Abstract
Anxiety disorders are widely prevalent but insufficiently recognized and inadequately treated in primary care practice. The annual costs of morbidity and mortality of these disorders approach $50 billion, substantially more than costs for schizophrenia or all affective disorders combined. Somatization of anxiety contributes to the challenges of making an accurate diagnosis and to the indirect costs associated with delaying appropriate treatment. Pharmacologic interventions give clinicians the necessary tools to treat anxiety safely and effectively. Former therapeutic choices were limited to benzodiazepines, buspirone, and older antidepressants, but newer anxiolytic agents have become available. The selective serotonin reuptake inhibitors and agents with dual reuptake inhibition, such as venlafaxine XR, are optimizing therapy and yielding less risk for serious adverse events, greater safety in long-term therapy, and opportunity for improved patient compliance. These newer antidepressants provide substantial efficacy in patients with comorbid anxiety and depression, commonly seen in the primary care setting.
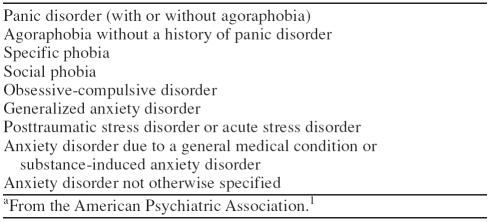
Anxiety disorders are a diverse range of psychiatric conditions (Table 1) characterized by clinically significant levels of worry, apprehension, or panic that occur in the absence of or out of proportion to specific causes (such as physical danger or public speaking) that are normally associated with such feelings.1–3 The emotional distress of anxiety is often accompanied by specific physical symptoms associated with a state of autonomic arousal, such as sweating, dizziness, and shortness of breath (most notable in patients with panic attacks), or more generalized somatic complaints, such as insomnia, restlessness, and muscle aches (commonly found in patients with generalized anxiety disorder [GAD]).1–3 Other primary anxiety disorders include phobic disorders (social or specific), obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and acute stress disorder. In addition, many medical conditions are associated with anxiety, particularly among older patients; these include neurologic conditions, thyroid dysfunction, and cardiovascular disease.1,4 Drug use or abuse, including benzodiazepine (BZD) and alcohol withdrawal or intoxication, also have been linked to clinically significant anxiety that should be distinguished carefully from medically related causes1 before a course of treatment is considered.
Table 1.
DSM-IV Classification of Anxiety Disordersa
It is estimated that approximately 27 million Americans have an anxiety disorder at some time in their lives.5 In a recent screening study conducted in the United States,6 the lifetime prevalence of a diagnosable anxiety disorder was 23.9% in a primary care setting. This figure concurs with data from the National Comorbidity Survey,7 which showed a lifetime prevalence of 24.9%. Among the categories of anxiety disorders,1 specific phobias appear to be the most common, with a lifetime prevalence of 9.8%, and OCD is the least common, with a lifetime prevalence of 2.3%.6 In general, the prevalence of anxiety disorders is higher in people younger than 65 years than in their older counterparts. Rates are also higher in women than in men, although the difference is much less pronounced for OCD, in which the rates in men are almost equal to those in women.8
Appropriate screening, diagnosis, and treatment are particularly important because a large proportion of patients with anxiety disorders will be seen initially by a generalist physician in the primary care setting.6 These patients often present a number of clinical challenges. In general, patients with anxiety fare substantially worse than patients with other psychiatric conditions, such as depression, even when they receive an accurate diagnosis and appropriate treatment.9 Because both anxiety and depression commonly manifest as nonspecific distress (e.g., mild sleep or appetite disturbances), it is not unusual for anxious patients seen in the primary care setting to receive a misdiagnosis of depression.6,10 This finding is further complicated by the fact that patients with long-standing anxiety may develop symptoms of depression over time.9 However, anxiety disorders generally can be distinguished from depressive states. In anxiety states, increased vasomotor responsiveness, as well as panic attacks, phobias, derealization, and perceptual dysfunctions, are frequently seen.9 In contrast, the general affect in depression is mostly negative, often associated with loss of interest and pleasure (anhedonia), hopelessness, emotional withdrawal, and fatigue.10 However, as we shall see, the diagnostic distinction between anxiety disorders and depression has become less important as the treatments have become more similar.
