Abstract
Background/aims: The relative frequency, basic patient data, results, and complications of planned same day bilateral phacoemulsification were studied from April 1999 to May 2001 at the Department of Ophthalmology, Linköping University Hospital, Sweden.
Methods: Retrospective study of patient records (n=220) regarding preoperative and postoperative visual acuity, applied indications, concurrent disease, preoperative, peroperative, and postoperative complications, and number of unplanned postoperative visits. The monthly rate of bilateral phacoemulsification to all cataract procedures was monitored.
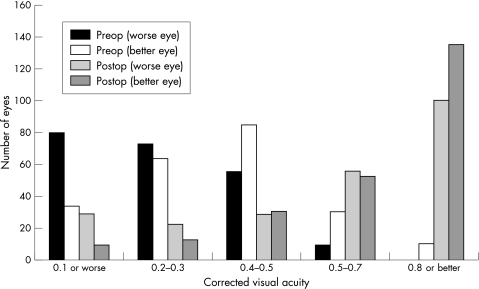
Results: Mean corrected preoperative visual acuity was 0.27 (worse eye) and 0.39 (better eye), and postoperatively (all eyes) 0.71. Visual acuity was 0.5 or better in 78% of eyes. Preoperative considerations included type of cataract, to avoid anisometropia, social circumstances, and concurrent eye disease. Reasons for unplanned postoperative visits included secondary cataract (n=10), iritis (n=6), corneal oedema (n=3), cortex in the anterior chamber (n=2), and unilateral endophthalmitis (n=2). During the study period, 10.5% of patients were operated upon bilaterally on the same day.
Conclusions: Same day bilateral phacoemulsification was found to be a safe and cost effective way of rapidly rehabilitating selected cataract patients. The patient must be informed of the added potential risks as well as the benefits of the procedure.
Keywords: cataract surgery, phacoemulsification, day case surgery
During recent decades, the development of cataract surgery has reduced complication rates and improved results. Patients who are aware that safe and effective treatment is available are unwilling to suffer problems caused by lens opacities. Increasing numbers of cataract operations have not met the demands, and the number of patients waiting for surgery is thus increasing even faster.1
Traditionally, cataract is operated on in one eye at a time. However, it has long been accepted that bilateral paediatric cataract may, for both general and ophthalmological reasons, be operated on in both eyes during a single general anaesthesia. The same applies to poorly cooperating patients with bilateral cataract. “Simultaneous” bilateral cataract surgery has also been used in the protocol of various studies.2,3 Terminologically, we prefer “same day bilateral cataract surgery” to “simultaneous bilateral cataract surgery.” In this paper “bilateral surgery/phacoemulsification” will be used synonymously.
Regular day case bilateral cataract surgery is not yet a routine everywhere. Beatty et al studied results and complications after bilateral extracapsular surgery.4 Although they considered bilateral surgery “a useful option,” they recommended it only for patients with poor general health who were operated upon under general anaesthesia, where the visual prognosis in both eyes was uncertain and both eyes were therefore considered to be in need of surgery. Others have suggested bilateral surgery in selected cases with fewer restrictions.5–7 Koch studied the timing of second eye surgery, stressing that modern methods reduce morbidity so far that cataract surgery can easily be performed only days or weeks apart with few medical, social, or economic disadvantages and without the risks associated with simultaneous surgery.8 In our general healthcare system, priority for cataract surgery is principally based on the visual acuity of the patient‘s better eye. In consequence, a successful monocular operation may lower the patient‘s priority for second eye surgery, which may be delayed for months or even years. In recent years, bilateral phacoemulsification has become standard practice at several Swedish ophthalmological centres.
