Abstract
Background: The small bowel is the most commonly affected site of Crohn’s disease (CD) although it may involve any part of the gastrointestinal tract. The current methodologies for examining the small bowel are x ray and endoscopy.
Aims: To evaluate, for the first time, the effectiveness of wireless capsule endoscopy in patients with suspected CD of the small bowel undetected by conventional modalities, and to determine the diagnostic yield of the M2A Given Capsule.
Patients: Seventeen patients (eight males, mean age 40 (15) years) with suspected CD fulfilled study entry criteria: nine had iron deficiency anaemia (mean haemoglobin 10.5 (SD 1.8) g%), eight had abdominal pain, seven had diarrhoea, and three had weight loss. Small bowel x ray and upper and lower gastrointestinal endoscopic findings were normal. Mean duration of symptoms before diagnosis was 6.3 (SD 2.2) years.
Methods: Each subject swallowed an M2A Given Capsule containing a miniature video camera, batteries, a transmitter, and an antenna. Recording time was approximately eight hours. The capsule was excreted naturally in the patient’s bowel movement, and the data it contained were retrieved and interpreted the next day.
Results: Of the 17 study participants, 12 (70.6%, six males, mean age 34.5 (12) years) were diagnosed as having CD of the small bowel according to the findings of the M2A Given Capsule.
Conclusions: Wireless capsule endoscopy diagnosed CD of the small bowel (diagnostic yield of 71%). It was demonstrated as being an effective modality for diagnosing patients with suspected CD undetected by conventional diagnostic methodologies.
Crohn’s disease (CD) is a systemic granulomatous disease that may involve any part of the alimentary tract: the small bowel is the affected site in 30–40% of cases.1 All of the recent studies published in the literature have reported a worldwide rise in the incidence of CD, with 25–33% of patients presenting with symptoms before the age of 20 years.2 The “gold standard” for the diagnosis of CD includes the presence of the following features: abdominal pain, weight loss, iron deficiency anaemia, diarrhoea, an elevated erythrocyte sedimentation rate (ESR), fever, and typical evidence of pathological processes on conventional imaging techniques—that is, small bowel x ray, computerised tomography (CT) of the abdomen, endoscopy, and colonoscopy with ileoscopy.
The reliability of radiological studies is highly influenced by the skill and experience of the operator and how fine is the detail of the mucosa on the film. CT of the abdomen does not detect mucosal inflammation: it can show transmural thickening and extramural complications but it is incapable of discerning CD in the early stages of disease.
Improved instrument design and therapeutic capability has led to an increasing use of push endoscopy. Push endoscopy however takes between 15 and 45 minutes, it is an invasive procedure (usually requiring sedation and analgesia), and there is a danger of perforation.3 The complications that may occasionally occur are usually related to the use of an overtube to facilitate deep intubation of the small bowel. Conventional endoscopic techniques for examining the small bowel are also limited by the length of the small intestine: the instrument can only examine 80–120 cm beyond the ligament of Trietz.3,4
Sonde endoscopy has, at least in theory, the potential to examine the entire small bowel. This technique employs a long scope that is inserted transnasally into the stomach and is then pushed through the pylorus with a gastroscope that is passed through the mouth.5,6 It is carried by peristalsis which propels a balloon inflated at the tip. This technique is not widely performed because it requires long examination times (6–8 hours), is extremely uncomfortable and often painful, and carries a risk of perforation.3,4
Another approach to small bowel imaging is examination of the entire small bowel by intraoperative endoscopy. The limitations of this option are the drawbacks associated with exploratory laparotomy and with general anaesthesia.7
Thus it is generally accepted that the current visualisation and imaging methods available to the gastroenterologist in diagnosing small bowel diseases and disorders are unsatisfactory.3 The need for enhanced endoscopic examination of the small bowel, particularly for evidence of inflammatory disease, is well recognised.8 The alternative solution should be relatively comfortable for the patient, easy to use by the gastroenterologist, relatively inexpensive, and one that will provide a reasonable level of visual imaging for the detection of small bowel abnormalities. The Given Diagnostic Imaging System (M2A Capsule)9,10 is a new modality designed to accommodate these requirements.
