Abstract
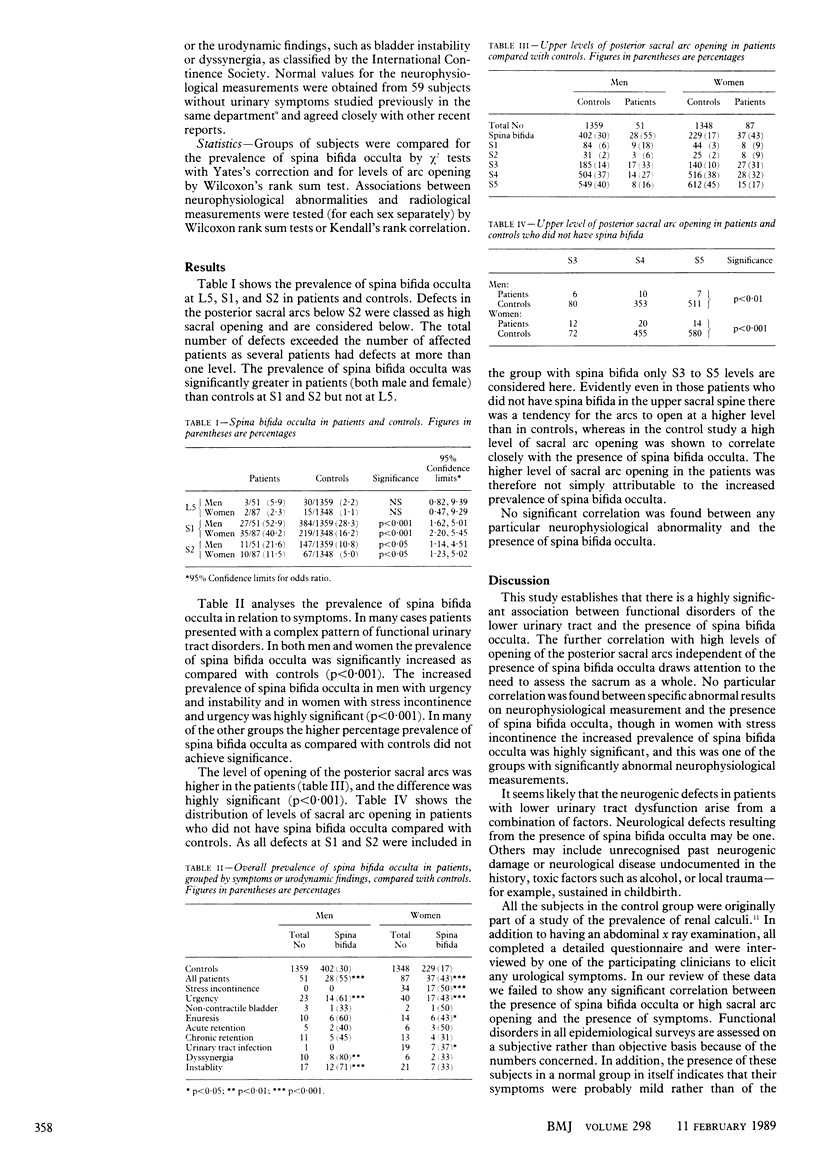
OBJECTIVE--To determine the relation between neurophysiological abnormalities and the radiological detection of spina bifida occulta in patients with dysfunction of the lower urinary tract. DESIGN--Blind assessment and subsequent decoding of mixed batch of abdominal radiographs from patients with and without urological symptoms for evidence of spina bifida occulta and comparison of results with those of previous control series. SETTING--Review study among tertiary referrals to an incontinence clinic of a city hospital. PATIENTS--One hundred and thirty eight adults with proved urodynamic abnormalities in whom neurophysiological measurements were available. INTERVENTIONS--None. END POINT--Correlation of neurophysiological abnormalities in lower urinary tract dysfunction with presence and type of spina bifida occulta and level of opening of posterior sacral arcs. MEASUREMENTS AND MAIN RESULTS--On decoding radiographs those from patients without urological symptoms showed a similar prevalence of spina bifida occulta to that in the control series (631/2707 controls; 23%). By contrast, patients with urological symptoms had a significantly increased prevalence of spina bifida occulta at S1 and S2 and a higher level of opening of posterior sacral arcs. The increased prevalence of the bony defect was particularly striking in men with urgency and instability and in women with stress incontinence. No significant correlation was found between any particular neurophysiological abnormality and the presence of spina bifida. CONCLUSIONS--In patients with dysfunction of the lower urinary tract neurophysiological abnormalities may be associated with congenital dysraphic lesions in the lower lumbar spine and sacrum. There appears to be no direct causal relation between the radiological and neurophysiological abnormalities but the findings suggest a common aetiological factor.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COWIE T. N. Congenital spinal deformities of surgical importance. Acta radiol. 1956 Jul-Aug;46(1-2):38–47. doi: 10.3109/00016925609170810. [DOI] [PubMed] [Google Scholar]
- Fidas A., Elton R. A., McInnes A., Chisholm G. D. Neurophysiological measurement of the voiding reflex arcs in patients with functional disorders of the lower urinary tract. Br J Urol. 1987 Sep;60(3):205–211. doi: 10.1111/j.1464-410x.1987.tb05484.x. [DOI] [PubMed] [Google Scholar]
- Fidas A., Galloway N. T., McInnes A., Chisholm G. D. Neurophysiological measurements in primary adult enuretics. Br J Urol. 1985 Dec;57(6):635–640. doi: 10.1111/j.1464-410x.1985.tb07022.x. [DOI] [PubMed] [Google Scholar]
- Fidas A., MacDonald H. L., Elton R. A., Wild S. R., Chisholm G. D., Scott R. Prevalence and patterns of spina bifida occulta in 2707 normal adults. Clin Radiol. 1987 Sep;38(5):537–542. doi: 10.1016/s0009-9260(87)80150-2. [DOI] [PubMed] [Google Scholar]
- Galloway N. T., Tainsh J. Minor defects of the sacrum and neurogenic bladder dysfunction. Br J Urol. 1985 Apr;57(2):154–155. doi: 10.1111/j.1464-410x.1985.tb06410.x. [DOI] [PubMed] [Google Scholar]
- Lemire R. J., Beckwith J. B. Pathogenesis of congenital tumors and malformations of the sacrococcygeal region. Teratology. 1982 Apr;25(2):201–213. doi: 10.1002/tera.1420250209. [DOI] [PubMed] [Google Scholar]
- SOUTHWORTH J. D., BERSACK S. R. Anomalies of the lumbosacral vertebrae in 550 individuals without symptoms referable to the low back. Am J Roentgenol Radium Ther. 1950 Oct;64(4):624–634. [PubMed] [Google Scholar]
- Scott R., Freeland R., Mowat W., Gardiner M., Hawthorne V., Marshall R. M., Ives J. G. The prevalence of calcified upper urinary tract stone disease in a random population--Cumbernauld Health Survey. Br J Urol. 1977;49(7):589–595. doi: 10.1111/j.1464-410x.1977.tb04536.x. [DOI] [PubMed] [Google Scholar]


