Figure 3.
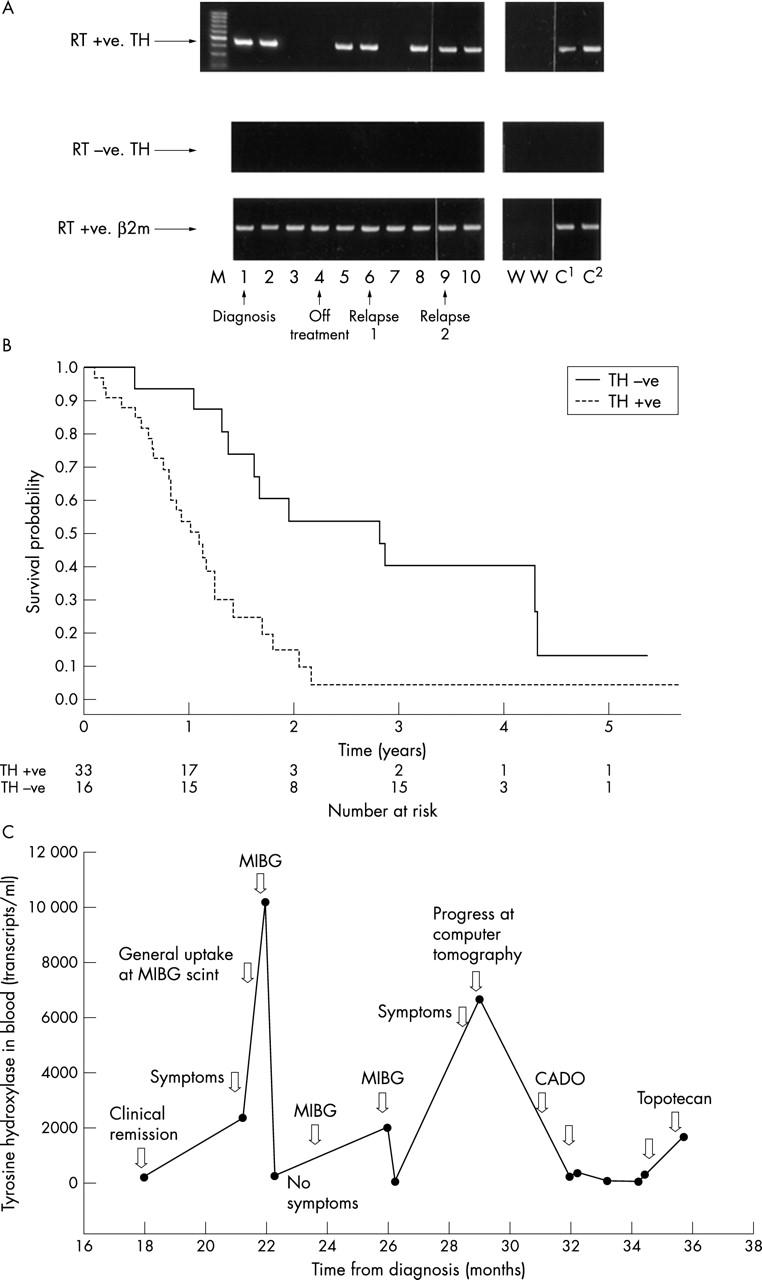
Assessment of disease status by reverse transcriptase polymerase chain reaction (RT-PCR) in children with neuroblastoma (NBL). RT-PCR and RT real time PCR are the most sensitive and specific methods for the detection of micrometastases, although their clinical usefulness is unclear. Using PCR based methods it is not possible to measure absolute NBL cell numbers, but changes in disease can be monitored throughout the disease course by RT-PCR (A) or RT real time PCR (C). (A) Detection of tyrosine hyroxylase (TH) mRNA (NBL cells) in sequential blood samples taken from a child with stage 4 NBL. Blood samples were positive at diagnosis (1) and four weeks into treatment (2), but negative five (3) and seven (4) weeks after the start of treatment. Peripheral blood (PB) was positive for TH mRNA at 13 weeks (5) and when the child was clinically disease free at 12 months (6), but negative at 13 months (7). Before clinical relapse the PB was positive (8; 14 months), and remained positive (9; 17 months) until relapse 19 months after initial diagnosis (10). The child did not respond to further treatment and died of disease 22 months after initial diagnosis. RT+ve, RT present; RT-ve, RT absent (negative control); β2m, β2 microglobulin mRNA (housekeeping gene used to check quality of RNA); M, molecular weight markers; W, negative control; C1 and C2, positive controls. (B) The presence of TH mRNA in PB from children with high risk (stage 4) NBL greater than 1 year old at diagnosis is associated with an increased risk of death; p = 0.002 (95% confidence interval, 1.49 to 6.66), log rank test. (C) TH mRNA detected by RT real time PCR in PB from a child with stage 4 NBL taken 18–36 months after diagnosis. TH mRNA increased in PB at the time of relapse and dropped after further treatment. (A, B) Reproduced from Burchill et al;25 (C) reproduced from Träger et al.29 CADO, vincristinecyclo-phosphamide-doxorubicin; MIBG, I-125 metaiodobenzylguanidine.
