Abstract
In the wake of fears over pandemic influenza, triggered by concern about avian influenza, a top national priority is to adapt surveillance systems, such as Biosense, for influenza monitoring. While real time surveillance system architects have been largely focused on the problem of discrete outbreak detection, the data in these systems have been shown to have unique advantages for the timely detection of influenza. In this study, we evaluate the utility influenza detection by real-time surveillance as an adjunct to the traditional CDC surveillance systems.
Methodology
Using the Massachusetts Department of Public Health AEGIS surveillance system, we tracked influenza activity through five years using respiratory chief complaint data from emergency department visits at six hospitals in metropolitan Boston. We compared timeliness and prediction of this system to two traditional systems: pneumonia and influenza (P&I) mortality in New England from the CDC 121 Cities Mortality Reporting System and excess influenza-like illness (ILI) in Boston from the CDC Influenza Sentinel Providers Surveillance Network. To evaluate the utility of this system for early warning of influenza epidemics, we tested alerting threshold algorithms, including the use of a stable baseline, a seasonal baseline and the rate of increase of influenza illness. These were compared to a gold standard of influenza viral isolate collection data.
Evaluation Results
Influenza morbidity from real-time surveillance data provides the earliest warning of influenza activity. Though the timing of influenza seasons varies from year to year, influenza morbidity from the real-time surveillance system consistently peaks prior to ILI and P&I. Using cross-correlation, we find that real-time data significantly leads P&I surveillance by three weeks (r=0.4; P<0.001) and ILI surveillance by one week (r=0.769; P<0.001). Real-time influenza data also significantly predicts oncoming ILI (r2=0.59; P<0.001) and P&I (r2=0.22; P<0.001). We also find that the use of a seasonal baseline for defining the alert threshold provides the best combination of timeliness (4 weeks) and prediction (r2=0.35; P<0.001).
Conclusions
Our analysis shows that real-time surveillance data can be effectively leveraged to monitor influenza epidemics. Our findings are particularly significant given mounting concern of pandemic influenza where increased early detection may provide critical lead time for public health action. This work is among the first to demonstrate the direct practical application of syndromic surveillance methods to influenza monitoring.
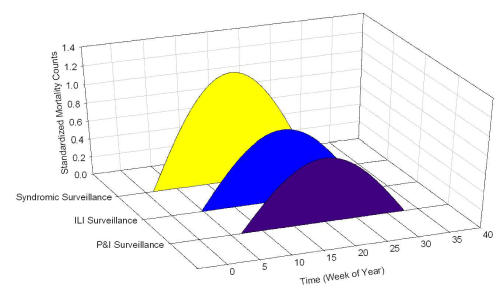
Figure 1.
Timing of influenza activity in 3 systems. Analysis shows that syndromic surveillance provides the earliest indication of an influenza season.
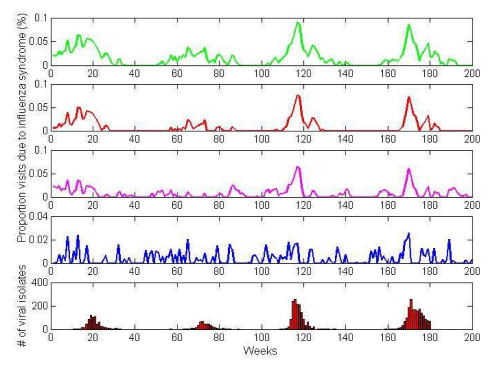
Figure 2.
Alerting algorithms used for monitoring influenza epidemics. Four thresholds were tested (1) Mean + 1 SD (green) (2) Mean + 2 SD (red) (3) Seasonal baseline (4) Percent increase (blue) and were compared to viral isolate data (red bars).