Abstract
This report describes the case of an asymptomatic, solitary splenotic nodule in the right ovary, revealed incidentally at histopathological examination. In gynaecological patients, splenosis most often presents as multiple pelvic nodules mimicking endometriosis. Two cases of ovarian splenosis accompanying pelvic and serosal splenotic nodules have been reported previously. However, this is the first documented case of solitary intraovarian splenosis.
Keywords: ovarian splenosis, ectopic splenic tissue
The pathogenesis of splenosis is ascribed to autotransplantation of splenic tissue as a consequence of splenic trauma or surgery.1 There is implantation of splenic tissue in the form of encapsulated nodules. It can occur on the peritoneal surface, pelvis, abdominal wall, pleural cavity, lung parenchyma, and rarely in the brain. Splenosis is most often encountered in the peritoneal cavity after splenic rupture. Intrathoracic and subcutaneous splenosis occur when trauma causes a path of entry for implantation of splenic tissue. However, in cerebral splenosis a haematogenous spread of splenic tissue has to be assumed.
“To our knowledge, there are no reported cases of solitary intraovarian splenosis”
In gynaecological patients, the most common presentation is asymptomatic pelvic nodules mimicking endometriosis, either discovered incidentally or presenting as pelvic pain. To our knowledge, there are no reported cases of solitary intraovarian splenosis.
There are two alternative, albeit unlikely explanations for this phenomenon. The first is an accessory (supernumerary) spleen and the second is splenogonadal fusion. These will be considered in more detail later.
CASE REPORT
A 61 year old woman presented with recurrent postmenopausal vaginal bleeding. Physical examination was unremarkable and a transvaginal ultrasound showed no abnormalities. Histopathological study of endometrial curettage specimens taken on two occasions showed no abnormalities. In view of the persistent vaginal bleeding, she was offered a total abdominal hysterectomy and bilateral salpingoopherectomy, which she accepted.
Her past history was notable in that she had undergone a splenectomy at the age of 16 years, after splenic trauma in a road traffic accident.
PATHOLOGICAL FINDINGS
The uterus, cervix, Fallopian tubes, and ovaries were unremarkable on gross examination. Microscopy of the right ovary showed a well defined nodule, 2 cm in maximum dimension, with features almost indistinguishable from normal spleen. White pulp composed of lymphoid aggregates centred round arterioles was present. This tissue was embedded in highly vascular red pulp composed of broad anastamosing venous sinuses. A capsule was also identified from which short trabeculae extended into the parenchyma. Normal ovarian stroma was present at the periphery (figs 1, 2).
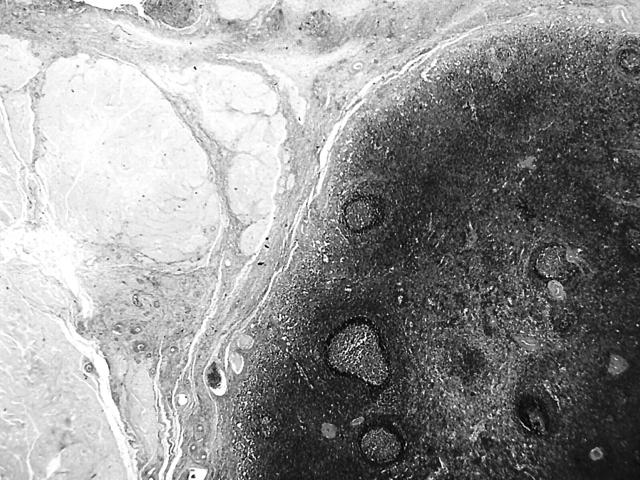
Figure 1.
Medium power view showing a well defined nodule of splenosis and normal ovarian tissue in the periphery.
Figure 2.
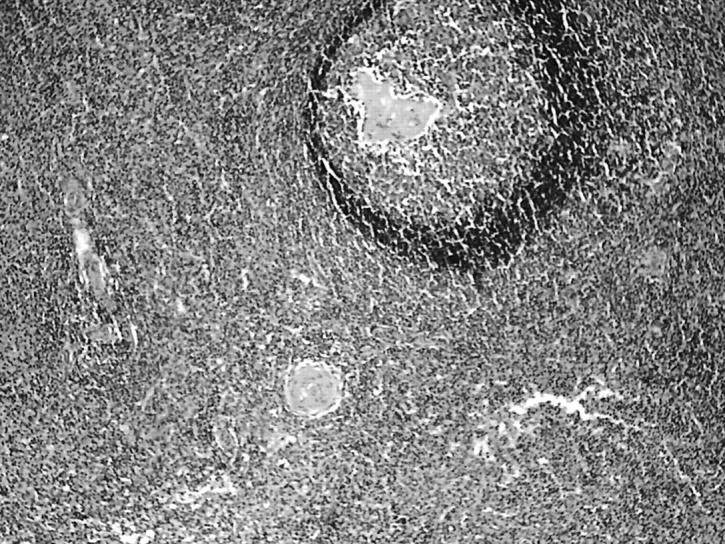
High power view of the splenotic nodule showing features indistinguishable from normal spleen.