SOMATIZATION OF ANXIETY AMONG PRIMARY CARE PATIENTS
Somatization refers to the phenomenon in which patients experience and express their feelings or emotions through physical complaints and distress.11 This phenomenon may result from a variety of cultural, familial, and personal circumstances, including biases against expressing psychological discomfort.12 Patients may fear being stigmatized if they are labeled with a psychiatric disorder, or they may be concerned about their physician's response to nonsomatic complaints.13 Although the term somatization is generally used, it needs to be differentiated from somatization disorder, which is recognized as a distinct clinical psychiatric disorder.1 A study in 425 primary care patients found that anxiety disorders were associated with a significantly higher rate of comorbid somatization disorder than that observed in the absence of anxiety disorders.6
Symptoms typically associated with somatization of anxiety and other psychiatric disorders include abdominal pain, dyspepsia, chest pain, fatigue, dizziness, insomnia, and headache.12,14,15 Such symptoms, occurring either alone or in various combinations, are among the most common reasons for nearly half of all primary care visits among the general population.15 A study in 1000 primary care patients found that at least 1 of these symptoms was reported by 38% of the patients, but in only 16% did the symptoms correlate with an organic disease over a 3-year period.14 Other data, also derived from a primary care population, suggested a strong association between the number of medically unexplained symptoms experienced by patients and the likelihood of a concurrent anxiety or depressive disorder.15 For example, if 7% of patients with 2 or 3 physical symptoms were found to have a diagnosable anxiety disorder, the incidence almost doubled (13%) in those with 4 or 5 somatic complaints and increased to 48% in patients with 9 or more physical symptoms.15
In the primary care setting, somatization of anxiety has important implications for identifying patients who have an anxiety disorder. It has been estimated that as many as 53% of patients who meet the criteria for a psychiatric disorder may receive an incorrect diagnosis in this setting.16 Clinicians may falsely attribute the somatic complaints to an underlying medical condition or, when diagnostic tests reveal no organic cause for the symptoms, may fail to look for a psychiatric cause. In a study conducted in Great Britain,17 primary care physicians were able to diagnose anxiety, depression, or both significantly more often in patients who had psychiatric symptoms than in patients who had only somatic complaints. A similar study in the United States showed that only 22% of anxious or depressed patients with somatic manifestations received correct diagnoses by their family physicians, compared with 77% of patients who had psychiatric symptoms.18 These data suggest that patients' somatic complaints may often lead to an overlooked diagnosis of anxiety as the primary source of the discomfort.
Another confounding factor in the timely and accurate diagnosis of anxiety is the high rate of medical and psychiatric comorbidity in patients with anxiety. Depression may occur in as many as 60% of patients with GAD or panic disorder.19 In some cases, this comorbidity may manifest as mixed anxiety-depression, a condition that is characterized by subsyndromal levels of both anxiety and depression.1 Comorbid anxiety and depression is associated with significantly greater psychopathology and early withdrawal from treatment than either disorder alone.19 In addition, coexisting depression and anxiety portends a worse prognosis, with less robust responses to treatment and a greater risk of suicide, than either disorder alone.6,20
Aside from the presence of unexplained somatic complaints and the high rate of psychiatric comorbidities, anxiety is also frequently associated with comorbid medical illnesses. Anxiety itself may be a factor in provoking or maintaining medical conditions or diseases.13 A survey of primary care patients found that those who experienced panic attacks had a significantly higher rate of hypertension than those who did not.13 Left untreated, anxiety may prolong or worsen a medical illness.21
Not surprisingly, undiagnosed or misdiagnosed anxiety is a major contributor to high use of health care resources and excessive health care costs, even after adjusting for comorbid medical conditions.22 Data collected in 1990 indicated that the total costs of anxiety disorders in the United States, including direct costs for hospitalizations and professional services and indirect costs related to morbidity and mortality, reached approximately $46 billion, one third of the total cost for all mental disorders.23 These costs associated with anxiety disorders were higher than those for schizophrenia ($32 billion), affective disorders ($30 billion), and other combined mental disorders ($38 billion). The greatest proportion of the cost of anxiety (nearly three quarters) is attributed to lost or reduced productivity, and the remainder is attributed to the direct costs of medical treatment.5
Somatization also contributes to the high cost of anxiety. Medical workups can be extensive and delay treatment of symptoms. Anxious patients may undergo unnecessary tests or procedures and be referred to various medical specialists before an appropriate psychiatric consultation is sought or a diagnosis is made.13 High users of health care resources are substantially more likely to have an underlying anxiety disorder: as many as 40% have a lifetime history of GAD, and 20% have somatization disorder.24 High medical-resource utilization and overall costs may be especially problematic in patients with panic disorder because of the somatic symptoms such as tachycardia and hypertension associated with a panic attack. These patients are often referred for costly cardiovascular or neurologic tests such as Holter monitoring, exercise testing, angiography, magnetic resonance imaging, or electroencephalography.12 In addition, the use of health care resources and loss of productivity are significantly higher in patients with an anxiety disorder and a comorbid medical or psychiatric condition.25 Therefore, prompt recognition and treatment of anxiety by the primary care physician would help reduce the total cost associated with this disorder.