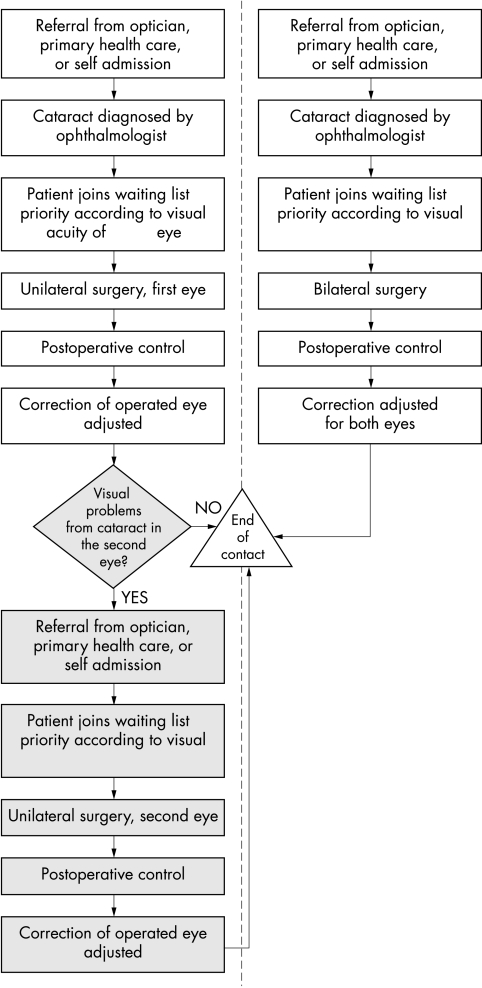
The delay in second eye surgery is also recognised within the British healthcare system.9 The cataract progresses while the patient is on the waiting list,10 which may make surgery technically more challenging. It is also well known that patients complain that the cataract in the unoperated eye “fogs the clear eye.” A moderate cataract in the unoperated eye may be even more annoying than a dense cataract. The benefits of second eye surgery have been shown in follow up quality of life studies, where patients did not report satisfaction until both eyes were rehabilitated.11,12 Rapid rehabilitation is especially desirable for the professionally active patient. However, elderly patients are also eager to attain good binocular vision quickly—for example, because of the need to drive a car, or because they are responsible for the care of a relative. The economic incentive for bilateral cataract surgery on the same day is obvious in a public healthcare system funded through taxes. Processing for surgery and postoperative controls will also be more efficient (Fig 1).
Figure 1.
Flow chart describing the pathway of cataract patients operated upon in one eye at a time (left pathway), compared with patients undergoing bilateral phacoemulsification (right pathway). The shaded steps of the left pathway show not only increased costs for managing a patient with bilateral cataract, but also the increased time that the patient will spend suffering from unsatisfactory vision. Note also that bilateral surgery results in less cost and effort in informing and preparing the patient, compared to operating on one eye at a time.
Bilateral surgery means that the patient is faced with the risk of a bilateral postoperative complication. Postoperative endophthalmitis is the most obvious and ominous example, but corneal oedema caused by endothelial decompensation has also been described.13 Retinal complications such as cystoid macular oedema, retinal breaks and detachments should also be borne in mind, especially when diabetics or myopes are operated. Furthermore, errors in preoperative lens power calculation may cause problems if both eyes are operated on the same day.
In 1998, same day bilateral phacoemulsification was used at our clinic in a study of multifocal intraocular lenses. The waiting time for cataract surgery at that time was long, especially for the second eye, and in some cases was more than 2 years. During the 1990s, phacoemulsification became the standard method, with topical anaesthesia being employed. Surgery results improved steadily, complication rates decreased and the number of operations per day increased. In order to meet the demands from the patients and at the same time simplify the process in the operating unit, bilateral phacoemulsification was introduced in the regular cataract process, beginning in April 1999. Initial results from the first 27 cases were encouraging.14
Here, we report retrospectively on the outcomes of planned bilateral phacoemulsification at the Department of Ophthalmology, Linköping University Hospital, Sweden between April 1999 and May 2001. The aim was to study (1) age and sex distribution in comparison with patients who had undergone monocular surgery, (2) the reasons for which bilateral surgery was performed, (3) the ratio between the number of patients operated upon bilaterally on the same day and the number who underwent monocular surgery during the study period, and (4) results and complications.