The current study is a prospective one that was carried out from August 2000 until December 2001, and represents our initial experience with the M2A Capsule in diagnosing CD in patients who had earlier undergone conventional investigations in which no characteristic abnormalities were detected.
MATERIALS AND METHODS
This prospective clinical study was conducted from August 2000 until December 2001 in the departments of gastroenterology of two Israeli medical centres (Hillel-Yaffe in Hadera and Asaf-Harofe in Zrifin). This was the first trial to evaluate the application of the Given M2A Capsule in patients with suspected CD. The investigation was approved by both the local and national ethics authorities, and each patient signed informed consent to participate.
Study population
We sent out a nationwide “call for patients” to our gastroenterologist colleagues. Originally, 18 subjects with symptoms of abdominal pain, fever, weight loss, anaemia, elevated ESR with negative small bowel x ray, normal oesophagogastroduodenoscopy (OGD), and colonoscopy carried out ≤6 months earlier were eligible for study admission. Exclusion criteria included a history of bowel obstruction, x ray evidence of small bowel stricture, evidence of any pathological abnormalities of the small bowel, major abdominal operation, any use of non-steroidal anti-inflammatory drugs during the past year, and known to be immune compromised or human immunodeficiency virus (HIV) positive, leading to one candidate being dropped. The remaining 17 patients (eight males and nine females, mean age 40 (15) years) with suspected but undiagnosed CD comprised the final study cohort.
Each subject swallowed the M2A Given Capsule containing a miniature video camera, batteries, a transmitter, and an antenna. Recording time was approximately eight hours and the disposable capsule was excreted naturally in the patient’s bowel movement. The data from the recorder were loaded onto a workstation equipped with proprietary image processing software and were reviewed and interpreted by the authors the following day.
Comparison of recordings with healthy control and confirmed CD groups
Data for normal controls were retrieved from the recordings of 20 volunteers who had normal small bowel studies. As one complication of CD is stricture of the bowel lumen, we are extremely cautious in conducting this examination when other evidence of CD is compelling because of the possibility that the capsule will get lodged in the bowel. However, we had recordings of eight patients with confirmed CD without stricture and we used these data for comparison.
Wireless capsule
The M2A Given Capsule is comprised of three main subsystems: an ingestible capsule, a data recorder, and a workstation equipped with proprietary image processing software. The ingestible M2A Imaging Capsule photographs video images during natural propulsion through the digestive system. It is designed to be used once. It transmits the acquired images via a digital radio frequency communication channel to the recorder unit located outside the body. The portable data recorder is an external receiving/recording unit that receives data transmitted by the ingestible capsule. It consists of a sensor array attached to the abdomen and a receiver which measures signal strength at each sensor. The receiver selects the strongest signal and receives the video data from it. The recorder also contains memory media for the accumulation of the signal strength and video data generated during the examination. On completion of the examination, the physician transfers the accumulated data in the recorder to the workstation for interpretation. Data transfer is performed via a high capacity digital link. The workstation is equipped with RAPID advanced image processing software and is a modified standard personal computer designed for offline storage, interpretation, and analysis of the acquired data as well as for generating reports.
Method
After an overnight 12 hour fast, patients ingested the wireless video capsule (Given M2A Video Capsule System). They were allowed to drink one hour after ingesting the capsule and to eat two hours afterwards. After having ingested the capsule with a small amount of water, patients were free to go about their usual activities. The recorder functioned for 7–8 hours after ingestion. Patients were asked to retrieve the capsule from their faeces, which they did from 12 hours to five days after ingestion.
The results from the video that was produced from the data recorded by each capsule were reviewed independently by two experts (ZF and ES) who were blinded to the clinical data. There was 100% agreement between the two raters.
