Abstract
Background
Although current guidelines emphasize the importance of cholesterol knowledge, little is known about accuracy of this knowledge, factors affecting accuracy, and the relationship of self-reported cholesterol with cardiovascular disease (CVD).
Methods
The 39,876 female health professionals with no prior CVD in the Women’s Health Study were asked to provide self-reported and measured levels of total and high-density lipoprotein (HDL) cholesterol. Demographic and cardiovascular risk factors were considered as determinants of awareness and accuracy. Accuracy was evaluated by the difference between reported and measured cholesterol. In addition, we examined the relationship of self-reported cholesterol with incident CVD over 10 years.
Results
Compared with women who were unaware of their cholesterol levels, aware women (84%) had higher levels of income, education, and exercise and were more likely to be married, normal in weight, treated for hypertension and hypercholesterolemia, nonsmokers, moderate drinkers, and users of hormone therapy. Women underestimated their total cholesterol by 9.7 mg/dL (95% CI: 9.2–10.2); covariates explained little of this difference (R2 < .01). Higher levels of self-reported cholesterol were strongly associated with increased risk of CVD, which occurred in 741 women (hazard ratio 1.23/40 mg/dL cholesterol, 95% CI: 1.15–1.33). Women with elevated cholesterol who were unaware of their level had particularly increased risk (HR=1.88, P <. 001) relative to aware women with normal measured cholesterol.
Conclusion
Women with obesity, smoking, untreated hypertension, or sedentary lifestyle have decreased awareness of their cholesterol levels. Self-reported cholesterol underestimates measured values, but is strongly related to CVD. Lack of awareness of elevated cholesterol is associated with increased risk of CVD.
KEY WORDS: cardiovascular disease, cholesterol, risk factors, self-report, women
INTRODUCTION
The National Cholesterol Education Program (NCEP) initiatives have emphasized the importance of cholesterol knowledge, recommending routine cholesterol testing for all adults older than 20.1,2 Similarly, Healthy People 20103 aims to improve the health of Americans through increased awareness of medical conditions and risk factors and greater use of screening services. Several studies4–8 have indicated that cholesterol awareness has increased with time but that it remains low among the general population. Furthermore, only limited information is available on determinants of cholesterol knowledge.
Many population studies, including the Behavioral Risk Factor Surveillance System4,9,10 and the American Heart Association National Survey,7,11 have used self-reported cholesterol levels as a screening tool to assess trends in dyslipidemia and the performance of cardiovascular risk screening programs. Thus, evaluation of the agreement between self-reported and measured cholesterol levels is important. Some studies6,12–18 have examined the validity of self-reported hypercholesterolemia and showed low sensitivity and frequent underestimation. However, little is known about predictors of accuracy and whether self-reported cholesterol levels differ systematically from measured levels across subgroups. Furthermore, in light of concerns about the accuracy of self-reported cholesterol, the ability of self-reported cholesterol to predict future cardiovascular disease (CVD) merits evaluation.
This study assessed awareness and determinants of cholesterol knowledge among 39,876 US female health professionals in the Women’s Health Study. We evaluated the validity of self-reported cholesterol levels and describe the demographic characteristics and cardiovascular risk factors influencing their accuracy. We also assessed the validity of self-reported cholesterol in the prediction of CVD over a period of 10 years.
METHODS
The Women’s Health Study (WHS) was a randomized, double-blind, clinical trial of low-dose aspirin and vitamin E in the primary prevention of CVD and cancer among 39,876 apparently healthy women age ≥45 years. Participants were recruited from registries of several health professions; detailed baseline characteristics are presented elsewhere.19–21 The trial and its questionnaires were approved by the Human Subjects Committee at the Brigham and Women’s Hospital.
During enrollment, between 1993 and 1996, participants were asked on the baseline questionnaires about demographic factors (age, race, education, profession, income, marital status), health characteristics, and behaviors [smoking status, alcohol use, physical activity, hormone replacement therapy (HRT) use], cardiovascular risk factors [body mass index (BMI), history of hypertension, diabetes mellitus, use of cholesterol-lowering drugs], and their total cholesterol (TC) levels. Yearly follow-up questionnaires were sent to update information on the presence of risk factors and the occurrence of incident cardiovascular events.
Self-reported Cholesterol Levels
Before randomization, participants were asked, “What is your CURRENT serum cholesterol level?” Those who had their cholesterol measured within the previous 5 years were asked to report their level in one of 14 categories (mg/dL): <140, 140–159, 160–179, 180–199, 200–219, 220–239, 240–249, 250–259, 260–269, 270–279, 280–299, 300–329, 330+, or unknown. At 48-month follow-up, women were specifically asked, “What is your most recent high-density lipoprotein (HDL) cholesterol level?” Awareness of cholesterol level was defined by a response other than unknown to the above questions. Among the 6,273 women who reported that their cholesterol level was unknown or left the question blank, 6,199 (99%) reported that they did not know their cholesterol level.