PATIENTS AND METHODS
The records of all patients (n=220) scheduled for bilateral phacoemulsification between April 1999 and May 2001 were reviewed retrospectively. Both the computer based system for registration and follow up of cataract patients and the manually kept operations register served as primary data sources. Parameters studied were preoperative and postoperative visual acuity tested with the Snellen chart, recorded indications for bilateral surgery, preoperatively recorded concurrent eye disease or general health problems, peroperative and postoperative complications, and unplanned visits related to the cataract operation. The proportion of patients undergoing bilateral phacoemulsification was monitored. Data were collected during July and August 2001.
All but three patients were operated upon by the authors (BJ, n=104; BL, n=113). Usually, the patient visited the surgeon once before the operation, and one postoperative visit was planned between 1 and 21 days after surgery. Patients who were considered suitable for and/or who expressed an interest in bilateral surgery were informed about the option and the risks and benefits involved. If the patient was eligible and consented, two operations were scheduled for the same day, usually with another case in between. A few disabled patients remained in the operating theatre while all equipment was changed for the second procedure. (After the study period we have changed the routine at our centre so that now the second operation is planned immediately after the first one.) Patients and surgeons had the possibility to change their mind and decline the second operation after the first was completed. The standard procedure was phacoemulsification with topical anaesthesia, corneal incision, and implantation of a foldable silicone or acrylic lens, and no suture. Sedatives were not given unless called for by the patient. When requested, diazepam 5 mg orally was given 1 hour preoperatively. Infection prophylactic routines consisted of rinsing the conjunctival sac of the eye to be operated on with sterile physiological saline solution. The upper half of the face was swabbed with chlorhexidine-alcohol solution. Gentamicin 0.1% solution was dropped in the eye once before and once after drape and blepharostat was placed, and again once at conclusion of surgery after drape and blepharostat had been removed. No antibiotics were added to the irrigation fluid. Topical dexamethasone was used 2–3 weeks postoperatively. At the postoperative visit, patients were advised about the need for adjustment of their spectacles after cessation of the steroids.
Table 1 lists the indications and contraindications for bilateral surgery. Bilateral cataract should be considered an absolute prerequisite for bilateral surgery and patient uncertainty an absolute contraindication.
Table 1.
| Reasons for suggesting bilateral phacoemulsification: |
| Significantly disturbing cataract in both eyes (cataract in the second eye expected to cause glare or binocular problems if left unoperated) |
| Reasons for speeding up visual rehabilitation: concurrent ophthalmic or general pathology, social situation |
| Unilateral surgery would result in postoperative anisometropia |
| Reasons for deferring bilateral phacoemulsification: |
| Patient uninterested or uncertain |
| Quality of postoperative care uncertain |
| Pathology of eye or its adnexa or general health problem with increased risk of complications |
| Significant difference in the density of the cataract |
| Increased risk for deviation from calculated postoperative refraction—eg, previous refractive corneal surgery, very short or long axial lengths or extreme or irregular corneal curvatures |
| Complication at first operation |
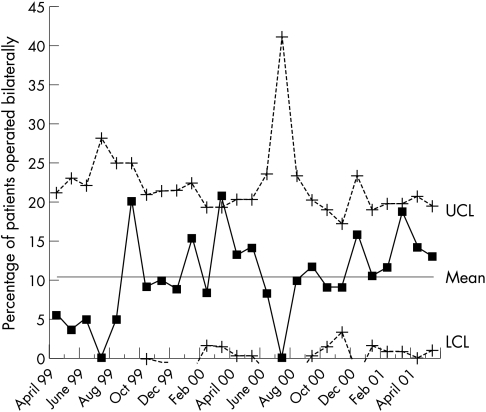
Statistical process control tools were used to monitor the ratio of patients planned for bilateral phacoemulsification.15 A control chart was constructed, showing the percentage of patients each month who were operated upon bilaterally. The percentage was calculated as the number of bilaterally operated patients divided by the total number of patients operated upon by BJ and BL. The variation coefficient for each data point, σi, is calculated as
√p(1 − p)/niwhere p is the overall process average, and ni is the total number of observations (patients who underwent monocular surgery plus patients who underwent bilateral surgery) for each data point. Upper (UCL) and lower (LCL) control limits are calculated as p ± 3(σi). Whereas most variations within the interval between UCL and LCL are considered non-significant (common cause variation), a point that falls outside the control limits is considered a special cause—that is, interest should be directed to this point to determine what may have caused the variation.
