Abstract
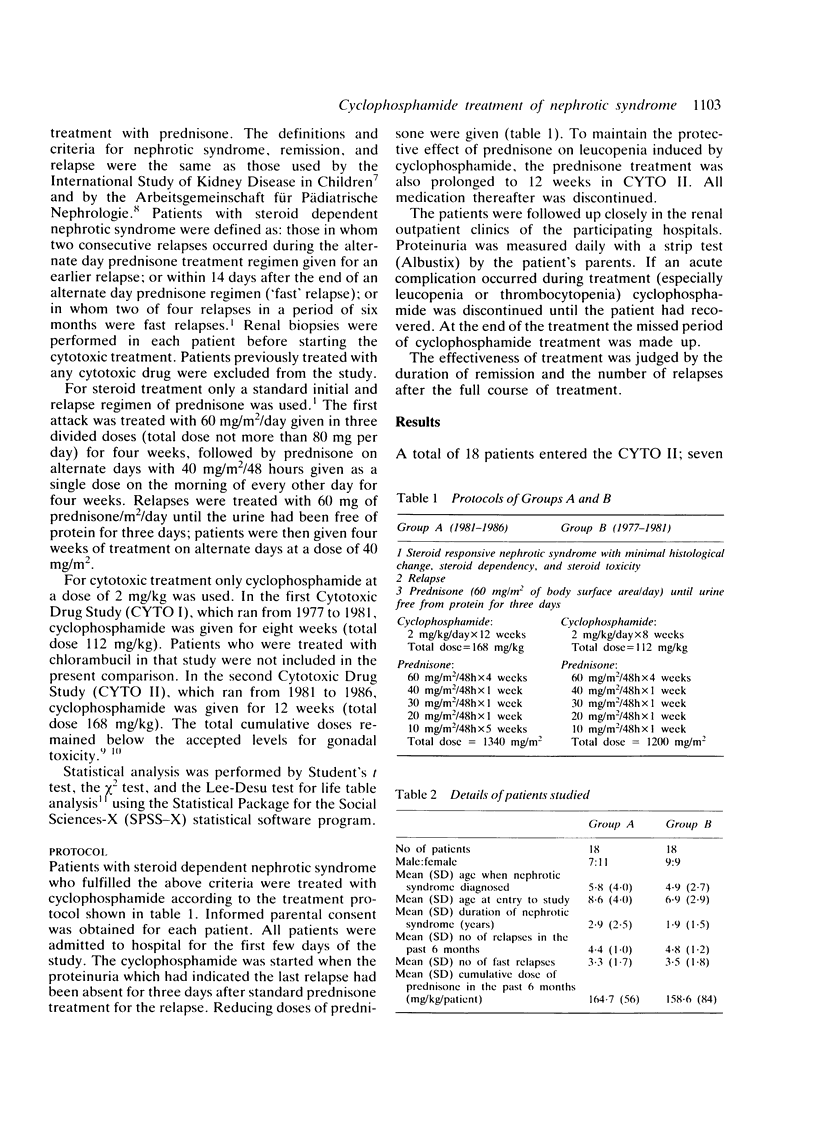
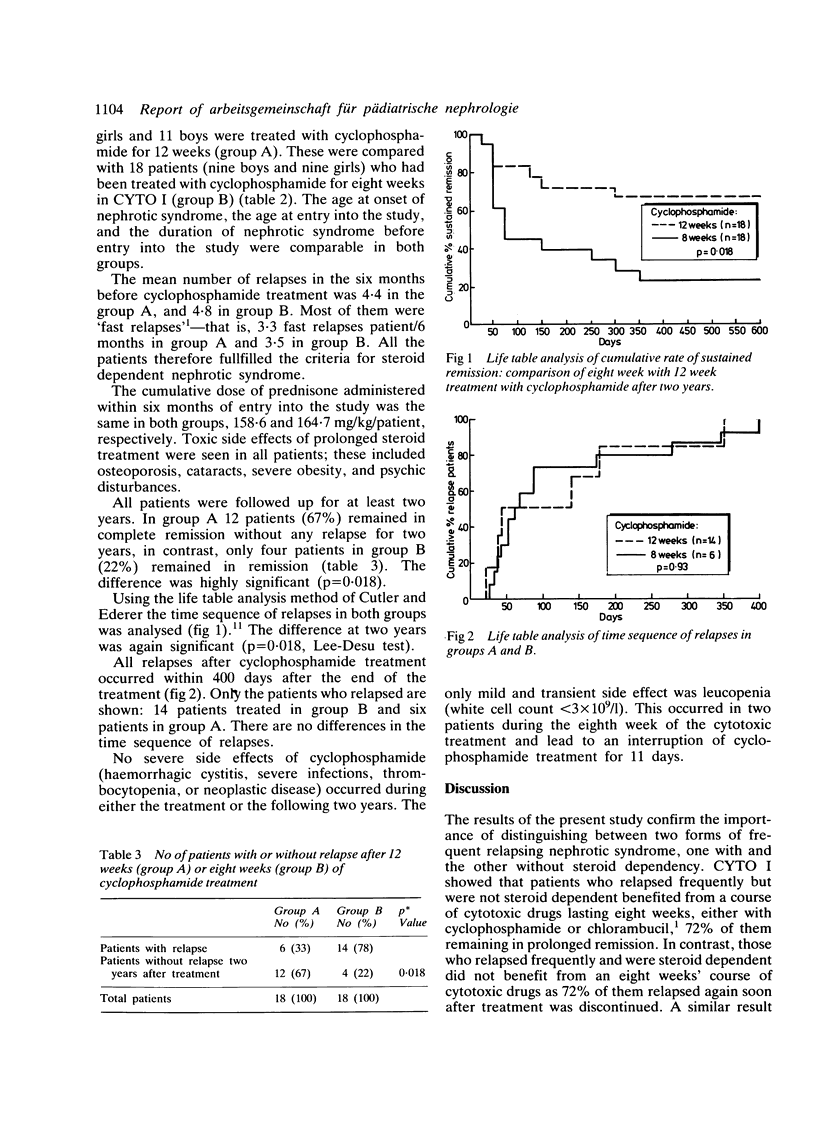
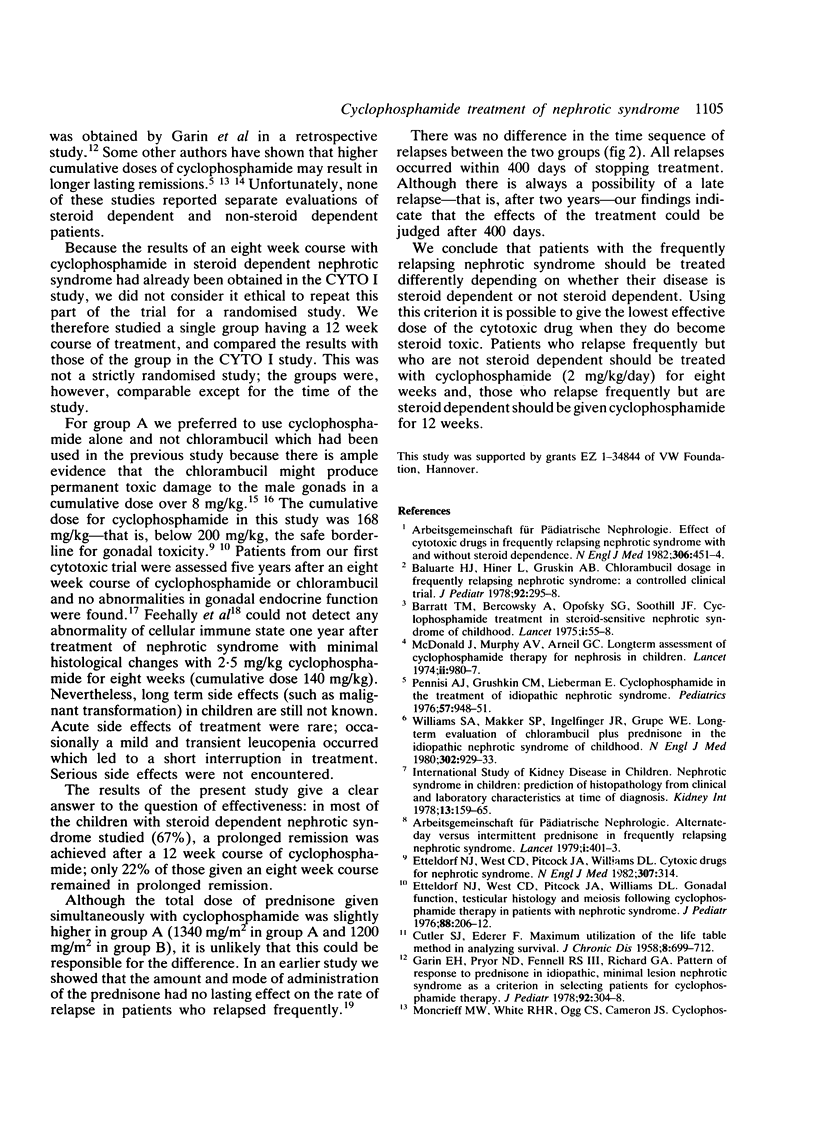
In a prospective study (Cytotoxic Drug Study II), 18 children with steroid dependent nephrotic syndrome and steroid toxicity were treated with cyclophosphamide (2 mg/kg body weight/day) for 12 weeks in combination with reducing doses of prednisone (group A). This group was compared retrospectively with 18 children with steroid dependent nephrotic syndrome, studied as part of the Cytotoxic Drug Study I, and who had received cyclophosphamide for eight weeks (group B). There were no differences between the groups in age at the onset of the nephrotic syndrome, age at entry into the study, and duration of the nephrotic syndrome before entry into the study. The number of relapses during the six months before the treatment was the same in both groups. Two years after treatment 12 of 18 children treated with cyclophosphamide for 12 weeks were still in remission. By contrast, only four of of 18 children treated with cyclophosphamide for eight weeks were still in remission. The cumulative rates of sustained remissions were significantly higher (67% and 22%, respectively) in group A. All relapses were observed