Blood Cholesterol Measurement
Participants were asked whether they would be willing to provide a venous blood sample and were mailed blood collection kits during the run-in phase. Blood samples were collected in ethylenediaminetetraacetic acid (EDTA) tubes from 28,263 randomized women (71.1% of the WHS participants) and stored in liquid nitrogen until the time of analysis. TC and HDL levels of 27,939 women (70.1%) were measured on a Hitachi 911 analyzer (Roche Diagnostics, IN) with reagents from Roche Diagnostics.21
The median time between the date of blood collection and the date of self-reported TC was 37 days (interquartile range, 4–82 days) and that between blood collection and HDL questionnaire was 48.2 months (43.4–53.1).
Outcome Measures
To evaluate the accuracy of the self-reported cholesterol levels in a risk prediction analysis, we examined data from the 24,069 women who provided both self-reported TC levels and blood samples. The participants were followed over a median of 10.1 years (interquartile range, 9.6–10.5). Annually, women (or their next of kin) who reported the occurrence of cardiovascular events were asked for consent to release relevant medical records, which were reviewed by an endpoint committee of physicians. We considered the first occurrence of a major vascular event (myocardial infarction, stroke, percutaneous transluminal coronary angioplasty, coronary artery bypass graft surgery, or death from cardiovascular causes) that was reviewed and confirmed by this committee.
STATISTICAL ANALYSIS
Awareness of Cholesterol Level
We used chi-square tests to assess differences in cholesterol awareness across categories of baseline variables. We fitted a multivariable logistic regression model with “whether or not a woman knew her cholesterol level” as a dichotomous outcome variable and categorical predictors of cholesterol awareness as independent variables. We computed the area under the receiver–operator characteristic curve as an overall measure of how well these variables predicted cholesterol awareness. A separate multivariate model was fitted after exclusion of the 74 women who left blank the question on cholesterol level.
Accuracy of Self-reported Cholesterol Versus Measured Blood Cholesterol
We used box-plots of the measured cholesterol levels within categories of self-reported cholesterol levels to characterize the distribution of cholesterol. We scored self-reported cholesterol levels with the midpoint of the reported category and calculated Pearson and Spearman correlation coefficients to examine the strength of the linear relationship between self-reported and measured blood cholesterol levels.
To describe the level of agreement, we calculated the mean difference between individuals’ self-reported and measured blood cholesterol levels and tested the significance of the difference between the measurements with a paired t-test. We used one-way analysis of variance (ANOVA) to evaluate the significance of differences for each characteristic and a multivariable linear regression model to determine whether the discrepancy between the two measurements could be explained by demographic characteristics and cardiovascular risk factors.
Predictive Ability of Self-reported Cholesterol
To assess the relationship of self-reported cholesterol with the hazard of first cardiovascular events, we considered self-reported cholesterol and measured blood cholesterol separately and jointly in Cox proportional hazards models adjusted for age. We used likelihood ratio tests to compare the predictive ability of self-reported versus measured cholesterol. We also compared categorical models with nested linear models to assess deviation from linearity. We repeated the analysis excluding women who were receiving cholesterol treatment for comparison.
We fit alternative proportional hazards models for 27,938 women who had measured TC with “whether or not a woman self-reported cholesterol” and “whether or not a woman has elevated measured cholesterol (>240 mg/dL)” as dichotomous predictors of CVD. We also examined the interaction between high cholesterol and self-reporting of cholesterol. We used SAS v.8 to perform all computations.
RESULTS
Determinants of Awareness of Cholesterol Levels
Among the 39,876 women randomized in the trial, 33,603 (84%) self-reported their TC level, whereas 6,273 were unaware of their cholesterol level. Among 38,147 women who responded at 48-month follow-up, only 10,542 specified their HDL level. The mean ages of women who reported and did not report their cholesterol at baseline were 54.7 and 54.2 years, respectively. Participants who provided blood samples also tended to be older, have higher education and income, and to be married.
Women’s cholesterol awareness improved with age up to 80 years, degree of education (except among those with doctorates), household income, and being married (Table 1). There were no significant differences among racial/ethnic groups, although confidence intervals for these effects were wide. Profession was not included in the model because it was highly correlated with education in this population.
Table 1.