RESULTS
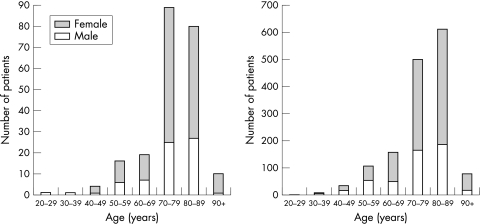
The distributions of sex and age of patients planned for bilateral phacoemulsification are depicted in Figure 2. Sixty nine (31.4%) were male and 151 (68.6%) female. The mean age was 76.3 years, (females 76.9, males 75.0); 81.4% were aged 70 or older. Corresponding figures for those operated upon monocularly during the study period are males 33.2%, females 66.8%, mean age 76.2 years (females 77.1, males 74.4), and 79.5% aged 70 or older.
Figure 2.
Left: The distribution of age and sex of 220 patients planned for bilateral phacoemulsification—68.6% were female, 31.4% male. Right: The distribution of age and sex of the 1499 patients operated upon monocularly for cataract during the study period by the participating surgeons—66.8% were female, 33.2% male.
Indications for bilateral phacoemulsification recorded at the preoperative visit are presented in Table 2. Note that “concurrent eye disease” can be a reason either for proposing or deferring bilateral surgery, depending on the situation, cf Table 3. More than one indication was recorded for 51 patients. The type of cataract in the second eye was the most commonly recorded reason at the preoperative visit. Two patients asked for bilateral surgery because they were afraid of the procedure and wanted to get it over with as quickly as possible. In 35 cases, the preoperative finding of bilateral cataract was the only recorded reason for choosing bilateral surgery.
Table 2.
| Recorded reasons for suggesting bilateral phacoemulsification | Found in number of records (n=220) |
| Cataract in second eye that with a high level of probability will cause the patient to request operation | 111 (50.2%) |
| Expected refraction problems (anisometropia) as a consequence of unilateral surgery | 37 (16.7%) |
| Concurrent eye disease (eg, AMD, glaucomatous optic damage, occlusion of retinal vessels) | 43 (19.4%) |
| General condition (eg, balance problems) | 20 (9.0%) |
| Problems in pursuing occupation | 8 (3.6%) |
| Other aspects of social situation (eg, living conditions, dependence on car driving) | 36 (16.3%) |
| Fear of operation | 2 (0.9%) |
| Preoperative finding of bilateral cataract only recorded reason | 35 (15.8%) |
Table 3.
| Ophthalmic pathology recorded preoperatively | Number of patients (n=220) |
| AMD | 53 (24.0%) |
| Diabetes | 14 (6.3%) |
| Glaucoma | 11 (5.0%) |
| Previous surgery | 4 (1.8%) |
| Endothelial dystrophy | 1 (0.5%) |
| Other ophthalmic pathology | 4 (1.8%) |
Figure 3 depicts month by month the ratio of patients undergoing bilateral phacoemulsification. The mean of the monthly ratios during the study period was 10.5%, and the median 10%. The total number of operations performed each month varies substantially, which in turn changes the UCL values. During the study period, there was no significant change in the percentage of patients who were scheduled for bilateral phacoemulsification.
Figure 3.
Percentage of patients undergoing bilateral surgery during the study period, monitored month by month. The graph is a control chart, used for monitoring process function over time. UCL = upper control limit. LCL = lower control limit (only values ≥0 are plotted). Overall mean percentage of bilaterally operated patients during the study period was 10.5%. The control chart does not suggest any significant shift in the process over time after the initial 5 months.
