Abstract
Aims: To evaluate how tumour size, retinal location, and patient age affect the outcome of retinoblastoma foci treated with chemotherapy.
Methods: Retrospective review of retinoblastoma foci treated with primary chemotherapy alone. Individual tumours were coded with regard to their largest basal diameter, location within the eye (macula, macula to equator, equator to ora serrata), and patient's age at diagnosis. Successfully treated tumours required no further intervention while those requiring additional treatment were coded as failures.
Results: 56 (72%) tumours responded successfully to chemotherapy alone while 22 (28%) required additional therapy. 26 of 31 macular tumours (84%) and 30 of 47 extramacular tumours (64%) responded to chemotherapy (p <0.060). Relative to size, 46 of 60 tumours (77%) greater than 2 mm in basal diameter were successfully treated with chemotherapy, while only 10 of 18 tumours (56%) less than or equal to 2 mm responded (p <0.088). Among the eight tumour foci diagnosed in children less than 2 months of age, five (63%) failed to respond to chemotherapy alone (p <0.032).
Conclusion: Retinoblastoma is more likely to respond to primary chemotherapy if it is located in the macula and if the patient is older than 2 months of age. Tumours measuring less than 2 mm in diameter may be less responsive to this treatment.
Keywords: retinoblastoma, chemotherapy, children
The role of chemotherapy in treating intraocular retinoblastoma has rapidly progressed since the earliest reports were published in the last decade.1–7 Initially used only in advanced cases with a poor prognosis,4 systemic chemotherapy has gradually replaced external beam radiotherapy as a primary treatment. The treatment is often combined with other techniques including plaque radiotherapy, cryotherapy, and diode laser hyperthermia.2,4,8–11 While success rates remain high with this approach, there remain some tumours that fail to respond to chemotherapy at all and others that relapse quickly. Alternative treatments such as plaque and external beam radiotherapy are often employed to salvage these cases.
We have observed a large variability in the response of retinoblastoma to chemotherapy and often find it difficult to predict which tumours will fail treatment. While a number of studies have looked at the relation between Reese-Ellsworth group and response rates few have considered individual tumour features such as size and intraocular location.4,12,13 Some centres have assessed size in the setting of thermotherapy but none has done so in relation to chemotherapy alone.14 It was our intention to evaluate how tumour size, location, and patient age at diagnosis correlated with response rates of retinoblastoma foci treated only with chemotherapy. Identifying factors predictive of outcome would allow us to use this treatment more effectively, thereby reducing failure rates. Visual loss and retinal damage might be reduced if adjuvant therapy such as laser hyperthermia could be avoided, especially within the macula.
METHODS
A retrospective review was performed using the records of the Ocular Oncology Service of St Bartholomew's and Moorfields Eye Hospitals. Included were children treated with primary chemotherapy alone for intraocular retinoblastoma. Our protocol includes carboplatin, vincristine, and etoposide given at 21 day intervals and has been published elsewhere.4 Initially it was our practice to administer eight cycles of chemotherapy but this has since been reduced to six cycles.
The sex of each patient was recorded as was his/her genetic presentation (familial versus sporadic). Each eye was grouped using the Reese-Ellsworth classification and listed as either left or right eye. Individual tumour foci were coded with regard to their size and location within the eye at the time of diagnosis. The size recorded was the largest basal diameter in millimetres as estimated by one the authors (JLH) using indirect ophthalmoscopy (based upon the principle that an image spanning the diameter of a 20 dioptre lens measures approximately 12 mm). Where available ultrasound measurements were used to correlate these findings (particularly for large tumours). Retinal location was classified as one of three zones: macula, equator, and ora. The macular zone was defined as that part of the retina between the superior and inferior temporal arterioles. The equatorial zone spanned from the borders of the macular zone to the equator, as estimated by the presence of vortex veins. The final ora location included the remaining anterior portion of the retina up to the ora serrata.