Awareness of Total Cholesterol, by Baseline Characteristics
| Baseline characteristics | N* | Percent known (%) | P value† | Odds ratio‡ | 95% CI |
|---|---|---|---|---|---|
| Age (yr) | |||||
| <50 | 12,874 | 82.7 | <0.001 | 1.00 | Referent |
| 50–59 | 18,379 | 84.9 | 1.04 | (0.97, 1.12) | |
| 60–69 | 7,312 | 85.4 | 1.17 | (1.06, 1.29) | |
| 70–79 | 1,251 | 85.5 | 1.23 | (1.01, 1.49) | |
| >80 | 60 | 76.7 | 0.84 | (0.42, 1.69) | |
| Race | |||||
| White | 37,480 | 84.3 | 0.09 | 1.00 | Referent |
| Hispanic | 430 | 84.0 | 1.13 | (0.85, 1.51) | |
| African American | 909 | 82.3 | 1.06 | (0.87, 1.29) | |
| Asian American | 541 | 87.3 | 1.35 | (1.00, 1.82) | |
| American Indian/Others | 176 | 80.7 | 0.92 | (0.61, 1.40) | |
| Education | |||||
| LPN/LVN | 5,554 | 78.5 | <0.001 | 1.00 | Referent |
| 2-yr associate’s degree RN | 4,499 | 83.1 | 1.09 | (0.97, 1.22) | |
| 3–yr RN diploma program | 12,402 | 85.4 | 1.26 | (1.15, 1.39) | |
| BS | 9,044 | 85.4 | 1.21 | (1.09, 1.34) | |
| MS | 5,816 | 86.7 | 1.31 | (1.16, 1.48) | |
| Doctorate/MD | 1,890 | 85.2 | 1.03 | (0.87, 1.22) | |
| Income | |||||
| <$10,000 | 342 | 68.4 | <0.001 | 1.00 | Referent |
| $10,000–19,999 | 1,802 | 76.4 | 1.36 | (1.04, 1.79) | |
| $20,000–29,999 | 3,862 | 81.0 | 1.72 | (1.32, 2.24) | |
| $30,000–39,999 | 5,375 | 83.0 | 1.95 | (1.50, 2.55) | |
| $40,000–49,999 | 6,208 | 84.5 | 2.10 | (1.61, 2.75) | |
| $50,000–99,999 | 15,324 | 86.2 | 2.28 | (1.74, 2.97) | |
| >$100,000 | 4,678 | 86.8 | 2.20 | (1.65, 2.92) | |
| Marital status | |||||
| Married | 28,360 | 85.3 | <0.001 | 1.00 | Referent |
| Single | 2,265 | 81.3 | 0.86 | (0.76, 0.97) | |
| Divorced | 5,445 | 81.1 | 0.89 | (0.82, 0.97) | |
| Widowed | 2,579 | 82.2 | 0.96 | (0.84, 1.09) | |
| Baseline history of diabetes | |||||
| No | 38,825 | 84.3 | 0.41 | 1.00 | Referent |
| Yes | 1,027 | 83.4 | 0.94 | (0.78, 1.14) | |
| Smoking status | |||||
| Never | 20,340 | 85.6 | <0.001 | 1.00 | Referent |
| Current | 5,235 | 75.4 | 0.62 | (0.57, 0.67) | |
| Past | 14,265 | 85.7 | 0.96 | (0.89, 1.02) | |
| Hypertension | |||||
| Normotensive | 29,535 | 83.7 | <0.001 | 1.00 | Referent |
| Untreated | 4,818 | 82.3 | 0.98 | (0.90, 1.07) | |
| Treated | 5,484 | 89.0 | 1.64 | (1.47, 1.82) | |
| BMI | |||||
| <25.0 | 19,849 | 84.8 | <0.001 | 1.00 | Referent |
| 25.0–<30.0 | 12,081 | 84.5 | 0.96 | (0.90, 1.03) | |
| ≥30.0 | 7,126 | 82.3 | 0.91 | (0.84, 0.99) | |
| Lipid-lowering agents | |||||
| No | 38,608 | 83.8 | <0.001 | 1.00 | Referent |
| Yes | 1,240 | 98.8 | 14.84 | (8.39, 26.28) | |
| Alcohol | |||||
| Never/rarely | 17,982 | 83.2 | <0.001 | 1.00 | Referent |
| <2 drinks/day | 20,342 | 85.5 | 1.08 | (1.02, 1.16) | |
| ≥2 drinks/day | 1,542 | 80.7 | 0.79 | (0.68, 0.92) | |
| Exercise | |||||
| Never/rarely | 15,280 | 81.4 | <0.001 | 1.00 | Referent |
| <1/week | 7,928 | 83.6 | 1.13 | (1.05, 1.23) | |
| 1-3 times/week | 12,409 | 86.8 | 1.35 | (1.26, 1.46) | |
| ≥4 times/week | 4,239 | 88.6 | 1.56 | (1.39, 1.75) | |
| HRT | |||||
| Never | 19,087 | 80.8 | <0.001 | 1.00 | Referent |
| Past | 4,084 | 83.0 | 1.18 | (1.07, 1.31) | |
| Current | 16,625 | 88.5 | 1.70 | (1.58, 1.82) | |
| Blood sample taken | |||||
| No | 11,938 | 79.9 | <0.001 | 1.00 | Referent |
| Yes | 27,938 | 86.2 | 1.44 | (1.35, 1.53) | |
C-statistic: 0.66
*Number of women in each category may not add up to total 39,876 due to missing data
†P value is from a chi-squared test