The mean preoperative best corrected visual acuity in the worse eye was 0.27 (median 0.2), and in the better eye 0.39 (median 0.4). Sixty one per cent of the patients had visual acuity <0.5 in the better eye. The mean corrected visual acuity at the final postoperative visit for all eyes operated upon was 0.71. It was ≥0.5 in 78%, ≥0.8 in 54%, and ≥1.0 in 34% of all eyes. The distributions of visual acuity before and after surgery, and in the worse and the better eye respectively, are shown in Figure 4.
Figure 4.
Distribution of corrected visual acuity (VA) before and after bilateral surgery, in the worse and better eye respectively. In the worse eye, preoperative mean VA was 0.27, and in the better eye 0.39. Postoperative mean VA for all operated eyes together was 0.71.
Table 3 lists concurrent eye disease and other factors considered as increasing the risk of per- and postoperative problems or potentially affecting postoperative visual acuity, recorded at the preoperative visit. Table 4 lists problems encountered during surgery, and Table 5 postoperative complications. In one case, the surgeon cancelled the second operation due to rupture of the posterior capsule and vitreous loss in the first eye. One patient declined the planned second operation after the first uncomplicated surgery was finished, because of general discomfort during the procedure. She later requested and underwent surgery on the second eye. With a few exceptions, complications had no consequences for the final result with regard to postoperative treatment or visual function. In one case with glaucoma, both pupils needed manual stretching with a pupil dilator. Five extra visits to follow up and treat elevated intraocular pressure, prolonged iritis, and posterior capsular opacification were needed, and the final corrected visual acuity was 1.0 and 0.9. One case, where pupil constriction in both eyes necessitated the use of iris hooks, had a unilateral local zonular dehiscence and postoperatively a small cortical remnant in the anterior chamber. The resolution of the cortex was monitored at one extra visit, and final corrected visual acuity was 0.9. Cortical remnants were also seen postoperatively in another case where iris hooks were used to dilate the pupil, but corrected visual acuity reached 1.0 after two extra visits. All cases of corneal oedema resolved within the standard steroid treatment period, 2–3 weeks, and they did not demand extra treatment such as osmotics. Unilateral endophthalmitis occurred in two cases: one where surgery had been complicated by iris prolapse (coagulase negative Staphylococcus aureus was cultured from aqueous), and the other after uneventful surgery in a patient with dementia (Bacillus cereus cultured from conjunctiva and Enterococcus faecalis from aqueous). In both cases, the eye that was infected had been operated as the second one. Useful vision was lost in the infected eyes, but the contralateral eye had no complications and both cases achieved improved vision.
Table 4.
| Problem encountered peroperatively | Number of operations (n=438) |
| Small or contracting pupil necessitating iris hooks | 20 (4.5%) |
| Small pupil necessitating pupil dilatator | 3 (0.7%) |
| Ruptured posterior capsule | 3 (0.7%) |
| Iris prolapse | 1 (0.2%) |
Table 5.
| Postoperative problems and complications | Number of patients (n=220) |
| Posterior capsule opacification | 10 (4.5%) |
| Prolonged postoperative iridocyclitis | 6 (2.7%) |
| Endophthalmitis (unilateral) | 2 (0.9%) |
| IOP elevation | 2 (0.9%) |
| Corneal oedema, unilateral | 2 (0.9%) |
| Cortex in anterior chamber | 2 (0.9%) |
| Floaters, halos | 2 (0.9%) |
| Miscellaneous | 2 (0.9%) |
| Cystoid macular oedema, bilateral | 1 (0.5%) |
| Corneal oedema, bilateral | 1 (0.5%) |
| Planned refraction not achieved | 1 (0.5%) |
Owing to complications, extra visits were necessary for 31 patients (14.1%), of whom 13 had one, 16 two or three, and two patients four or more extra visits. The rest (189 patients, 85.9%) attended only the one planned postoperative visit. During the study period, 86.9% of monocularly operated patients attended only the one planned postoperative visit.