TREATING ANXIETY: OPTIONS FOR THE PRIMARY CARE PHYSICIAN
For many years, pharmacologic therapy for anxiety disorders was dominated by the use of BZDs, buspirone, the older tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs).26–34 More recently, newer types of antidepressants have emerged as promising alternatives for the treatment of anxiety, as a result of their robust efficacy (particularly in patients with comorbid anxiety and depression), improved safety profiles, and ease of use.33,35–44 The following sections review these agents from a clinical perspective on dose-response potential, drug-drug interaction profiles, and adverse effects.
Traditional Anxiolytic Agents
Benzodiazepines.
The BZDs have a rapid onset of action, which becomes clinically apparent within the first week of therapy.28 Many currently available BZDs appear to have equivalent anxiolytic efficacy.27 However, many clinicians favor drugs with relatively short half-lives—such as alprazolam, lorazepam, and oxazepam—over longer-acting agents because of their lower risk of sedation, psychomotor impairment (an effect that is enhanced by the intake of alcohol), and amnesic effects, probably as a result of less drug accumulation.26,27 On the other hand, drugs with long half-lives are less likely to produce an intense discontinuation syndrome, a well-characterized reaction in patients who stop therapy with BZDs, which may include symptoms such as rebound anxiety, nervousness, insomnia, restlessness, and depression.26,28,29 The duration of therapy and the rate at which the dosage is tapered off appear to contribute to the likelihood or severity of withdrawal symptoms.29 These effects substantially limit the use of BZDs in the primary care setting. Physical dependence and pharmacologic tolerance are additional risks of therapy with BZDs, particularly over the long term. Therefore, continuous treatment with BZDs requires clinical reevaluation for gradual reduction and discontinuation.27,29
Aside from alprazolam, for which higher plasma concentrations correlate with improved clinical response, no clear dose response has been demonstrated for the BZDs. Typical dosage ranges for healthy adults are 0.75 to 4.0 mg/day for alprazolam (dosages of 1.5–10 mg/day are often used in patients with panic disorder), 2 to 6 mg/day for lorazepam, and 30 to 120 mg/day for oxazepam.27 Therapy should be initiated at the lowest possible dosage, to minimize the risk of adverse effects, and should be tailored to patients' clinical and medication history, age, body size, and state of physical health.27
The duration of treatment and the dosing pattern also should be individualized. Once-daily dosing would encourage patients to comply better with treatment. Intermittent therapy may be adequate in patients with intermittent symptoms or symptoms triggered by identifiable anxiety-provoking situations. Patients experiencing persistent symptoms characteristic of an anxiety disorder, such as GAD, may require more sustained courses of therapy27 with an agent carefully selected for its efficacy and safety properties for each individual patient.45 Particular care should be exercised when using BZDs in older patients and those with organ dysfunction. Drug clearance of longer-acting agents may be impaired with age, hepatic disease, or the concomitant use of estrogens or cimetidine.26
Buspirone.