within 400 days of stopping cytotoxic treatment. No severe side effects of cyclophosphamide occurred up to two years after treatment had been stopped. We conclude that for children with steroid dependent nephrotic syndrome and steroid toxicity cyclophosphamide treatment should be prolonged to 12 weeks to increase the likelihood of a prolonged remission.
Full text
PDF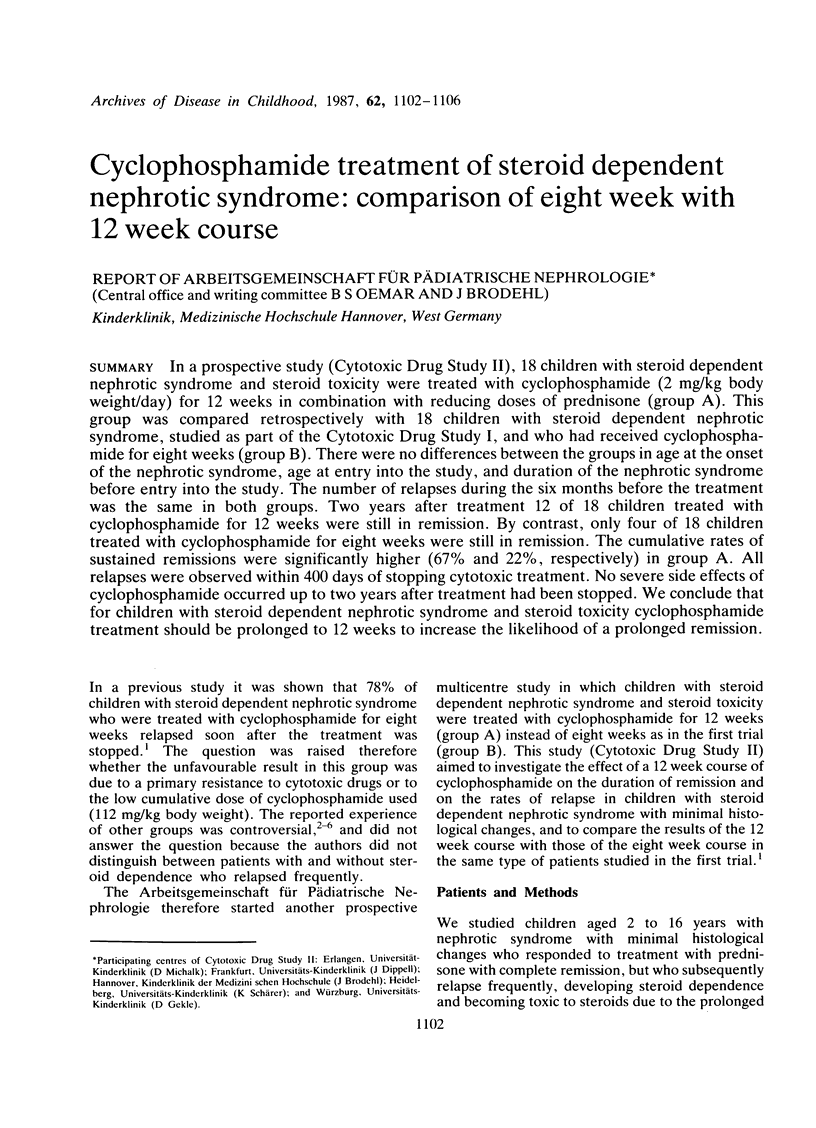
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baluarte H. J., Hiner L., Gruskin A. B. Chlorambucil dosage in frequently relapsing nephrotic syndrome: a controlled clinical trial. J Pediatr. 1978 Feb;92(2):295–298. doi: 10.1016/s0022-3476(78)80030-4. [DOI] [PubMed] [Google Scholar]
- Barratt T. M., Bercowsky A., Osofsky S. G., Soothill J. F. Cyclophosphamide treatment in steroid-sensitive nephrotic syndrome of childhood. Lancet. 1975 Jan 11;1(7898):55–58. doi: 10.1016/s0140-6736(75)91068-5. [DOI] [PubMed] [Google Scholar]
- CUTLER S. J., EDERER F. Maximum utilization of the life table method in analyzing survival. J Chronic Dis. 1958 Dec;8(6):699–712. doi: 10.1016/0021-9681(58)90126-7. [DOI] [PubMed] [Google Scholar]