DISCUSSION
Hypothetically, because of a more active life, younger patients might show a greater desire for the shortest possible rehabilitation. However, the mean age of bilaterally operated patients is not substantially different from that of our monocularly operated patients, or from that found in larger surveys of cataract patient populations.16,17 The fraction of patients aged 70 or more is 81%, both in our material and for all patients operated upon for cataract in Sweden during 1999.18 For binocularly operated patients, the group aged 70–79 is larger than the group aged 80–89, but vice versa for monocularly operated patients (Fig 2). Apart from that, the age distribution is similar for the two groups. Hypothetically, the “younger elderly” might be more active and more interested in the shorter rehabilitation time with bilateral same day surgery than the “elder elderly.”
The female preponderance in our material (68.8%) slightly exceeds that of our monocularly operated patients (66.8%) and is also larger than that found in a general cataract patient population, which in turn is larger than would be expected from the general female majority in the higher age groups.18 Lundström et al formulated three different hypotheses that could account for all or part of the sex differences in a cataract operated population.17 Since bilateral phacoemulsification is suggested only when the ophthalmologist finds bilateral cataract that is expected to cause problems for the patient if only one eye is operated upon, we consider the hypothesis of a higher cataract prevalence in women to best explain our figures.
The different recorded “non-cataract” indications for bilateral phacoemulsification seem fairly evenly distributed. Concurrent eye disease, such as macular degeneration or glaucoma, may of course speak in favour of bilateral surgery, since rehabilitation is quicker. The occasional uncertainty about which eye is best helped with surgery is also avoided. On the other hand, severe concurrent eye disease may also be a reason for deferring bilateral surgery. In case any postoperative problems appear, it is essential not only to have discussed thoroughly the reason(s) for bilateral surgery with the individual patient but also to record this discussion thoroughly. It should not be necessary to stress that economical factors never be used to motivate the patient for bilateral surgery. Admittedly, our patients did indeed “save” the fee for one operation and one postoperative visit (totalling approximately US$50/£35, the rest of the cost being covered by public insurance) but this was not discussed preoperatively. Only medical benefits and risks, social factors, and information about the expected waiting time for second eye surgery were discussed when deciding between unilateral and bilateral phacoemulsification.
The preoperative visual acuity in the better, usually the second operated, eye (mean 0.4) before bilateral surgery is lower than in the overall figures of the Swedish National Cataract Register, where the median visual acuity of the operated eye is 0.3, and of the better eye 0.6.18 Sixty one per cent of our patients had a visual acuity of less than 0.5 in the better eye, compared to 32.9% in the national register. This indicates that patients we considered suitable for bilateral surgery to a larger extent suffered from cataract of similar degree in both eyes, compared with those undergoing monocular cataract surgery. It should be borne in mind that the overall figures of the Swedish National Cataract Register include patients undergoing their second cataract operation. In 1999, 36.8% of cataract operations in Sweden were second eye operations.18
During the study period, the mean percentage of patients undergoing bilateral phacoemulsification was 10.5%, a figure that did not increase significantly with time. The operating programmes were not limited with respect to the number of patients the surgeon was able to plan for bilateral surgery. We conclude that as long as strict indications are followed, the majority of cataract patients will undergo monocular surgery.
The mean postoperative visual acuity after bilateral surgery (0.71) did not differ from that of patients operated upon monocularly during the study period.
The vast majority of patients did not need any extra visits postoperatively. We did not detect any extra visits necessitated by the bilateral surgery per se. Most complications encountered in the study (corneal oedema, cystoid macular oedema, iritis, etc) resolved with treatment over time and did not result in visual loss.
Two cases of endophthalmitis suffered monocular visual loss as a consequence of the operation. It was noted that one of these patients expressed great satisfaction that both eyes had been operated upon, stating “Otherwise, I would have been severely disabled through poor vision [if only one eye had been operated upon and become infected].”
Both unilateral and bilateral endophthalmitis after bilateral surgery have been described earlier.4,19 At the same time as we encountered the second unilateral case of endophthalmitis, the perioperative infection prophylactic routine was reviewed and updated.