Since buspirone became available in the late 1980s, it has been used as an alternative to BZDs in certain patients. This agent appears to be somewhat more effective in reducing the psychological symptoms of anxiety than it is in treating somatic complaints, and it appears to have dose-related effects. The average therapeutic dosage is 20 to 30 mg/day.28,30 Buspirone has a slow onset of action (as long as 4 weeks for full therapeutic effect), and its anxiolytic efficacy is unclear in patients with panic disorder and reduced in those recently withdrawn from BZD therapy.30
However, buspirone is more suitable than BZDs for the treatment of chronically anxious patients. The starting dosage should be low (5 mg) and given on a 3-times-daily schedule, with incremental increases every few days. Generally, initial aggressive dosing may result in headache, dizziness, and nausea—common reasons why patients stop their medication prematurely.28 Although buspirone has an overall more favorable safety profile than the BZDs, drug discontinuation rates after 6 months are higher with buspirone, suggesting less patient satisfaction.28,29 Finally, as with the BZDs, care should be taken to avoid drug-drug interactions with buspirone: levels of diazepam or haloperidol may increase during concomitant therapy, and levels of buspirone may increase in the presence of cimetidine and in patients with renal disease.26,46
Tricyclic antidepressants and monoamine oxidase inhibitors.
The TCAs and MAOIs also have been used successfully in patients with anxiety, particularly in panic disorder and in those with coexisting depression. Their overall use in primary care, however, is limited by their associated adverse events, safety issues in terms of lethality in overdosage, and, particularly with the MAOIs, significant adverse interactions with foods and drugs.32–34 The TCAs are associated with notable anticholinergic side effects such as dry mouth, blurred vision, and constipation, which generally do not abate during therapy.39 Patients often find these effects intolerable and may discontinue treatment as a result.29,39 Because TCAs can cause agitation in anxious patients, initial dosages should be very low. In addition, their use in anxious patients with suicidal tendencies should be avoided because of their potential for lethal overdosing—amounts as small as a 1-week's supply of amitriptyline or imipramine can be lethal.39,47
Newer Antidepressants in the Treatment of Anxiety
The selective serotonin reuptake inhibitors (SSRIs) have been evaluated extensively in the treatment of anxiety disorders, particularly panic disorder32,35 and comorbid anxiety and depression,33,36,39 although their acceptance by the clinical community preceded the results of formal research to demonstrate their anxiolytic efficacy.32 The more favorable safety and tolerability profiles of the SSRIs are responsible for their preference over the TCAs and MAOIs.39
A growing body of data now suggests that venlafaxine extended release (XR), which acts by blocking the reuptake of both serotonin and norepinephrine, is also efficacious for treating patients with an anxiety disorder40–42,48–51 and, possibly, mixed anxiety-depression.43,44 Short- and long-term studies in patients meeting DSM-IV criteria for GAD showed venlafaxine XR to be more effective than placebo48–51 and, to a statistically significant degree, buspirone.48 Venlafaxine XR appears to have one of the most favorable drug-drug interaction profiles relative to those of other antidepressants because it lacks any significant inhibitory effect on the cytochrome P450 isoenzyme system.52
In general, these newer antidepressants are considerably safer than the BZDs in sedative effects, withdrawal liability, and psychomotor impairment, and they lack the anticholinergic effects and risk of overdosage of the TCAs. Nausea, headache, insomnia, and somnolence (usually transient) are among the most prominent adverse events noted with these agents.39,53,54 In addition to these effects, some sexual dysfunction has been reported with the use of many of the newer antidepressants.39,53,55 On the other hand, the use of some SSRIs, such as fluoxetine, has been associated with paradoxic anxiety, jitteriness, and nervousness, which may require a short course of therapy with a BZD39 or starting with a low dosage of the SSRI.
In efficacy, the SSRIs appear to be equivalent to the TCAs in treating anxiety.32,33 As is the case with the TCAs and buspirone, the SSRIs are associated with a delay in the onset of activity.30,32,34 Evidence also indicates that the SSRIs may reduce the psychological symptoms of anxiety without improving the somatic symptoms.56 In contrast, data from studies have shown that venlafaxine XR significantly improves both psychological and somatic symptoms of anxiety in patients with GAD alone and in those with comorbid anxiety and depression, suggesting that this agent may be particularly useful in patients with these types of anxiety disorders.44,48–51,57 Both the SSRIs and venlafaxine XR can be taken once daily, which enhances convenience for patients, increasing their compliance and possibly increasing their ability to achieve remission and full resolution of symptoms.
CONCLUSIONS
Primary care physicians have an ever-widening array of pharmacologic therapies to use in treating patients with anxiety or mixed anxiety-depression. Compared with the standard anxiolytic agents, the newer antidepressants offer a number of important advantages in this setting. Agents such as the SSRIs and dual reuptake inhibitors are safer in overdosage, more pharmacologically suited to treating anxiety and mixed anxiety-depression, and better tolerated than the older agents. The characteristics of individual agents that may help guide clinical decisions about which agent to use for a particular patient include the risk of drug-drug interactions, specific side effect profiles, and the presence of coexisting medical or psychiatric disorders.
