Abstract
Aim: To describe vitreoretinal surgical services in 1998 in 12 eastern European countries and to identify ways for their further improvement.
Methods: All inpatient eye departments in the 12 countries received a standardised questionnaire; the data obtained were processed at the international study coordinating centre in Prague.
Results: All 458 eye departments in the region were involved. The number of retinal detachments treated by extraocular surgery, or pars plana vitrectomy, per one million inhabitants respectively, were as follows: Belarus (52; 6), Federation of Bosnia and Herzegovina (21; 2), Bulgaria (39; 19), the Czech Republic (78; 40), Estonia (60; 17), Hungary (81; 88), Latvia (82; 36), Lithuania (68; 6), Trans-Dniester Region of Moldova (6; –), Poland (70; data not available), Romania (24; 25), and Slovakia (67; 55). The number of people per one retinal laser was assessed (in millions): Belarus (1.26), Federation of Bosnia and Herzegovina (2.23), Bulgaria (0.59), the Czech Republic (0.22), Estonia (0.24), Hungary (0.23), Latvia (0.41), Lithuania (0.62), Poland (0.36), Romania (2.25), and Slovakia (0.14).
Conclusions: Conditions for posterior eye segment surgery in the central and eastern European region vary substantially. Underserved regions require (1) more eye doctors trained in surgical and laser retinal treatment; (2) improvement in screening for diabetic eye complications and retinopathy of prematurity; (3) technical equipment for places in need.
Keywords: diabetic retinopathy, retinopathy of prematurity, retinal detachment, eastern Europe
An evaluation of the affordability and availability of eye healthcare services for posterior eye disorders was conducted to analyse the current status and to identify the ways to enhance their further development. Attention was primarily aimed at eye healthcare services in potentially preventable and treatable conditions of visual disability in the region, diabetic retinopathy in adults, and retinopathy of prematurity in children. The appropriate preventive measures and adequate treatment may dramatically reduce the magnitude of visual impairment in the population of a given country or region. The outcome of this study provided essential information for the development of national prevention of blindness strategies in the framework of the global initiative “Vision 2020—the right to sight.”1
SUBJECT AND METHODS
Representatives of national societies of ophthalmology from 12 eastern European countries joined an international study group. They included Belarus, Federation of Bosnia and Herzegovina, Bulgaria, the Czech Republic, Estonia, Hungary, Latvia, Lithuania, Trans-Dniester Region of Moldova, Poland, Romania, and Slovakia. Standardised questionnaires were distributed among all inpatient eye departments, and further information was collected by personal visits and inquiries. Data from participating countries were processed by the international coordinating centre in Prague.
RESULTS
All 458 eye departments (70 university and 388 non-university inpatient departments) located in the 12 participating countries were involved in the study. The response rate was 100%, except for Romania (93%) and Bulgaria (93%). The non-participating eye departments in these two countries were surgically inactive.
Vitreoretinal surgery
Vitreoretinal surgeons were considered eye surgeons providing independent surgeries for retinal detachment by both extraocular techniques, and/or pars plana vitrectomies. On average, there were two to three vitreoretinal surgeons per one million inhabitants except for Belarus, Federation of Bosnia and Herzegovina, and Romania, where the number of inhabitants per one vitreoretinal surgeon exceeded one million. The ophthalmologists trained in vitreoretinal surgery represented only 7% (270) from the total number of inpatient ophthalmologists involved in this study (3851). The eye departments providing vitreoretinal surgery were mostly attached to the main universities in the country. Fifty eight per cent of retinal eye surgeons were based at university eye departments; in the Federation of Bosnia and Herzegovina, Latvia, Lithuania, and Trans-Dniester Region of Moldova there were no vitreoretinal surgeons working at non-university eye departments.
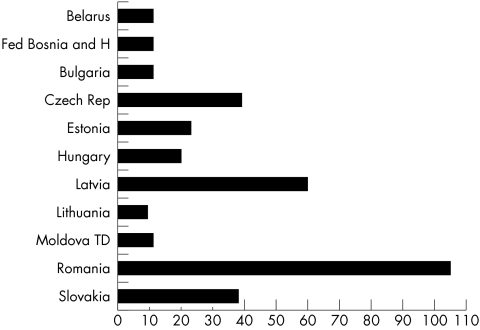
The workload of vitreoretinal surgeons was analysed. The number of pars plana vitrectomies performed by one vitreoretinal surgeon in 1998 was as follows: Belarus (11), Federation of Bosnia and Herzegovina (11), Bulgaria (11), the Czech Republic (39), Estonia (23), Hungary (20), Latvia (60), Lithuania (9), Trans-Dniester Region of Moldova (11), Romania (105), and Slovakia (38) (Fig 1).
Figure 1.
Average number of pars plana vitrectomies performed by one vitreoretinal surgeon in 1998.