Each tumour focus was then coded as having responded successfully or having failed chemotherapy. Failure was defined as lack of response or continued growth of the tumour requiring additional treatment (as assessed by one of the authors, JLH). Classifying a successful response necessitated at least a 1 year period free of tumour recurrence or growth. Those tumours responding to chemotherapy but with less than 1 year of follow up were not included in this study. Tumour foci initially treated with chemotherapy and subsequently receiving external beam radiotherapy due to treatment failure of an adjacent tumour were excluded. Cases initially selected for treatment using chemotherapy as part of a multimodal approach utilising diode laser hyperthermia, cryotherapy, or radiotherapy were also excluded. A univariate and bivariate logistic regression analysis was used to evaluate statistically how each tumour characteristic (location, size, and age at diagnosis) correlated with response to chemotherapy.
RESULTS
Of the initial 42 patients reviewed 36 met the inclusion criteria. Eighteen (50%) patients were male, 10 (28%) had a positive family history and eight (22%) were unilateral sporadic cases. Three patients received primary systemic chemotherapy with additional adjuvant intrathecal administration (cytarabine, methotrexate, and hydrocortisone) due to adverse histological findings on contralateral enucleation. Among the 42 eyes there were 78 individual tumour foci treated with chemotherapy alone. The Reese-Ellsworth group of these eyes ranged from Ia to Vb (see Table 1) Thirty one (40%) tumours were located in the macular zone. Thirty nine (50%) were identified in the equatorial region and eight (10%) tumour foci were in the anterior ora zone (see Table 2). Basal tumour dimensions ranged in size from 0.25 mm to 17 mm with a mean of 6.6 mm. Age at diagnosis ranged from 2 weeks to 5 years with a median of 6 months (mean 8.8 months).
Table 1.
Reese-Ellsworth group of eyes treated with chemotherapy
| Reese-Ellsworth group | Ia | Ib | IIa | IIb | IIIa | IIIb | IVa | IVb | Va | Vb | Total number of eyes |
| Stage at presentation | 2 | 2 | 11 | 8 | 8 | 1 | 1 | 1 | 0 | 8 | 42 |
| Eyes with tumours successfully treated | 1 | 0 | 10 | 7 | 4 | 0 | 0 | 0 | 0 | 2 | 24 |
| Eyes with tumours failing treatment | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 0 | 6 | 18 |
| Eyes enucleated for failed salvage treatment | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 3 | 8 |
Table 2.
Location of tumour foci treated with chemotherapy
| Successful responses | Failures | Total | |
| Macula* | 26 | 5 | 31 |
| Equatorial region* | 26 | 13 | 39 |
| Anterior ora* | 4 | 4 | 8 |
| Total | 56 | 22 | 78 |
*As defined in the text.
Fifty six (72%) tumours responded successfully to chemotherapy alone while 22 (28%) required additional therapy. Twenty six of 31 (84%) macular tumours, 26 of 39 (67%) tumours in the equatorial zone, and four of eight (50%) anterior tumour foci responded to chemotherapy (p <0.060) (see Table 2). The mean basal dimensions were 6.7 mm for successfully treated tumours and 6.2 mm for those failing chemotherapy. The mean follow up time for successfully treated tumours was 29 months (median 33 months, range 12–44 months). Failure to respond to chemotherapy occurred 2–25 months following treatment (mean 10.8 months, median 11months). Eight of 18 tumours (44%) less than or equal to 2 mm in basal diameter failed chemotherapy while 14 of 60 tumours (23%) greater than 2 mm required additional treatment (p<0.088). The 22 tumours failing chemotherapy were detected in 18 eyes, of which 10 (56%) were salvaged by alternative means. The remaining eight eyes were enucleated (see Table 1).
A univariate logistic regression analysis was used to establish which variables were associated with a successful response to chemotherapy. Those with the strongest correlation were age at diagnosis greater than 2 months, macular location, sporadic inheritance, and tumour size greater than 2 mm (see Table 3). Age was a confounding variable and was itself associated with tumour size and genetic inheritance. A bivariate logistic regression model was constructed to assess the relation of these variables to outcome. This statistical evaluation continued to suggest that macular location and size were independently associated with a successful response to chemotherapy. A backward elimination analysis confirmed that age at diagnosis greater than 2 months, macular location, and sporadic presentation were independent variables associated with a successful response to chemotherapy. However in this final assessment the relation between tumour size and outcome was no longer statistically significant.