Drug names: alprazolam (Xanax and others), amitriptyline (Elavil and others), buspirone (BuSpar), cimetidine (Tagamet and others), diazepam (Valium and others), fluoxetine (Prozac), haloperidol (Haldol and others), lorazepam (Ativan and others), oxazepam (Serax and others), venlafaxine XR (Effexor XR).
Footnotes
Supported by an unrestricted educational grant from Wyeth-Ayerst Laboratories, Philadelphia, Pa.
Financial disclosure: Dr. Gelenberg has received grant/research support from Bristol-Myers Squibb, Organon, Pfizer, Lilly Research Laboratories, Janssen, Merck Sharp & Dohme, SmithKline Beecham, Wyeth-Ayerst, Hoechst Marion Roussel, and Forest Laboratories; is on the speakers' bureaus for Bristol-Myers Squibb, Pfizer, SmithKline Beecham, Janssen, Lilly, Forest Laboratories, and Parke-Davis; has stock or other ownership interest in Pfizer, Warner-Lambert, and Eli Lilly; and has received consultant fees from Eli Lilly, SCIOS, Forest Laboratories, Parke-Davis, Pfizer, Janus Pharmaceuticals, Best Practice, and Bristol-Myers Squibb.
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association. 1994 [Google Scholar]
- Martin LM, Fleming KC, Evans JM. Recognition and management of anxiety and depression in elderly patients. Mayo Clin Proc. 1995;70:999–1006. doi: 10.4065/70.10.999. [DOI] [PubMed] [Google Scholar]
- Burke WJ, Folks DG, McNeilly DP. Effective use of anxiolytics in older adults. Clin Geriatr Med. 1998;14:47–65. [PubMed] [Google Scholar]
- Small GW. Recognizing and treating anxiety in the elderly. J Clin Psychiatry. 1997;58(suppl 3):41–47. [PubMed] [Google Scholar]
- DuPont RL, Rice DP, Miller LS, et al. Economic costs of anxiety disorders. Anxiety. 1996;2:167–172. doi: 10.1002/(SICI)1522-7154(1996)2:4<167::AID-ANXI2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Nisenson LG, Pepper CM, Schwenk TL, et al. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. 1998;20:21–28. doi: 10.1016/s0163-8343(97)00096-0. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151:640–649. doi: 10.1176/ajp.151.5.640. [DOI] [PubMed] [Google Scholar]
- Schapira K, Roth M, Kerr TA, et al. The prognosis of affective disorders: the differentiation of anxiety states from depressive illnesses. Br J Psychiatry. 1972;121:175–181. doi: 10.1192/bjp.121.2.175. [DOI] [PubMed] [Google Scholar]
- Keller MB, Hanks DL. Anxiety symptom relief in depression treatment outcomes. J Clin Psychiatry. 1995;56(suppl 6):22–29. [PubMed] [Google Scholar]
- Baughman OL III. Rapid diagnosis and treatment of anxiety and depression in primary care: the somatizing patient. J Fam Pract. 1994;39:373–378. [PubMed] [Google Scholar]
- Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59(suppl 20):15–21. [PubMed] [Google Scholar]
- Zajecka J. Importance of establishing the diagnosis of persistent anxiety. J Clin Psychiatry. 1997;58(suppl 3):9–13. [PubMed] [Google Scholar]
- Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, et al. Physical symptoms in primary care: predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- Ormel J, Koeter MWJ, van den Brink W, et al. Recognition, management, and course of anxiety and depression in general practice. Arch Gen Psychiatry. 1991;48:700–706. doi: 10.1001/archpsyc.1991.01810320024004. [DOI] [PubMed] [Google Scholar]
- Bridges KW, Goldberg DP. Somatic presentation of DSM-III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Robbins JM, Dworkind M, et al. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–741. doi: 10.1176/ajp.150.5.734. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, et al. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry. 1996;153:1293–1300. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Gorman JM. Comorbid depression and anxiety spectrum disorders. Depress Anxiety. 1996/1997;4:160–168. doi: 10.1002/(SICI)1520-6394(1996)4:4<160::AID-DA2>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Rogers MP, White K, Warshaw MG, et al. Prevalence of medical illness in patients with anxiety disorders. Int J Psychiatry Med. 1994;24:83–96. doi: 10.2190/TXM9-EVX8-Q4WT-G03J. [DOI] [PubMed] [Google Scholar]
- Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152:352–357. doi: 10.1176/ajp.152.3.352. [DOI] [PubMed] [Google Scholar]
- Rice DP, Miller LS. Health economics and cost implications of anxiety and other mental disorders in the United States. Br J Psychiatry. 1998;173(suppl 34):4–9. [PubMed] [Google Scholar]
- Katon W, VonKorff M, Lin E, et al. Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- Souêtre E, Lozet H, Cimarosti I, et al. Cost of anxiety disorders: impact of comorbidity. J Psychosom Res. 1994;38(suppl 1):151–160. doi: 10.1016/0022-3999(94)90145-7. [DOI] [PubMed] [Google Scholar]
- Dubovsky SL. Generalized anxiety disorder: new concepts and psychopharmacologic therapies. J Clin Psychiatry. 1990;51(1, suppl):3–10. [PubMed] [Google Scholar]
- Shader RI, Greenblatt DJ. Use of benzodiazepines in anxiety disorders. N Engl J Med. 1993;328:1398–1405. doi: 10.1056/NEJM199305133281907. [DOI] [PubMed] [Google Scholar]
- Schweizer E, Rickels K. Strategies for treatment of generalized anxiety in the primary care setting. J Clin Psychiatry. 1997;58(suppl 3):27–31. [PubMed] [Google Scholar]
- Schweizer E. Generalized anxiety disorder: longitudinal course and pharmacologic treatment. Psychiatr Clin North Am. 1995;18:843–857. [PubMed] [Google Scholar]
- Sussman N. The uses of buspirone in psychiatry. J Clin Psychiatry Monograph. 1994;12(1):3–19. [Google Scholar]
- Sramek JJ, Tansman M, Suri A, et al. Efficacy of buspirone in generalized anxiety disorder with coexisting mild depressive symptoms. J Clin Psychiatry. 1996;57:287–291. [PubMed] [Google Scholar]
- Jefferson JW. Antidepressants in panic disorder. J Clin Psychiatry. 1997;58(suppl 2):20–25. [PubMed] [Google Scholar]
- Tollefson GD, Holman SL, Sayler ME, et al. Fluoxetine, placebo, and tricyclic antidepressants in major depression with and without anxious features. J Clin Psychiatry. 1994;55:50–59. [PubMed] [Google Scholar]
- Rickels K, Downing R, Schweizer E, et al. Antidepressants for the treatment of generalized anxiety disorder: a placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry. 1993;50:884–895. doi: 10.1001/archpsyc.1993.01820230054005. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K. The role of SSRIs in panic disorder. J Clin Psychiatry. 1996;57(suppl 10):51–58. [PubMed] [Google Scholar]
- Sheehan D, Dunbar GC, Fuell DL. The effect of paroxetine on anxiety and agitation associated with depression. Psychopharmacol Bull. 1992;28:139–143. [PubMed] [Google Scholar]
- Katzelnick DJ, Kobak KA, Greist JH, et al. Sertraline for social phobia: a double-blind, placebo-controlled crossover study. Am J Psychiatry. 1995;152:1368–1376. doi: 10.1176/ajp.152.9.1368. [DOI] [PubMed] [Google Scholar]
- Rocca P, Fonzo V, Scotta M, et al. Paroxetine efficacy in the treatment of generalized anxiety disorder. Acta Psychiatr Scand. 1997;95:444–450. doi: 10.1111/j.1600-0447.1997.tb09660.x. [DOI] [PubMed] [Google Scholar]
- Kuzel RJ. Treating comorbid depression and anxiety. J Fam Pract. 1996;43(6, suppl):S45–S53. [PubMed] [Google Scholar]
- Kelsey JE. Venlafaxine in social phobia. Psychopharmacol Bull. 1995;31:767–771. [PubMed] [Google Scholar]
- Pollack MH, Worthington JJ III, Otto MW, et al. Venlafaxine for panic disorder: results from a double-blind, placebo-controlled study. Psychopharmacol Bull. 1996;32:667–670. [PubMed] [Google Scholar]