- Callis L., Nieto J., Vila A., Rende J. Chlorambucil treatment in minimal lesion nephrotic syndrome: a reappraisal of its gonadal toxicity. J Pediatr. 1980 Oct;97(4):653–656. doi: 10.1016/s0022-3476(80)80035-7. [DOI] [PubMed] [Google Scholar]
- Chiu J., McLaine P. N., Drummond K. N. A controlled prospective study of cyclophosphamide in relapsing, corticosteroid-responsive, minimal-lesion nephrotic syndrome in childhood. J Pediatr. 1973 Apr;82(4):607–613. doi: 10.1016/s0022-3476(73)80585-2. [DOI] [PubMed] [Google Scholar]
- Etteldorf J. N., West C. D., Pitcock J. A., Williams D. L. Gonadal function, testicular histology, and meiosis following cyclophosphamide therapy in patients with nephrotic syndrome. J Pediatr. 1976 Feb;88(2):206–212. doi: 10.1016/s0022-3476(76)80983-3. [DOI] [PubMed] [Google Scholar]
- Feehally J., Beattie T. J., Brenchley P. E., Coupes B. M., Houston I. B., Mallick N. P., Postlethwaite R. J. Modulation of cellular immune function by cyclophosphamide in children with minimal-change nephropathy. N Engl J Med. 1984 Feb 16;310(7):415–420. doi: 10.1056/NEJM198402163100702. [DOI] [PubMed] [Google Scholar]
- Garin E. H., Pryor N. D., Fennell R. S., 3rd, Richard G. A. Pattern of response to prednisone in idiopathic, minimal lesion nephrotic syndrome as a criterion in selecting patients for cyclophosphamide therapy. J Pediatr. 1978 Feb;92(2):304–308. doi: 10.1016/s0022-3476(78)80032-8. [DOI] [PubMed] [Google Scholar]