It is clear from the review that bilateral phacoemulsification was scheduled also for cases with a risk of surgical problems. It must always be the surgeon‘s responsibility to decide whether expected risks in connection with surgery as a consequence of, for example, previous eye surgery, pupil or iris defects, type of cataract, defective zonular support, should be considered as contraindicative of bilateral surgery. In our material, iris hooks were used in some cases that required extra postoperative visits because of complications. Table 4 shows that most peroperative problems were related to iris or pupil (24 operations, 18 patients). Expected problems with the pupil should therefore lead to a meticulous weighing up of the risks and benefits of bilateral surgery.
In our clinical experience from the study period, patient satisfaction overall was quite high. Two dissatisfied patients were identified by the record review. One female patient aged 82 had homonymous hemianopsia diagnosed before surgery and although the operation resulted in better visual acuity she claimed her situation had not improved. One male patient aged 57 with preoperative myopia of approximately −7 dioptres in both eyes had an unexpected postoperative myopia of −2 dioptres in the eye operated upon first, while the second eye had emmetropia as planned. Such “refractive surprises” has been suggested as one reason to defer bilateral surgery, as the resulting postoperative refraction after first surgery cannot be used to judge the reliability of the calculated postoperative refraction of the second eye to be operated. It could be argued that even if the second eye is operated later, this second eye might deviate from predicted refraction in cases where the first eye was on target. Delayed second operation will not prevent this. Nevertheless, we think it is prudent to give information about this possible drawback, especially to those with conditions known to increase the difficulty to predict postoperative refraction. This includes patients with extremely long or short eyes, extreme or irregular corneal curvatures and, increasingly important, those who have previously undergone refractive surgery. For this last difficult group where the resulting refraction after the first cataract operation is suggested as one tool to better predict the result for the second eye, same day bilateral surgery should be avoided (Table 1). On the other hand, preoperative myopia or hyperopia, with associated deviations from normal axial length, may constitute reasons to recommend bilateral surgery because this will make it possible to emmetropise the patient without causing temporary anisometropia. In our material, myopia ranging from −2 to −11.5 dioptres and hyperopia from +3.75 to +4 dioptres were found in the records where one stated reason for bilateral operation was “avoiding postoperative anisometropia.” In the same subgroup we found deviation from calculated postoperative refraction on the hyperopic side of more than +0.5 dioptres in three patients (one of those deviated more than +1 dioptre). In seven patients there was un unexpected deviation to the myopic side of more than −0.5 dioptres (three patients between −1 and −2 dioptres, and two patients more than −2.5 dioptres). Thus we find in our material several patients with postoperative refraction deviating from preoperative calculation more than 1 dioptre but only one of those patients was dissatisfied. The rest of the patients with deviations, but without resulting anisometropia, were probably satisfied because comfortable glass correction could be given for both eyes soon after the surgery.
Bilateral surgery can also be performed with an interval between the two operations of 48 hours to some weeks.8,20 Although this reduces the risk of bilateral infection and increases the possibility of detecting postoperative deviation from planned refraction, albeit only in the first operated eye, economic and social advantages are also reduced.
The goal of cataract surgery is not only to remove the clouded lens in an eye, but also to give the patient the best and safest possible visual rehabilitation, using the limited resources of the healthcare system in the most effective way. While different healthcare systems will choose different means for attaining this goal, we have in recent years chosen bilateral phacoemulsification as one such means. We conclude from the results of this study that using bilateral phacoemulsification in selected cases is a safe way of speeding up visual rehabilitation of the patient with bilateral cataract, with reduced costs both for the general healthcare system and the patient. The inherent risk of bilateral complications must be balanced against the benefits. Different healthcare systems will have different ways of calculating the economic gains. Based on Figure 1 we make a rough estimate of the increase in direct costs for surgery with one eye operated upon at a time to be 1000–2500 Swedish kroners (approximately US$100–250/£70–170) per case. Indirect costs for transports, accompanying people, postoperative care, etc, are additional. Since the risk of bilateral complications cannot be disregarded, the patient must be informed of the potential risk of losing vision in both eyes following bilateral surgery. By closely monitoring the outcome of a large series of bilateral operations, we will acquire more precise knowledge to help the individual patient choose the type of surgery. In general, we have found the binocular surgery experience to have both advantages and disadvantages. The inherent risks have not deterred us from continuing with the approach. In a broad context, we have found the benefits for the patients and the healthcare system to predominate.