- Geracioti TD Jr. Venlafaxine treatment of panic disorder: a case series. J Clin Psychiatry. 1995;56:408–410. [PubMed] [Google Scholar]
- Zajecka JM, Fawcett J, Guy C. Coexisting major depression and obsessive-compulsive disorder treated with venlafaxine [letter] J Clin Psychopharmacol. 1990;10:152–153. doi: 10.1097/00004714-199004000-00033. [DOI] [PubMed] [Google Scholar]
- Khan A, Upton GV, Rudolph RL, et al. The use of venlafaxine in the treatment of major depression and major depression associated with anxiety: a dose-response study. J Clin Psychopharmacol. 1998;18:19–25. doi: 10.1097/00004714-199802000-00004. [DOI] [PubMed] [Google Scholar]
- Richelson E. Pharmacokinetic drug interactions of new antidepressants: a review of the effects on the metabolism of other drugs. Mayo Clin Proc. 1997;72:835–847. doi: 10.4065/72.9.835. [DOI] [PubMed] [Google Scholar]
- Sussman N. Treatment of anxiety with buspirone. Psychiatr Ann. 1987;17:114–117. 120. [Google Scholar]
- Nemeroff CB. Evolutionary trends in the pharmacotherapeutic management of depression. J Clin Psychiatry. 1994;55(12, suppl):3–15. [PubMed] [Google Scholar]
- Davidson JRT, DuPont RL, Hedges D, et al. Efficacy, safety, and tolerability of venlafaxine extended release and buspirone in outpatients with generalized anxiety disorder. J Clin Psychiatry. 1999;60:528–535. doi: 10.4088/jcp.v60n0805. [DOI] [PubMed] [Google Scholar]
- Hackett D, Parks V, and Salinas E. A 6-month evaluation of 3 dose levels of venlafaxine extended-release in non-depressed outpatients with generalized anxiety disorder [poster]. Presented at the 19th annual conference of the Anxiety Disorders Association of America; March 25–28, 1999; San Diego, Calif. [Google Scholar]
- Haskins JT, Rudolph R, Aguiar L, and et al. Venlafaxine XR is an efficacious short- and long-term treatment for generalized anxiety disorder [poster]. Presented at the 11th annual Congress of the European College of Neuropsychopharmacology; Oct 31–Nov 4, 1998; Paris, France. [Google Scholar]
- Haskins T, Rudolph R, Pallay A, and et al. Double-blind, placebo-controlled study of once daily venlafaxine XR in outpatients with generalized anxiety disorder (GAD) [poster]. Presented at the 21st annual meeting of the Collegium Internationale Neuro-Psychopharmacologicum; July 12–16, 1998; Glasgow, Scotland. [Google Scholar]
- Ereshefsky L. Drug-drug interactions involving antidepressants: focus on venlafaxine. J Clin Psychopharmacol. 1996;16(3, suppl 2):37S–53S. doi: 10.1097/00004714-199606002-00009. [DOI] [PubMed] [Google Scholar]
- Hedges DW, Reimherr FW, Strong RE, et al. An open trial of nefazodone in adult patients with generalized anxiety disorder. Psychopharmacol Bull. 1996;32:671–676. [PubMed] [Google Scholar]
- Ballenger JC. Clinical evaluation of venlafaxine. J Clin Psychopharmacol. 1996;16(3, suppl 2):29S–36S. doi: 10.1097/00004714-199606002-00007. [DOI] [PubMed] [Google Scholar]
- Thase ME. for the Venlafaxine XR 209 Study Group. Efficacy and tolerability of once-daily venlafaxine extended release (XR) in outpatients with major depression. J Clin Psychiatry. 1997 58:393–398. [DOI] [PubMed] [Google Scholar]
- Hoehn-Saric R, McLeod DR, Zimmerli WD. Differential effects of alprazolam and imipramine in generalized anxiety disorder: somatic versus psychic symptoms. J Clin Psychiatry. 1988;49:293–301. [PubMed] [Google Scholar]
- Feighner JP, Entsuah AR, McPherson MK. Efficacy of once-daily venlafaxine extended release (XR) for symptoms of anxiety in depressed outpatients. J Affect Disord. 1998;47:55–62. doi: 10.1016/s0165-0327(97)00109-2. [DOI] [PubMed] [Google Scholar]