Table 3.
Statistical evaluation correlating variable with successful response to chemotherapy
| Variable | Odds ratio | 95% CI | p Value |
| Univariate logistic regression analysis | |||
| Age greater than 2 months | 5.10 | (1.12 to 24.01) | 0.032 |
| Macular location | 2.95 | (0.95 to 9.09) | 0.060 |
| Sporadic presentation | 2.54 | (0.88 to 7.35) | 0.088 |
| Basal dimension greater than 2 mm | 2.63 | (0.87 to 7.94) | 0.088 |
| Bivariate logistic regression that includes age | |||
| Macular location | 3.70 | (1.08 to 12.69) | 0.025 |
| Sporadic presentation | 1.50 | (0.40 to 5.69) | 0.554 |
| Basal dimension greater than 2 mm | 2.16 | (0.68 to 6.89) | 0.199 |
p Values refer to the significance of the individual variable; odds ratios are for successful response to treatment.
DISCUSSION
This study reviewed our experience of treating intraocular retinoblastoma with primary chemotherapy alone. Our findings indicate that retinoblastoma is more likely to respond to systemic chemotherapy if the lesions are located in the macula and if the patient is older than 2 months of age. Statistical analysis also suggests tumours measuring less than 2 mm in diameter may be less responsive to this treatment.
Clinically it can be challenging to predict the response of retinoblastoma foci to chemotherapy. Some tumours, particularly larger ones, can have a dramatic reduction in size leaving nothing but an atrophic scar (Fig 1). Others, often smaller, can be less responsive with little or no change in appearance (Fig 2). This variability prompted us to investigate how certain features, such as size and location, correlate with the response of retinoblastoma foci to treatment. We retrospectively reviewed all patients treated in our centre with chemotherapy using a protocol we have published before.4 We excluded tumours concomitantly receiving thermotherapy during drug delivery (chemothermotherapy). To ensure that we had assessed tumour response adequately, we excluded any tumour responding to chemotherapy with less than 1 year of follow up. The size, location, and response of tumours was determined by our senior ophthalmologist (JLH) and based upon his experience in this discipline.
Figure 1.
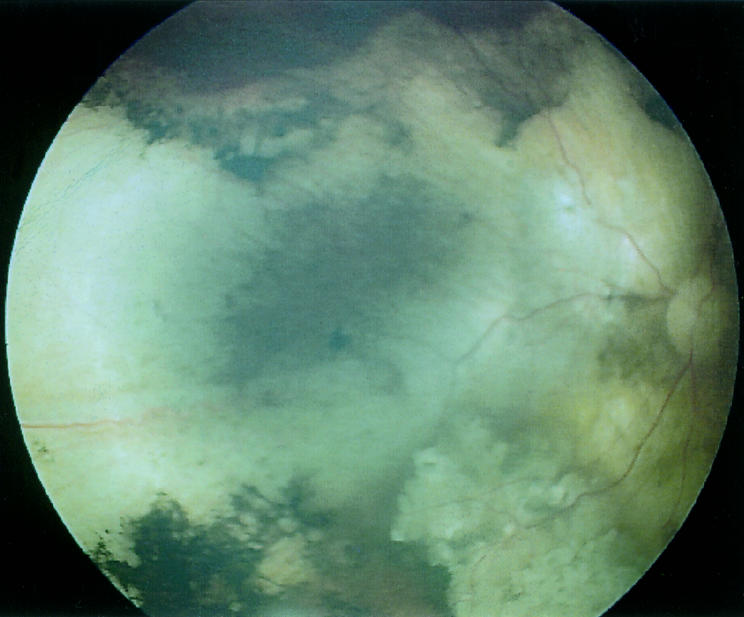
Fundus photograph of a 16 mm retinoblastoma tumour following treatment with chemotherapy. Note the dramatic reduction in size leaving a large atrophic scar.
Figure 2.
