiomyopathy (4). We excluded patients not in sinus rhythm, or with ventricular aneurysm or severe regional wall motion abnormalities, mitral or aortic stenosis, or more than mild valvar regurgitation. Twenty nine patients were taking an angiotensin converting enzyme (ACE) inhibitor, 23 a diuretic, 8 a β blocker, 27 a statin, and 7 a calcium antagonist. The protocol was approved by the local research ethics committee, and each subject gave informed consent.
Arterial stiffness
Subjects were studied after resting supine for 15 minutes in a temperature controlled environment. The stiffness parameter β was calculated according to the formula:
 |
where Ps and Pd are systolic and diastolic blood pressure in the brachial artery measured by an automated sphygmomanometer (Omron 705CP, Tokyo, Japan), and Ds and Dd are the maximal and minimal diameters of the right common carotid artery measured by ultrasonic high resolution wall tracking (Aloka SSD-5500, Tokyo, Japan; 7.5 MHz linear array probe).3 Adjustable gates were positioned at the junctions of the intima and media, and diameter was calculated and displayed in real time as the difference between the displacement waveforms of the anterior and posterior walls. Measurements were taken as a mean of five beats; β was log transformed for analyses, because its distribution was skew.
Echocardiography
Immediately after assessment of arterial stiffness, subjects were studied by conventional and tissue Doppler echocardiography (Vingmed System 5, GE Vingmed, Horten, Norway), using a 1.5–2.5 MHz transducer. Digital echocardiographic data were acquired and transferred to a Macintosh computer.
Conventional echocardiography
M mode tracings from the parasternal long axis view were used to measure septal thickness, LV diameter, and posterior wall thickness, and LV mass index was calculated (method of Devereux with the application of the Penn convention). Cross sectional images were recorded from the apex, and end diastolic and end systolic areas were measured for the calculation of ejection fraction (modified biplane Simpson‘s method). Left ventricular inflow was recorded by colour M mode echocardiography and flow propagation velocity was measured. LV diastolic filling pressure was estimated from the ratio of mitral E wave, by pulsed wave Doppler, to mitral annular early diastolic velocity (Ea wave) by pulsed wave tissue Doppler.
Regional myocardial velocities
Digital loops were retrieved and off-line tissue Doppler measurements were made in five myocardial segments: radial function from the basal posterior wall (parasternal long axis view), and longitudinal function from the velocities of basal septal and basal lateral segments (apical four chamber view), and basal anterior and basal inferior segments (apical two chamber view). Peak myocardial velocities in systole and early diastole were measured using customised software (Echopac TVI, GE Vingmed; mean of two consecutive beats). Velocities of the four segments imaged from the apex were averaged.
RESULTS
Univariate analysis
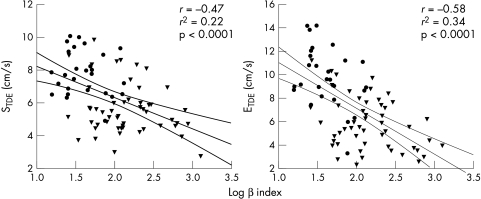
Arterial stiffness (β) was inversely related to LV longitudinal function (r = −0.47 for average peak systolic velocity, r = −0.58 for early diastolic velocity, both p < 0.0001) (fig 1), but it was not related to radial systolic velocity (r = −0.03) or to global ejection fraction (r = −0.19). There was an inverse relation between β and radial early diastolic velocity (r = −0.34, p < 0.01), and with global diastolic function (inverse relation with flow propagation velocity, r = −0.55; and direct relation with estimated LV filling pressure, r = 0.47; both p < 0.0001). β Index was positively related to LV wall thickness (r = 0.26 for the ventricular septum and r = 0.35 for the posterior wall, both p < 0.05).
Figure 1.
Correlations between longitudinal (subendocardial) left ventricular function (STDE = mean systolic velocity, ETDE = mean early diastolic velocity) and arterial stiffness (log transformed β index). • = normal subjects; ▾ patients with left ventricular dysfunction.
Multivariate analysis
By stepwise multiple regression analysis (parameters tested: age, systolic and diastolic blood pressure, pulse pressure, LV mass index, body mass index, and β index), longitudinal (subendocardial) LV average peak systolic velocity was shown to be independently and inversely related to β index and LV mass index (r = 0.54, r2 = 0.29, p < 0.0001), but not to the other parameters tested. Longitudinal early diastolic velocity was inversely related to age and β index (r = 0.69, r2 = 0.47, p < 0.0001).
DISCUSSION
These results suggest that subendocardial function of the left ventricle may be depressed in patients whose conduit arteries are stiffer and less compliant than normal. Reduced compliance of the large arteries modifies the timing of wave reflections and thus determines ventricular load. Ventricular ejection generates a forward pressure wave, which travels from the heart at a speed labelled pulse wave velocity (PWV). This wave is reflected from the arterial tree as a wave travelling backwards to the heart. In young subjects PWV is low, and the reflected wave can reach the ascending aorta after the aortic valve has closed; central systolic pressure may be unchanged, but the backward wave increases central diastolic pressure and coronary perfusion pressure. In subjects with increased arterial stiffness, such as patients with hypertension and/or diabetes, PWV is high (perhaps 20 m/s compared with 5 m/s in normals), and the backwards wave from the periphery returns early to the ascending aorta. It arrives during LV ejection, increasing central systolic blood pressure and LV afterload, and decreasing central diastolic and coronary perfusion pressures.4 The net effect of these haemodynamic changes may be ischaemia particularly in the subendocardium, which if chronic is associated with interstitial fibrosis and the development of heart failure.2 Aortic stiffness has been reported recently to be an independent predictor of all cause mortality and of cardiovascular mortality in hypertensive subjects.5
Our data confirm that LV subendocardial function is inversely related to conduit arterial stiffness, and suggest that non-invasive assessment of the β index might be useful for studying the effects on arterial stiffness of treatment designed to optimise ventriculo-arterial coupling and cardiac performance.
REFERENCES
- 1.Greenbaum RA, Ho SY, Gibson DG, et al. Left ventricular fibre architecture in man. Br Heart J 1981;45:248–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohtsuka S, Kakihana M, Watanabe H, et al. Alterations in left ventricular wall stress and coronary circulation in patients with isolated systolic hypertension. J Hypertens 1996;14:1349–55. [DOI] [PubMed] [Google Scholar]
- 3.Kawasaki T, Sasayama S, Yagi S, et al. Non-invasive assessment of the age related changes in stiffness of major branches of the human arteries. Cardiovasc Res 1987;21:678–87. [DOI] [PubMed] [Google Scholar]
- 4.London GM, Guerin A. Influence of arterial pulse and reflected waves on blood pressure and cardiac function. Am Heart J 1999;138:220–4. [DOI] [PubMed] [Google Scholar]
- 5.Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001;37:1236–41. [DOI] [PubMed] [Google Scholar]