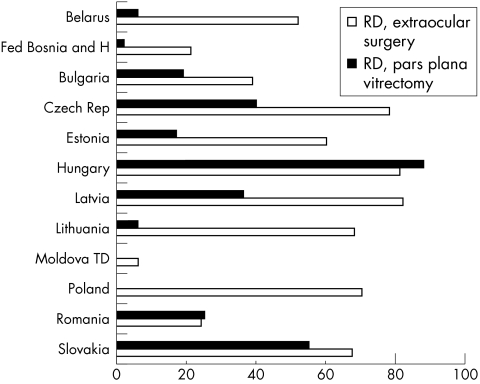
The number of retinal detachments treated by extraocular surgery, or pars plana vitrectomy, per one million inhabitants respectively, was as follows: Belarus (52; 6), Federation of Bosnia and Herzegovina (21; 2), Bulgaria (39; 19), Czech Republic (78; 40), Estonia (60; 17), Hungary (81; 88), Latvia (82; 36), Lithuania (68; 6), Trans-Dniester Region of Moldova (6; –), Poland (70; data not available), Romania (24; 25), and Slovakia (67; 55) (Fig 2).
Figure 2.
Retinal detachment-extraocular surgeries and pars plana vitrectomies performed per one million inhabitants in 1998. (Poland, data on pars plana vitrectomies performed exclusively for retinal detachments are not available, Trans-Dniester Moldova, no pars plana vitrectomies performed.)
Diabetic retinopathy
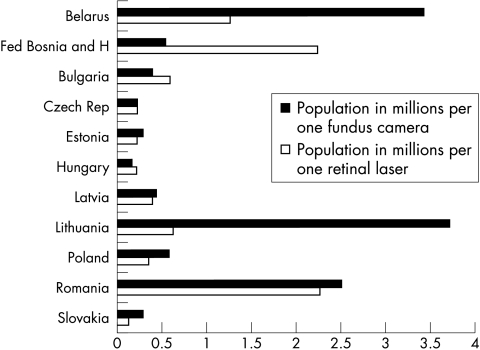
Patients with diabetes mellitus were referred for their eye examinations mostly by general practitioners and internal medicine specialists. The availability of fundus cameras for colour eye fundus photographs and fluorescein angiography was evaluated, and the number of inhabitants per one fundus camera was calculated (in millions): Belarus (3.4), Federation of Bosnia and Herzegovina (0.56), Bulgaria (0.41), Czech Republic (0.22), Estonia (0.29), Hungary (0.18), Latvia (0.49), Lithuania (3.70), Poland (0.57), Trans-Dniester Region of Moldova (no fundus camera), Romania (2.50), and Slovakia (0.30). This indicates, for example, that in the Federation of Bosnia and Herzegovina and in Poland there were more than half a million inhabitants per one fundus camera, while in Romania it was two and a half million, and in Belarus and Lithuania, it was more than three million (Fig 3).
Figure 3.
Number of inhabitants in millions per one laser for retinal photocoagulation and one fundus camera in 1998.
The availability of laser treatment for diabetic eye complications was assessed. The number of people per one retinal laser was as follows (in millions): Belarus (1.26), Federation of Bosnia and Herzegovina (2.23), Bulgaria (0.59), the Czech Republic (0.22), Estonia (0.24), Hungary (0.23), Latvia (0.41), Lithuania (0.62), Poland (0.36), Romania (2.25) and Slovakia (0.14) (Fig 3).
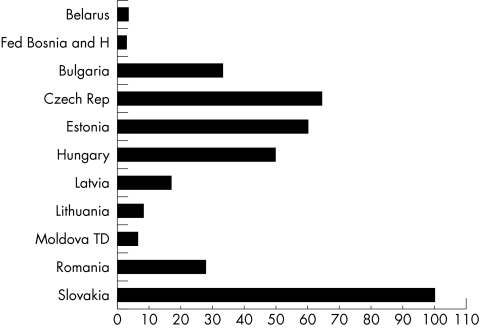
The availability and utilisation of vitreoretinal surgical services for patients with advanced stages of diabetic eye complications were analysed. The average number of pars plana vitrectomies for advanced diabetic eye complications performed per one million inhabitants were calculated: Belarus (4), Federation of Bosnia and Herzegovina (3), Bulgaria (33), Czech Republic (64), Estonia (60), Hungary (50), Latvia (17), Lithuania (8), Trans-Dniester Region of Moldova (6), Romania (28) and Slovakia (100) (Fig 4).
Figure 4.
Diabetes mellitus eye complications, total number of pars plana vitrectomies per one million inhabitants in 1998.
Retinopathy of prematurity
The majority of ophthalmologists are familiar with the internationally accepted rules for screening of low birthweight babies for retinopathy of prematurity (ROP). The implementation of screening programmes and availability of treatment for advanced stages of this condition, however, differ substantially from country to country. In the Czech Republic, Estonia, Hungary, Latvia, Lithuania, Poland, and Slovakia suggestions for national ROP screening have been introduced and/or published in their medical literature. Both retinopexy and laser treatment are available for babies in need. In Romania, screening for ROP in the capital city district was introduced in 1998; in that year there was no diode laser treatment available. In Belarus, Bulgaria, Federation of Bosnia and Herzegovina, and Trans-Dniester Region of Moldova there was no laser treatment for ROP available in 1998.
