Abstract
Introduction: Delirium, an organic psychiatric syndrome, occurs in 10% of hospitalized patients and is characterized by fluctuating consciousness and impaired cognition, perception, and behavior.
Method: Charts of 11 consecutive patients with delirium were retrospectively reviewed. These patients were given quetiapine fumarate, a novel antipsychotic, as first-line treatment for their symptoms. The charts of a control group of 11 patients treated with haloperidol, the standard treatment for delirium, during the same time period were also evaluated. The Delirium Rating Scale (DRS) was used to evaluate the efficacy of each treatment.
Results: Ten of 11 patients in both groups had > 50% improvement in DRS scores. There was no difference in onset of symptom resolution, duration of treatment, and overall clinical improvement. Quetiapine was better tolerated in these medically ill patients.
Conclusion: Quetiapine appears to be an efficacious and well-tolerated treatment for delirium. Further prospective studies are warranted.
Delirium is an organic psychiatric syndrome characterized by fluctuating consciousness and impairment in cognition, perception, and behavior. It is generally short-lived and has symptoms similar to longer duration psychosis seen in patients suffering from schizophrenia, major depression with psychosis, or bipolar disorder with psychosis. Psychiatric patients with these disorders will often experience hallucinations and delusions, such as paranoia. Medically delirious patients may suffer from hallucinations and delusions, as well as from confusion and disorientation. Delirium occurs in approximately 10% of hospitalized medical and surgical patients and in up to 80% of patients with terminal illness.1–3 It is associated with increased mortality and longer hospitalization.4–6
Antipsychotic medications are generally efficacious in treating psychotic features regardless of etiology, and outside of treating the underlying medical cause of delirium, they are the pharmacologic treatment of choice for these patients.2 Haloperidol is considered the “gold standard” because it has few anticholinergic side effects, few active metabolites, and minimal propensity to cause sedation and hypotension. Haloperidol can be administered orally, intramuscularly, or intravenously, causing the fewest extrapyramidal side effects when administered intravenously.7 Conventional, high-potency antipsychotics such as haloperidol tend to produce higher rates of neurologic side effects, such as parkinsonism and dystonia, whereas lower potency drugs such as chlorpromazine can exacerbate delirium owing to anticholinergic effects.
Newer antipsychotics have much lower risk of causing serious neurologic side effects. This more favorable side effect profile occurs because these agents produce a blockade of dopamine and serotonin receptors, whereas the older, conventional antipsychotics only block dopamine. This favorable side effect profile has prompted use of these newer antipsychotics in the medically ill, and specifically in delirious patients. Risperidone8,9 and olanzapine10 were found to be effective, well-tolerated treatments for delirium. In similar fashion, we evaluated the use of the novel antipsychotic quetiapine fumarate to treat delirium in a general hospital setting. We hypothesized that quetiapine, which has safety and efficacy profiles similar to those of risperidone and olanzapine in psychotic disorders, would be at least as efficacious as haloperidol in treating delirium and would be better tolerated.
METHOD
The State University of New York Upstate Medical University's hospital is a 350-bed tertiary care general hospital that treats both indigent and privately insured patients. The Psychiatric Consultation Service of University Hospital comprises 2 psychiatrists, 2 psychiatric residents, and 1 psychiatric nurse specialist. This service is often asked to evaluate and provide treatment recommendations for delirious patients.
On review of patient care statistics, it was noted that 11 patients with delirium had been treated with quetiapine from 1997 to 1999. The authors retrospectively reviewed those charts and collected data with regard to age, sex, medical diagnoses, maximum dose of quetiapine, time to peak response with quetiapine, total duration of treatment, and Delirium Rating Scale (DRS)11 scores prior to and after treatment. DRS is a validated scale and is a usual part of the consultation workup. Scores were derived pretreatment and posttreatment. When available, these scores were taken directly from clinicians' notes. If no score was available, the chart was reviewed by an independent psychiatrist and a score retrospectively assigned on the basis of chart-listed symptoms. Clinicians' documentation of symptoms was felt to be adequate in all charts studied. A random selection of patients with haloperidol-treated delirium were evaluated similarly and acted as controls. Patients were excluded if they were taking any other concomitant antipsychotic medication. Patients were not excluded on the basis of type or severity of medical illness or concomitant medications of other sources. Descriptive statistics, chi-square analyses, and t tests were used to compare these groups to determine dosing, efficacy, and tolerability profiles.