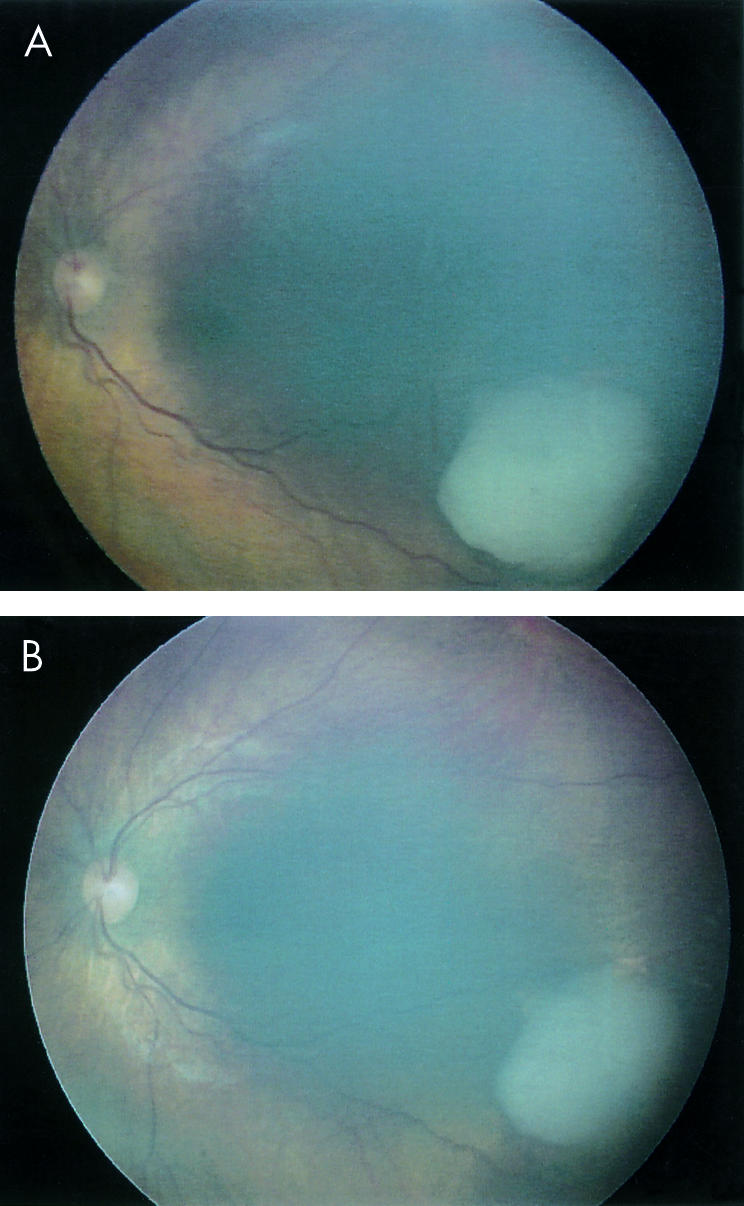
Fundus photographs of a 4.5 mm tumour showing minimal response following administration of chemotherapy. (A) Demonstrates the appearance at diagnosis and (B) 4 months after treatment.
We divided the retina into three easily identifiable zones progressing from the posterior pole anteriorly. Macular tumours were found to have the highest success rates with 26 of 31 tumours (84 %) responding (p<0.060). Tumours in the equatorial and anterior ora zones had serially lower success rates with 26 of 39 (67 %) and four of eight (50%) tumours responding (Fig 3). The higher response rate observed with macular tumours is not entirely unexpected. The disproportionate choroidal blood flow supplied by the short posterior ciliary vessels probably contributes to increased drug delivery to this area. We suspect that macular tumours receive higher concentrations of chemotherapy and therefore respond better to this treatment. Clinically this finding suggests that a majority of tumours in the macula can be cured by chemotherapy alone without the need for adjuvant diode laser hyperthermia. In our centre we prefer not to use thermotherapy for tumours within the macula in order to preserve the best possible visual outcome for the patient. Adjuvant or alternative treatment for macular tumours is given only after chemotherapy has failed. Many of the small peripheral tumours reviewed for this study were treated initially with cryotherapy and were therefore excluded. We suspect this is why our sample size of anterior peripheral tumours was limited to eight. Although it is difficult to draw conclusions from such a small group of tumours it is interesting to note that four of them (50%) failed therapy.