DISCUSSION
Remarkable differences in surgical services for patients with vitreoretinal diseases were observed in eastern European countries.
On average there were 31 pars plana vitrectomies performed by one vitreoretinal surgeon in eastern Europe in 1998. There are certainly several reasons for the rather low utilisation of the surgical skills of these surgeons. Firstly, vitreoretinal surgery needs properly equipped operating theatres with operating microscopes, vitrectomes, and consumables. Severe economic restrictions on healthcare systems in some eastern European countries and the frequent inability of patients to contribute to the cost of their surgery, keep the number of surgeries low. Secondly, as some surgeons perform rather low numbers of operations per year; this lack of experience may cause unsatisfactory results and/or a higher rate of reoperations. This may discourage patients considering their operation. Thirdly, in some countries, the availability of vitreoretinal surgical treatment remains limited to the capital and large cities. This may restrict many patients’ awareness of this way of treatment as well as their actual access to it.
Diabetic retinopathy is among the leading causes of blindness in adults worldwide, particularly in industrialised countries, and middle income countries of eastern Europe.2 In the majority of patients, diabetic eye complications may be preventable and treatable. There is apparently a lack of systematic screening for eye complications in diabetes in some countries of eastern Europe, particularly in the early stages of this disease. The introduction of comprehensive national disease control programmes for diabetic retinopathy in eastern Europe is highly advisable. The development of national strategies to control diabetic retinopathy is one of the main priorities for reducing the magnitude of visual disability in the region.
Similarly, retinopathy of prematurity is among the leading causes of blindness in children in eastern Europe.3,4 While the highly industrialised countries experienced a dramatic decline in the incidence of ROP, it increased in some of the middle income countries. There may be two scenarios for this. The more economically successful eastern European countries with developed perinatal care may have experienced an increase in the incidence of ROP because of higher numbers of surviving babies with extremely low birth weight. Other eastern European countries may have experienced a similar increase in ROP cases in prematurely born children because of their gradual introduction and improvement of neonatal care. Both groups will require well implemented and organised screening for ROP in babies at risk, needing a sufficient number of trained ophthalmologists and the appropriate equipment for diagnostics and treatment of advanced cases.
In several countries of eastern Europe, three main limitations to vitreoretinal surgical services provided may be identified: lack of skills and experience of healthcare personnel, inadequate technical equipment, and insufficient awareness of the public.
CONCLUSIONS AND RECOMMENDATIONS
An evaluation of the availability of surgical services for posterior segment eye diseases in 12 eastern European countries as of 1998 was undertaken. Conditions for posterior eye segment surgery in the central and eastern European region vary substantially. The main requirements for improving eye care for posterior segment eye diseases were identified as follows:
There is a need for “hands-on” skills transfer and education for many ophthalmologists who are involved in posterior segment eye surgery in eastern Europe. Short term teaching visits by experienced vitreoretinal surgeons and retinal specialists, particularly to non-university vitreoretinal centres, should enhance the experience and knowledge of surgeons in need.
There is an urgent need for basic equipment for some regions (for example, lasers for retinal photocoagulation, surgical instruments, indirect ophthalmoscopes, etc) to sufficiently implement preventive and therapeutical measures.
National healthcare authorities and policymakers should evaluate the requirements for improving the screening for diabetic retinopathy, and retinopathy of prematurity, as well as for the even distribution of the necessary diagnostic and therapeutical equipment in their countries.
An awareness of potential conditions leading to blindness and the means of prevention must be strongly disseminated to the public.
Acknowledgments
This work was sponsored by Christoffel-Blindenmission. We gratefully acknowledge the assistance of Professor Dr med Volker Klauss, and Mr T ffytche, LVO FRCS FRCOphth, and the contribution of all members of the international study group.
INTERNATIONAL STUDY GROUP Ü Aamer (Estonia), T A Birich (Belorus), B Cârstocea, D F Şelaru (Romania), A ernák (Slovakia), V Jašinskas (Lithuania), G Laganovska (Latvia), J Németh (Hungary), V Novac (Moldova), M Sefić (Bosnia and Herzegovina), J Szaflik, J Kałužny (Poland), P Vassileva (Bulgaria).
REFERENCES
- 1.Vision 2020—the right to sight. www.iapb.org
- 2.Hamilton AMP, Ulbig MW, Polkinghorne P. Management of diabetic retinopathy. London: BMJ Publishing Group, 1996:1–15.
- 3.Gilbert CE, Rahi J, Eckstein M, et al. Retinopathy of prematurity in middle-income countries. Lancet 1997;9070:12–14. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Preventing blindness in children. Report of WHO/IAPB scientific meeting. Hyderabad, India, 13–17 April 1999. Geneva: WHO, 2000.