RESULTS
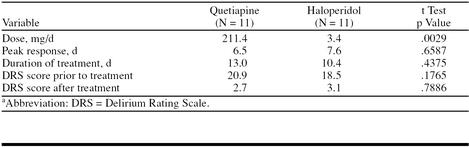
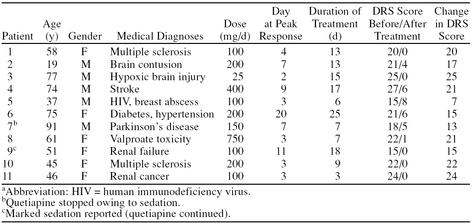
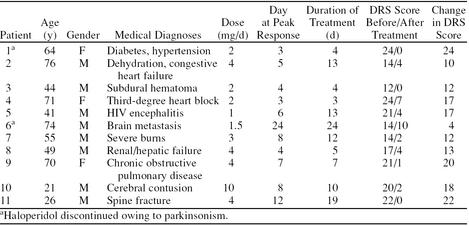
The mean age for the quetiapine-treated patients was 57.6 years (range, 19–91 years) and for the haloperidol-treated patients, 53.7 years (range, 21–74 years). No significant baseline differences were found between the haloperidol- and the quetiapine-treated population of delirious patients in regard to age, sex, DRS scores, or efficacy measures. All but the latter suggest that the haloperidol control group was evenly matched to the quetiapine group demographically and in regard to symptom severity. The mean dose of quetiapine was 211.4 mg/day and of haloperidol, 3.4 mg/day. These doses tend to be lower than those used in schizophrenia, but are consistent with the literature and clinical practice in regard to delirium, which requires lower doses. Ten of 11 patients on haloperidol treatment had > 50% improvement in DRS scores, and 10 of 11 quetiapine-treated patients had a similar improvement. DRS improvement is a global score that incorporates orientation, agitation, perceptual disturbance, sleep-wake disturbance, and course-of-illness subscales. Time to peak response, total duration of treatment, and change in DRS scores were not significantly different (Table 1). Demographics of patients taking quetiapine and haloperidol are described in Tables 2 and 3, respectively.
Table 1.
Mean Dose and Response Rates for Patients Taking Quetiapine or Haloperidola
Table 2.
Characteristics of Quetiapine-Treated Patientsa
Table 3.
Characteristics of Haloperidol-Treated Patients
Two patients on haloperidol treatment developed extrapyramidal symptoms (EPS) leading to discontinuation of the drug. None of the patients on quetiapine treatment (including 1 with Parkinson's disease) developed EPS. Quetiapine led to mild-to-moderate sedation in 2 patients (1 had to discontinue the drug). These side effect rates are similar in the psychiatric population in regard to quetiapine and haloperidol.
DISCUSSION
Ours is the first report of quetiapine in the treatment of delirium. Traditionally, high-potency antipsychotics, particularly haloperidol, are used as first-line treatment for delirious patients. Unfortunately, haloperidol is frequently associated with extrapyramidal neurologic side effects, including akathisia. This was evident in 2 of our patients who developed significant EPS. Often, clinicians will use antiparkinsonian agents that possess antimuscarinic effects to treat EPS. These agents are particularly problematic in delirious patients since they may exacerbate anticholinergic delirium. Quetiapine is a novel antipsychotic agent whose mechanism of action is similar to that of risperidone and olanzapine in that it blocks the serotonin-2A receptors preferentially compared with dopamine-2 receptors. It has a low propensity to cause EPS and is also devoid of antimuscarinic blockade. Quetiapine was as efficacious as haloperidol and may be better tolerated, since haloperidol needed to be discontinued more frequently.