Figure 3.
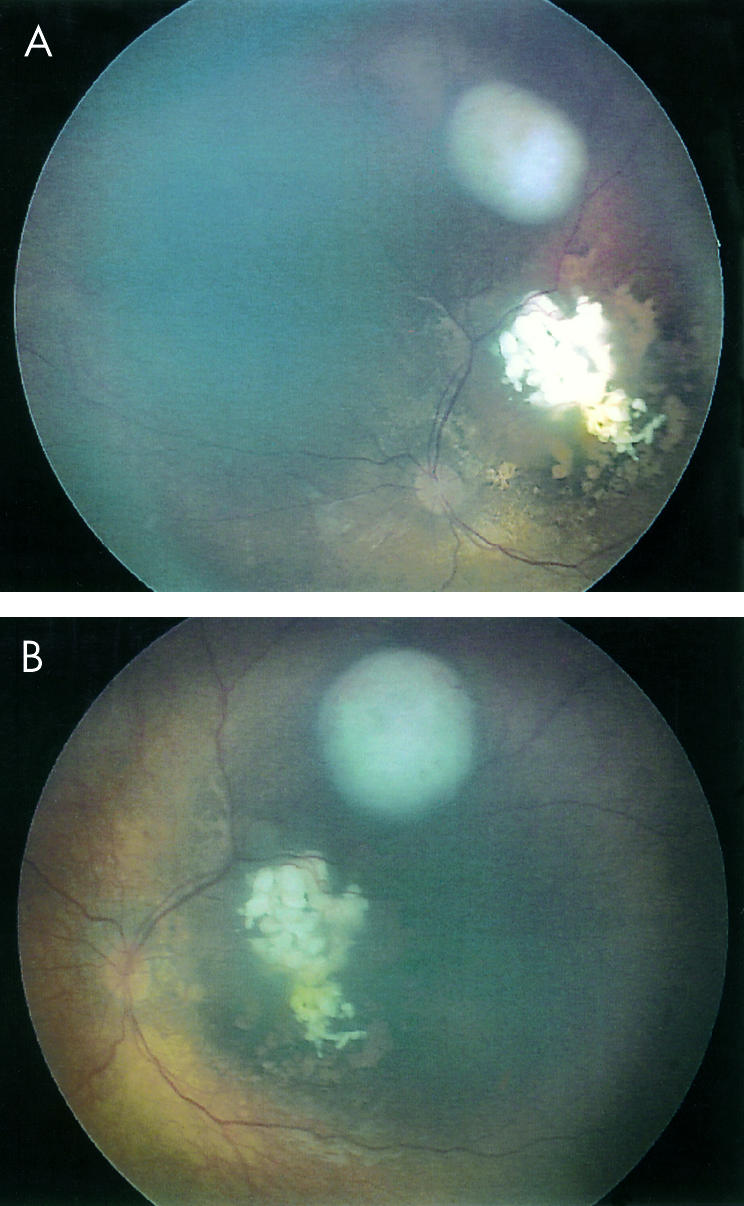
Fundus photographs (A, B) demonstrating the successful response of a macular tumour to chemotherapy with an adjacent extramacular lesion failing treatment and continuing to grow.
Tumour burden is an important parameter in the staging of a majority of cancers. As it increases response to many therapeutic treatments including chemotherapy often declines. In order to assess how this variable affects response rates in retinoblastoma we evaluated the relation between tumour size at diagnosis and outcome. Estimates of the largest basal tumour dimension were made by one ophthalmologist (JLH) using indirect ophthalmoscopy. This approach has been used in other studies and is based upon the optical principles of image size observed through a 20 dioptre lens.14 We felt it was the most reliable and reproducible method of assessing tumour dimension. While ultrasonography is a useful adjunct, very small and peripheral tumours can be difficult to assess using this approach; measurements can vary greatly depending upon the positioning and angle of the probe. In our study basal tumour dimensions ranged in size from 0.25 mm to 17 mm with a mean of 6.6 mm. We found the response rates among the majority of intraocular tumours did not differ in relation to size. Large and medium tumours (those greater than 2 mm) did not have a worse outcome.