DISCUSSION
Two cases of ovarian splenosis accompanied by multiple pelvic and serosal nodules clinically mimicking endometriosis have been described previously.2,3 However, to the best of our knowledge, our present case is the first documented case of solitary intraovarian splenosis.
Histologically, in splenosis the splenic tissue may be poorly developed architecturally or, as in this case, indistinguishable from the parent organ. Although many authors state that various features can differentiate splenosis from accessory spleen histologically, Carr and Turk4 report two cases in which, as in our case, histology was unhelpful because there were no distinguishing features between the two.
The differential diagnoses to be considered in this case are accessory spleen and splenogonadal fusion.
“Histologically, in splenosis the splenic tissue may be poorly developed architecturally or, as in this case, indistinguishable from the parent organ”
The former occurs in about 10% of individuals and can be solitary or multiple with histological and functional features similar to those of the normal spleen. This occurs as a result of the normal multifocal development of spleen and subsequent failure of fusion of one or more contributory foci. The most common site is the splenic hilum. Less frequently it occurs in the tail of the pancreas and has been reported in the liver and retroperitoneum.
Splenogonadal fusion is the result of fusion of the splenic and gonadal anlage during embryonic development. Most reported cases are in males, which may not necessarily reflect a true difference in incidence but may be, as noted by Watson,5 the result of the fact that the situation of the male gonads makes them more accessible to examination. In addition, except for one case, the fusion involved the left gonad.6 Splenogonadal fusion occurs in two forms. One is continuous, in which a fibrous band connects the gonadal and splenic structures. The other is discontinuous, in which discrete masses of splenic tissue are found fused to the gonadal structures. The first form is associated with congenital malformations, including limb defects and micrognathia. Meneses and Ostrowski7 described the first reported case of discontinuous splenogonadal fusion in a female, which occurred as intraovarian splenic tissue in the left ovary.
Take home messages.
To the best of our knowledge, this is the first reported case of solitary ovarian splenosis
Although it is impossible to determine with certainty that this does not represent an accessory spleen in the ovary, the past history of splenic trauma and splenectomy strongly support the diagnosis of splenosis
The final possibility of splenogonadal fusion can also be disregarded with caution because all reported cases of splenogonadal fusion with the exception of one possible case involve the left gonad, and most cases occur in males
Acknowledgments
We are deeply grateful to Dr S Trotter, Consultant Pathologist, Birmingham Heartlands Hospital for taking the pictures used in this case report.
REFERENCES
- 1.Brunning RD, Desmet VJ, Ordonez NG, et al. Splenosis. In: Rosai and Ackerman’s surgical pathology. 9th ed. St Louis: Mosby 2004:2020–75.
- 2.Tawfik O, Balarezo F, Weed J. Splenosis. A report of ovarian stromal involvement. Kans Med 1998;98:14–16. [PubMed] [Google Scholar]
- 3.Watson WJ, Sundwell DA, Benson WL. Splenosis mimicking endometriosis. Obstet Gynecol 1982;6 (suppl) :51S–3S. [PubMed] [Google Scholar]
- 4.Carr NJ, Turk EP. The histological features of splenosis. Histopathology 1992;21:549–53. [DOI] [PubMed] [Google Scholar]
- 5.Watson RJ. Splenogonadal fusion. Surgery 1968;63:853–8. [PubMed] [Google Scholar]
- 6.Rosenthal JT, Bedetti CD, Labayen RF, et al. Right splenogonadal fusion with associated hypersplenism. J Urol 1981;126:812–14. [DOI] [PubMed] [Google Scholar]
- 7.Meneses MF, Ostrowski ML. Female spleno–gonadal fusion of the discontinuous type. Hum Pathol 1989;20:486–8. [DOI] [PubMed] [Google Scholar]