REFERENCES
- 1.Hanning M, Lundström M. Assessment of the maximum waiting time guarantee for cataract surgery. The case of a Swedish policy. Int J Technol Assess Health Care 1998;14:180–93. [DOI] [PubMed] [Google Scholar]
- 2.Nielsen PJ, Allerod CW. Evaluation of local anesthesia techniques for small incision cataract surgery. J Cataract Refract Surg 1998;24:1136–44. [DOI] [PubMed] [Google Scholar]
- 3.Jacobi FK, Kammann J, Jacobi KW, et al. Bilateral implantation of asymmetrical diffractive multifocal intraocular lenses. Arch Ophthalmol 1999;117:17–23. [DOI] [PubMed] [Google Scholar]
- 4.Beatty S, Aggarwal RK, David DB, et al. Simultaneous bilateral cataract extraction in the UK. Br J Ophthalmol 1995;79:1111–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramsay AL, Diaper CJ, Saba SN, et al. Simultaneous bilateral cataract extraction. J Cataract Refract Surg 1999;25:753–62. [DOI] [PubMed] [Google Scholar]
- 6.Totan Y, Bayramlar H, Cekic O, et al. Bilateral cataract surgery in adult and pediatric patients in a single session. J Cataract Refract Surg 2000;26:1008–11. [DOI] [PubMed] [Google Scholar]
- 7.Sharma TK, Worstmann T. Simultaneous bilateral cataract extraction. J Cataract Refract Surg 2001;27:741–4. [DOI] [PubMed] [Google Scholar]
- 8.Koch PS. Evolving trends in cataract surgery techniques and timing. Curr Opin Ophthalmol 1997;8:18–21. [PubMed] [Google Scholar]
- 9.Gray CS, Crabtree HL, O‘Connell JE. Waiting in the dark: cataract surgery in older people. BMJ 1999;318:1367–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mordue A, Parkin DW, Baxter C, et al. Thresholds for treatment in cataract surgery. J Publ Health Med 1994;16:393–8. [DOI] [PubMed] [Google Scholar]
- 11.Talbot EM, Perkins A. The benefit of second eye surgery. Eye 1998;12:983–9. [DOI] [PubMed] [Google Scholar]
- 12.Lundström M, Brege KG, Florén I, et al. Impaired visual function after cataract surgery assessed using the Catquest questionnaire. J Cataract Refract Surg 2000;26:101–8. [DOI] [PubMed] [Google Scholar]
- 13.Tyagi AK, McDonnell PJ. Visual impairment due to bilateral corneal endothelial failure following simultaneous bilateral cataract surgery. Br J Ophthalmol 1998;82:1341–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johansson B. Bilateral cataract surgery on the same day—a review of 27 cases. Acta Ophthalmol 2000;78:275 [Google Scholar]
- 15.Carey RG, Lloyd RC. Measuring quality improvement in healthcare: a guide to statistical process control applications. White Plains, NY: Quality Resources Press, 1995:70–7, 185.
- 16.Desai P, Reidy A, Minassian DC. Profile of patients presenting for cataract surgery in the UK: National data collection. Br J Ophthalmol 1999;83:893–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundström M, Stenevi U, Thorburn W. Cataract surgery in the very elderly. J Cataract Refract Surg 2000; 26:408–14. [DOI] [PubMed] [Google Scholar]
- 18.Lundström M, Stenevi U, Thorburn W. [Swedish Cataract Surgery 1999. The Swedish National Board of Health and Welfare: Annual report based on data from The Swedish National Cataract Register.] [Swedish] Karlskrona, Department of Ophthalmology, Blekinge Hospital, 2000.
- 19.Benezra D, Chirambo MC. Bilateral versus unilateral cataract extraction: advantages and complications. Br J Ophthalmol 1978;62:770–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Booth A, Coombes A, Rostron C. Bilateral cataract extraction can be safely done within 48 hours. BMJ 1999;319:579. [DOI] [PMC free article] [PubMed] [Google Scholar]