Sipahimalani et al.8 treated 11 consecutive patients who had delirium of multifactorial etiology with risperidone (mean ± SD dose = 1.59 ± 0.8 mg/day). The mean ± SD duration of treatment with risperidone was 8.9 ± 5.2 days. Maximum response was seen at 5.1 ± 4.3 days. Eight of 11 patients showed some improvement with risperidone. The drug was very well tolerated in these patients with delirium. In another study, Sipahimalani and Masand10 used olanzapine (mean dose = 8.2 ± 3.4 mg at bedtime) to treat 11 delirious patients and compared them with a control group of 11 patients who were treated with haloperidol (mean dose = 5.1 ± 3.5 mg at bedtime). Peak response time was similar in both groups. Five of 11 olanzapine-treated patients and 6 of 11 haloperidol-treated patients showed a greater than 50% improvement on the DRS. Five of the haloperidol-treated patients had EPS (parkinsonism, dystonia) or excessive sedation.
The above reports point to the efficacy and tolerability of the newer antipsychotics in the treatment of delirium of multifactorial etiology. These newer antipsychotics are more efficacious than conventional antipsychotics in treating negative and mood symptoms and are less likely to cause neurologic side effects and tardive dyskinesia. They offer viable alternatives to the conventional antipsychotics for the treatment of not only schizophrenia but nonschizophrenic conditions such as delirium as well.12 The purpose of this article is to provide the primary care or hospital-based physician with up-to-date information about these newer and potentially safer treatments for their medically ill patients.
Finally, this pilot study has several limitations, including a small sample size, lack of randomization, and clinical ratings that were based on retrospective chart review. Larger controlled studies in patients with delirium are warranted to explore these preliminary observations and conclusions.
Drug names: chlorpromazine (Thorazine and others), haloperidol (Haldol and others), olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal).
Footnotes
Supported in part by AstraZeneca.
REFERENCES
- Lipowski ZJ. Delirium (acute confusional states) JAMA. 1987;258:1789–1792. [PubMed] [Google Scholar]
- Practice Guideline for the Treatment of Patients With Delirium. Am J Psychiatry. 1999;156(5 suppl):1–20. [PubMed] [Google Scholar]
- Massie MJ, Holland J, Glass E. Delirium in terminally ill cancer patients. Am J Psychiatry. 1983;140:1048–1050. doi: 10.1176/ajp.140.8.1048. [DOI] [PubMed] [Google Scholar]
- Van Hemert AM, Van Der Mast RC, Hengeveld MW, et al. Excess mortality in general hospital patients with delirium: a five year follow up of 519 patients seen in psychiatric consultation. J Psychosom Res. 1994;38:339–346. doi: 10.1016/0022-3999(94)90038-8. [DOI] [PubMed] [Google Scholar]
- Trzepacz PT, Teague GB, Lipowski ZJ. Delirium and other organic mental disorders in a general hospital. Gen Hosp Psychiatry. 1985;7(2):101–106. doi: 10.1016/0163-8343(85)90018-0. [DOI] [PubMed] [Google Scholar]
- Weddington WW. The mortality of delirium: an underappreciated problem. Psychosomatics. 1982;3:1232–1235. doi: 10.1016/S0033-3182(82)73269-4. [DOI] [PubMed] [Google Scholar]
- Tesar GE, Murray GB, Cassem NH. Use of high-dose intravenous haloperidol in the treatment of agitated cardiac patients. J Clin Psychopharmacol. 1985;5:344–347. [PubMed] [Google Scholar]
- Sipahimalani A, Sime RM, Masand PS. Treatment of delirium with risperidone. Int J Geriatr Psychopharmacol. 1997;1:24–26. [Google Scholar]
- Ravona-Springer R, Dolbert OT, Hirschmann S, et al. Delirium in elderly patients treated with risperidone: a report of three cases [letter] J Clin Psychopharmacol. 1998;18:171–172. doi: 10.1097/00004714-199804000-00011. [DOI] [PubMed] [Google Scholar]
- Sipahimalani A, Masand PS. Olanzapine in the treatment of delirium. Psychosomatics. 1998;39:422–430. doi: 10.1016/S0033-3182(98)71301-5. [DOI] [PubMed] [Google Scholar]
- Trzepacz PT, Baker RW, Greenhouse J. A symptom rating scale for delirium. Psychiatry Res. 1988;23:89–97. doi: 10.1016/0165-1781(88)90037-6. [DOI] [PubMed] [Google Scholar]
- Masand PS. Using newer antipsychotic agents in primary care. Primary Psychiatry. 1997;58:64–68. [Google Scholar]