For the clinician, these results are particularly relevant in the setting of asymmetrically staged bilateral retinoblastoma. Years ago patients who presented with advanced retinoblastoma in one eye and smaller tumours in the contralateral eye were treated with radiotherapy and enucleation (of the worse eye). Today we defer enucleation and assess tumour response in both eyes after giving chemotherapy. Our data suggest that this approach is reasonable even in the setting of very large tumours. In this study tumours with basal dimensions as large as 16 mm responded to chemotherapy alone. We have observed cases where eyes with large advanced tumours were cured by chemotherapy whereas contralateral eyes with smaller tumours failed all modalities and succumbed to enucleation.
The response of small tumours, those less than or equal to 2 mm in size, is less clear. A univariate logistic analysis suggested that they were less responsive to chemotherapy than larger ones. Among 18 tumour foci less than or equal to 2 mm, eight (44%) failed chemotherapy. This compares with 14 of 60 (23%) tumours greater than 2 mm in size failing to respond (p <0.088). Further analysis, however, revealed that age was a confounding variable and associated both with tumour size and outcome. To assess whether size less than or equal to 2 mm was independently predictive of outcome we constructed a bivariate logistic model that included age. In this analysis the significance of tumour size declined (p <0.199) but remained suggestive given our sample size. We can only conclude therefore that small retinoblastoma foci (less than or equal to 2 mm in basal dimension) may have a worse response to chemotherapy than larger tumours. Vascular perfusion and drug delivery may be reduced in very small tumours resulting in chemoresistance and continued growth. Careful and more frequent assessment of these lesions seems prudent given our results.
An unexpected finding of our study was the poor response of tumours diagnosed in very young patients. Eight tumours were diagnosed in six patients (six eyes) less than 2 months of age. Five (63%) failed to respond to chemotherapy alone and required additional treatment. Although there were only eight tumours diagnosed at less than 2 months of age this variable correlated strongly with outcome (p <0.032). We reviewed the chemotherapeutic regimen given to these patients and confirmed that doses were not altered for patients in this age group. These tumours ranged in size from 0.25 mm to 12 mm with a mean of 5.8 mm; four were located in the macula, three in the equatorial zone, and one anteriorly. Given the small sample size these results may reflect a statistical aberration of the data. Alternatively, tumour biology and drug absorption may differ in this age group. If these results accurately reflect clinical response rates, it suggests that chemotherapy alone may not be the preferred approach for tumours diagnosed at less than 2 months of age. Certainly, external beam radiotherapy would be discouraged in these children, as they are prone to severe orbital deformity and increased second tumour risk.15 These lesions may have a better response with adjuvant therapy, such as diode laser hyperthermia, or more traditional approaches, such as plaque radiotherapy. Altering chemotherapy protocols and dosing regimens is another consideration. The results certainly suggest the need for further research in the use of chemotherapy in this age group.
The relapse time of tumours failing treatment was also reviewed in this study. Failure to respond to chemotherapy occurred 2–25 months following treatment (mean 10.8 months). The vast majority of tumours that relapsed, 18 of 22 (82 %) did so by 12 months. These data serve to emphasise the importance of careful and frequent assessment of all retinoblastoma foci treated by chemotherapy alone, especially in the first year following treatment. Use of a fundus digital imaging system can be helpful in assessing these tumours through serial photographic comparison.
The management of retinoblastoma has evolved over the past decade through the advances of a number of techniques including chemotherapy and diode laser hyperthermia. None the less there remain a number of patients who do not respond to this approach. For them, traditional methods such as plaque radiotherapy, cryotherapy, and external beam radiotherapy are necessary. By identifying patients prone to chemotherapeutic failure we may be able to offer alternative or adjuvant treatment initially at diagnosis. Our study is unique in its sample of tumours treated with chemotherapy alone and serially followed for their response or failure. Certain factors can now be considered before initiating chemotherapy. We have identified the macula as a preferential site of successful tumour response. The majority of tumour foci irrespective of basal size were found to respond equally to chemotherapy, with only the smallest of tumours suggestive of having a poor response. Finally, tumours diagnosed at less than 2 months of age were also shown to have a poor response to chemotherapy. By considering these findings the clinician can use chemotherapy in a selective fashion, in concert with other treatments thereby improving patient survival and lowering ocular morbidity.