RESULTS
The pertinent characteristics of the study population are shown in table 1 ▶. The symptoms of the 17 patients enrolled in the study were consistent with suspected CD. Twelve had abdominal pain, 10 had iron deficiency anaemia (mean 10.5 g% haemoglobin), six had diarrhoea, four had an elevated ESR, three had weight loss, and one had fever: some had more than one symptom. Mean duration of symptoms before the diagnosis was 6.3 (SD 2.2) years. Within six months prior to study entry, all patients had undergone a small bowel x ray and total colonoscopy with ileoscopy (the ileoscopy succeeded in only six patients) which were normal without exception.
Table 1.
Characteristics of the study population
| Study patients | Patient’s diagnosed as having CD based on capsule enteroscopy findings | |
| Patients (n) | 17 | 12 |
| Age (y) (mean (range)) | 40 (18–68) | 34.5 (18–63) |
| Males (%) | 47 | 50 |
| Haemoglobin (g%) (mean (SD)) | 10.5 (1.8) | 10.5 (1.8) |
| Anaemia* (%) | 58.8 | 75 |
| Abdominal pain* (%) | 70.5 | 66.6 |
| Diarrhoea* (%) | 35.3 | 58.3 |
| Weight loss* (%) | 17.6 | 25 |
| Duration of disease (y) (mean (SD)) | 6.3 (2.2) | 7.4 (3.2) |
*Some of the patients had more than one symptom.
CD, Crohn’s disease.
All patients ingested the capsule smoothly and there were no side effects. Based on the results of the Given M2A Capsule, the two expert examiners (ZF and ES) independently diagnosed CD of the small bowel in 12/17 patients (70.6%) and a normal appearing small bowel mucosa in the remaining five (29.4%). Among the findings detected by the capsule were mucosal erosions, ulcers, and strictures (figs 1,2 ▶ ▶). The distribution of the lesions was mainly in the distal part of the small bowel, and the degree of severity ranged from mild to severe. Only one patient had CD in the distal jejunum which could not be reached with push endoscopy.
Figure 1.
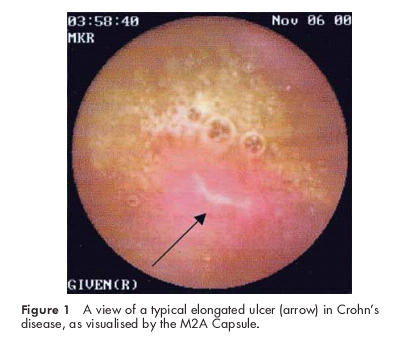
A view of a typical elongated ulcer (arrow) in Crohn’s disease, as visualised by the M2A Capsule.
Figure 2.

Stricture of an ileum with irregular ulceration (black arrows) surrounding a narrowed lumen (white arrow). The capsule passed through without difficulty.
Most of the patients underwent total colonoscopy (15/17) and OGD (16/17); 7/17 had abdominal CT and all had small bowel x ray series. Some of the patients underwent those procedures more than once: the mean number of procedures they had undergone previously was 5.4 (1.14).
Of the 12 patients who received medications, 10 showed good clinical improvement after 5-ASA (mean 3.5 g/day) and short term steroid treatment while the other two showed some improvement in their clinical symptoms with the same treatment. Follow up ranged from one to eight months (mean four months).
DISCUSSION
It is generally accepted that the visualisation and imaging methods currently available to the gastroenterologist in diagnosing small bowel diseases and disorders are unsatisfactory and that there is a need for a solution that will be relatively comfortable for the patient, easy to use by the gastroenterologist, relatively inexpensive, and one that will provide a reasonable level of visual imaging for the detection of small bowel abnormalities. The Given Diagnostic Imaging System (M2A Capsule)9,10 is a new modality designed to answer these needs.
The capsule enteroscope contains a miniature video camera, a light source, batteries, and a radio transmitter. Video images are transmitted by means of radio telemetry to the sensor array attached to the body, allowing images to be captured from the entire gastrointestinal tract. Images from a period of time as long as eight hours are stored in a portable recorder.