- Guesry P., Lenoir G., Broyer M. Gonadal effects of chlorambucil given to prepubertal and pubertal boys for nephrotic syndrome. J Pediatr. 1978 Feb;92(2):299–303. doi: 10.1016/s0022-3476(78)80031-6. [DOI] [PubMed] [Google Scholar]
- McDonald J., Murphy A. V., Arneil G. C. Long-term assessment of cyclophosphamide therapy for nephrosis in children. Lancet. 1974 Oct 26;2(7887):980–982. doi: 10.1016/s0140-6736(74)92073-x. [DOI] [PubMed] [Google Scholar]
- Moncrieff M. W., White R. H., Oggs C. S., Cameron J. S. Cyclophosphamide therapy in the nephrotic syndrome in childhood. Br Med J. 1969 Mar 15;1(5645):666–671. doi: 10.1136/bmj.1.5645.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennisi A. J., Grushkin C. M., Lieberman E. Cyclophosphamide in the treatment of idiopathic nephrotic syndrome. Pediatrics. 1976 Jun;57(6):948–951. [PubMed] [Google Scholar]
- Williams S. A., Makker S. P., Ingelfinger J. R., Grupe W. E. Long-term evaluation of chlorambucil plus prednisone in the idiopathic nephrotic syndrome of childhood. N Engl J Med. 1980 Apr 24;302(17):929–933. doi: 10.1056/NEJM198004243021701. [DOI] [PubMed] [Google Scholar]