Acknowledgments
We gratefully acknowledge the clerical assistance of Ms P Meelapsom, Ms G Chryssaanthopoulou, and Ms P Jackson. This research was funded in part by a grant from the Retinoblastoma Society UK (DSG).
REFERENCES
- 1.Chan HSL, Thorner PS, Haddad G, et al. Effect of chemotherapy on intraocular retinoblastoma. Int J Pediatr Hematol Oncol 1995;2:269–81. [Google Scholar]
- 2.Gallie BL, Budning A, DeBoer G, et al. Chemotherapy with focal therapy can cure intraocular retinoblastoma without radiation. Arch Ophthalmol 1996;114:1321–9. [DOI] [PubMed] [Google Scholar]
- 3.Greenwald MJ, Strauss LC. Treatment of intraocular retinoblastoma with carboplatin and etoposide chemotherapy. Ophthalmology 1996;103:1989–97. [DOI] [PubMed] [Google Scholar]
- 4.Kingston JE, Hungerford JL, Madreperla SA, et al. Results of combined chemotherapy and radiotherapy for advanced intraocular retinoblastoma. Arch Ophthalmol 1996;114:1339–43. [DOI] [PubMed] [Google Scholar]
- 5.Shields CL, De Potter P, Himelstein BP, et al. Chemoreduction in the initial management of intraocular retinoblastoma. Arch Ophthalmol 1996;114:1330–8. [DOI] [PubMed] [Google Scholar]
- 6.White L. Chemotherapy in retinoblastoma: current status and future directions. Am Ped Hematol Oncol 1991;13:189–201. [PubMed] [Google Scholar]
- 7.Bornfeld N, Schuler A, Bechrakis N, et al. Preliminary results of primary chemotherapy in retinoblastoma. Klin Pediatr 1997;209:216–21. [DOI] [PubMed] [Google Scholar]
- 8.Levy C, Doz F, Quintana E, et al. Role of chemotherapy alone or in combination with hyperthermia in the primary treatment of intraocular retinoblastoma: preliminary results. Br J Ophthalmol 1998;82:1154–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman DL, Himelstein B, Shields CL, et al. Chemoreduction and local ophthalmic therapy for intraocular retinoblastoma. J Clin Oncol 2000;18:12–7. [DOI] [PubMed] [Google Scholar]
- 10.Murphree AL, Villablanca JG, et al. Chemotherapy plus local treatment in the management of intraocular retinoblastoma. Arch Ophthalmol 1996;114:1348–56. [DOI] [PubMed] [Google Scholar]
- 11.Shields CL, Shields JA, Needle M, et al. Combined chemoreduction and adjuvant treatment for intraocular retinoblastoma. Ophthalmology 1997;104:2101–11. [DOI] [PubMed] [Google Scholar]
- 12.Beck MN, Balmer A, Dessing C, et al. First-line chemotherapy with local treatment can prevent external-beam irradiation and enucleation in low-stage intraocular retinoblastoma. J Clin Oncol 2000;18:2881–7. [DOI] [PubMed] [Google Scholar]
- 13.Gunduz K, Shields CL, Shields JA, et al. The outcome of chemoreduction treatment in patients with Reese-Ellsworth group V retinoblastoma. Arch Ophthalmol 1998;116:1613–7. [DOI] [PubMed] [Google Scholar]
- 14.Shields CL, Santos MC, Diniz W, et al. Thermotherapy for retinoblastoma. Arch Ophthalmol 1999;117:885–93. [DOI] [PubMed] [Google Scholar]
- 15.Abramson DH, Frank CM. Second nonocular tumors in survivors of bilateral retinoblastoma; a possible age effect on radiation-related risk. Ophthalmology 1998;105:573–9. [DOI] [PubMed] [Google Scholar]


