Two dominant periodic fevers, tumour necrosis factor (TNF) receptor‐associated periodic syndrome (TRAPS) and cryopyrin‐associated periodic syndrome (CAPS), are prominent auto‐inflammatory disorders. Mutations in the 55 kDa TNF receptor superfamily 1A gene (TNFRSF1A) and in the cold‐induced auto‐inflammatory syndrome 1 gene (CIAS1) were recently associated with TRAPS1 and CAPS,2 respectively. Following publications describing the efficacy of etanercept (enbrel), a recombinant human TNF receptor 1B fusion protein in patients with TRAPS3 and anakinra (kineret), a recombinant human interleukin‐1 (IL1)‐receptor antagonist, in patients with CAPS,4 targeted biotherapies have been repeatedly and successfully given for these two conditions.
Our proband (fig 1) is a 36‐year‐old French woman who presented with rashes of urticaria and oedema precipitated by exposure to heat and water. These rashes, lasting a few hours and recurring twice a month since the patient was 6 years old, were associated with moderate fever, symmetric arthralgia of the wrists, ankles and hip, myalgia, painful cutaneous contact, bipolar aphthosis, intense fatigue and conjunctivitis. She had no uveitis, no folliculitis and no pathergy, ruling out Behçet's disease. Levels of C reactive protein were repeatedly found to be normal. Her mother, now aged 60 years, exhibited the same symptomatology, except that she had no genital aphthosis and no urticaria and her oedemas were triggered by both cold and heat. She also showed severe bilateral deformation of the distal interphalangeal joints. The proband's daughter, aged 8 years, had fever, urticaria and oral aphthosis. Because these phenotypes overlapped with symptoms reported for TRAPS and CAPS, we first sequenced TNFRSF1A exons 2–4 and CIAS1 exon 3, thereby covering 98% of the known mutations in both genes. We discovered double heterozygosity for R92Q and V198M in both the proband and her mother. No mutation was found in the two other periodic fever genes: MEFV responsible for familial Mediterranean fever and MVK responsible for the hyper immunoglobulin D syndrome (not shown). Although the IL1‐receptor antagonist has been consistently shown to dramatically improve CAPS, and sometimes TRAPS, in patients within hours of the first injection, the proband's symptoms did not decrease even after 1 month of daily subcutaneous injections of 100 mg anakinra. Instead, she needed to be hospitalised for severe side effects, including fatigue, erythema and anaemia. Four weeks later, she was given etanercept 25 mg subcutaneous twice a week. This treatment was rapidly withdrawn after the onset of bronchitis, then unsuccessfully re‐introduced for one month 8 months later. The other symptomatic family members declined any treatment.
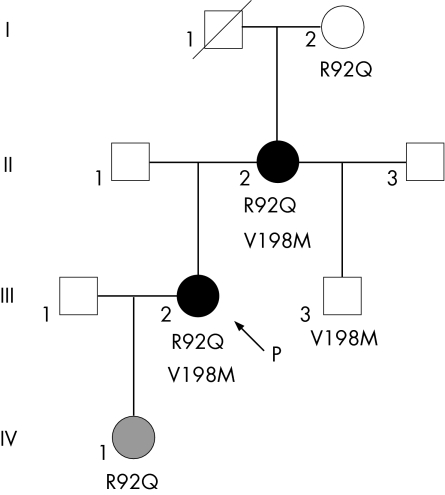
Figure 1 Digenic expression of tumour necrosis factor receptor‐associated periodic syndrome and cryopyrin‐associated periodic syndrome mutations. The two patients with the most severe phenotypes (black circles), including the proband (P, arrowed), who is refractory to anakinra, inherited both tumour necrosis factor receptor superfamily 1A gene (R92Q) and cold‐induced auto‐inflammatory syndrome 1 (V198M) mutations. By contrast, two of the three people with only one variant, the grandmother (R92Q) and the step‐brother (V198M), were completely asymptomatic. The daughter (grey circle, R92Q) had a milder symptomatology.
We describe here the first CIAS1‐positive patient refractory to anakinra and provide a possible molecular basis for this. R92Q and V198M are individually recognised as mild and low‐penetrance mutations.5 The two patients with combined mutations (II2 and III2) presented with quite atypical, overlapping and severe symptoms, whereas the three people with only one variant were either totally asymptomatic (I2, III3) or had a much milder disease (IV1). Clustering of hereditary auto‐inflammatory mutated genes has been occasionally reported,5 but familial molecular analysis showing a clear segregation between the phenotype and the genotype has never been carried out before. Our data strongly suggest that severe phenotypes and unresponsiveness to biotherapies may result from digenic inheritance, which is consistent with the transmission pattern observed in this family (fig 1).
Footnotes
Competing interests: None declared.
References
- 1.McDermott M F, Aksentijevich I, Galon J, McDermott E M, Ogunkolade B W, Centola M.et al Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell 199997133–144. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman H M, Mueller J L, Broide D H, Wanderer A A, Kolodner R D. Mutation of a new gene encoding a putative pyrin‐like protein causes familial cold autoinflammatory syndrome and Muckle‐Wells syndrome. Nat Genet 200129301–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drewe E, McDermott E M, Powell R J. Treatment of the nephrotic syndrome with etanercept in patients with the tumor necrosis factor receptor‐associated periodic syndrome. N Engl J Med 20003431044–1045. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins P N, Lachmann H J, McDermott M F. Interleukin‐1‐receptor antagonist in the Muckle‐Wells syndrome. N Engl J Med 20033482583–2584. [DOI] [PubMed] [Google Scholar]
- 5.Touitou I, Notarnicola C, Grandemange S. Identifying mutations in autoinflammatory diseases: towards novel genetic tests and therapies? Am J Pharmacogenomics 20044109–118. [DOI] [PubMed] [Google Scholar]