In the preliminary results presented herein, the Given M2A Capsule successfully imaged and provided good views of the gastrointestinal tract from the mouth to the colon in 10 of 12 CD patients. The recording stopped before entry into the colon, possibly because of slow transit time due to the inflamed small bowel mucosa in these two patients. Although the capsule failed to reach the caecum however we could still identify typical lesions of CD from the recordings that emerged before the battery ran out. The information gained was helpful in further treatment planning for all of these patients and this leads us to propose that the Given M2A Diagnostic System shows promise of being a valuable tool in the assessment of small bowel disease.
There are two limitations to this study that should be noted. Firstly, follow up for patients receiving medications was short (mean four months (range 1–8)). Secondly, failure to diagnose CD in two cases may well have been caused by the effect of the disease on the motility of the small bowel thus slowing the movement of the capsule and not allowing it to image the entire small bowel in the limited time provided by the battery.
To date, over 8000 patients have undergone wireless capsule endoscopy worldwide. The authors have themselves conducted approximately 250 such examinations. This is the first description of an attempt to diagnose CD of the small bowel by a wireless capsule. Our study demonstrated a high diagnostic yield in patients with clinical symptoms indicative of CD who had previously undergone several diagnostic procedures that showed normal results. Our patients had long intervals from the onset of disease until diagnosis: the wireless capsule might have been able to provide a correct diagnosis during the early stages of disease as well as in cases of less severe forms. We propose the wireless capsule as being an effective modality for diagnosing patients with suspected CD.
Acknowledgments
Esther Eshkol is thanked for editorial assistance.
Abbreviations
CD, Crohn’s disease
CT, computerised tomography
ESR, erythrocyte sedimentation rate
OGD, oesophagogastroduodenoscopy
Footnotes
Drs Fireman and Scapa are members of the medical advisory board of Given Imaging.
REFERENCES
- 1.Kornbluth A, Sachar D, Salomon P. Crohn’s disease. In: Sleisenger MN, Fordtran JS, eds. Gastrointestinal and liver diseases, 6th edn. Philadelphia: WB Saunders, 1998:1708–34.
- 2.Fielding JF. Clinical features of Crohn’s disease in Ireland. Am J Gastroenterol 1986;81:524–8. [PubMed] [Google Scholar]
- 3.Swain CP. The role of enteroscopy in clinical practice. Gastrointest Endosc Clin N Am 1999;9:135–44. [PubMed] [Google Scholar]
- 4.Lewis BS. The history of enteroscopy. Gastrointest Endosc Clin N Am 1999;9:1–11. [PubMed] [Google Scholar]
- 5.Lewis BS, Waye JD. Total small bowel enteroscopy. Gastrointest Endosc 1987;33:435–8. [DOI] [PubMed] [Google Scholar]
- 6.Seensalu R. The sonde examination. Gastrointest Endosc Clin N Am 1999;9:37–59. [PubMed] [Google Scholar]
- 7.Ress A M, Benaccin JC, Sarr MG. Efficacy of intraoperative enteroscopy in diagnosis and prevention of recurrent, occult gastrointestinal bleeding. Am J Gastroenterol 1994;89:2143–6. [DOI] [PubMed] [Google Scholar]
- 8.Gay GJ, Delmotte JS. Enteroscopy in small intestinal inflammatory diseases. Gastrointest Endosc Clin N Am 1999;9:115–23. [PubMed] [Google Scholar]
- 9.Iddan G, Meron G, Glukhovsky A, et al. Wireless capsule endoscopy. Nature 2000;405:417. [DOI] [PubMed] [Google Scholar]
- 10.Appleyard M, Fireman Z, Glukhovsky A, et al. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for detection of small bowel lesions. Gastroenterology 2000;119:1431–8. [DOI] [PubMed] [Google Scholar]