‡Odds ratios adjusted for all variables by logistic regression; 34,658 women with complete demographic information were included in the multivariable model
Several cardiovascular risk factors were associated with lower cholesterol awareness. Women who were current smokers, obese, heavier drinkers, or living sedentary lifestyles were less likely to report their cholesterol levels. In contrast, 89% of women receiving treatment for hypertension and 99% of women receiving lipid-lowering agents reported their cholesterol levels (each P < .0001). Women with untreated hypertension had significantly less knowledge of their cholesterol levels than did those with treated hypertension (P < .0001, not shown in table). Women with diabetes were not more likely than women without diabetes to know their cholesterol levels (P = .41). Interestingly, women receiving HRT were much more likely than women who never received HRT to report their cholesterol level (OR = 1.7). Women who provided blood samples had a 44% increased odds of cholesterol awareness. We reran the multivariate analysis after exclusion of the 74 women who left blank the question on cholesterol level, and found virtually identical results.
The area under the ROC curve22 was 0.66, indicating that the multivariable model has a marginal ability to discriminate those with and without awareness of cholesterol levels.
Accuracy of Self-reported Cholesterol
Among women who provided both a cholesterol level and a blood sample, self-reported and measured blood cholesterol were moderately correlated. The Pearson and Spearman correlation coefficients were 0.54 and 0.57, respectively (P < .0001), for TC (Fig. 1) and 0.63 and 0.65, respectively (P < .0001), for HDL.
Figure 1.
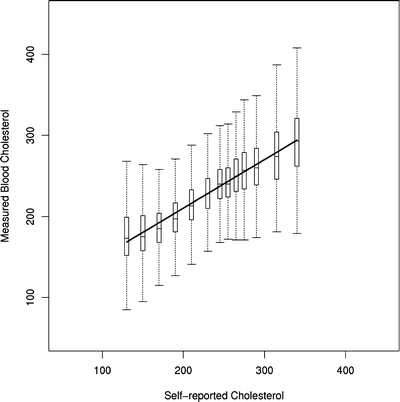
Distribution of measured cholesterol levels within categories of self-reported total cholesterol levels. For each of the 13 categories of self-reported cholesterol, the figure shows the interquartile range of measured total cholesterol (box), the median (horizontal line within the box), and the extreme values within 1.5 times the interquartile range from the upper or lower quartile (vertical bars above and below the box).
In general, women underestimated their TC level by an average of 9.7 mg/dL (95% CI: 9.2–10.2). Almost half of the participants (49.8%) had a difference of <20 mg/dL in either direction between self-reported and measured cholesterol, with 32.6% of women underestimating by >20 mg/dL. For HDL, 52.7% participants had a difference of <10 mg/dL in either direction between self-reported and measured HDL, with 37.8% overestimating by >10 mg/dL. Women systematically overestimated their HDL by 12.4 mg/dL (95% CI: 11.7–13.2).
The magnitude of the bias was significantly higher among divorced women and current smokers and less among obese (BMI > 30) and hypertensive women and women receiving treatment for hypercholesterolemia (Table 2). Overall, the bias could not be explained well by the available variables, as the R2 for the multivariable regression model was 0.008.
Table 2.
Mean Difference Between Self-reported and Measured Total Cholesterol, by Baseline Characteristics
| Baseline characteristics | N* | Mean cholesterol (mg/mL) | Difference | 95% CI | Regression coefficient† | P value | |
|---|---|---|---|---|---|---|---|
| Self-reported | Measured | ||||||
| Total | 24,069 | 202.1 | 211.8 | −9.7 | (−10.2, −9.2) | ||
| Age (yr) | |||||||
| <50 | 7,534 | 191.3 | 201.2 | −9.9 | (−10.7, −9.1) | Referent | |
| 50–59 | 11,183 | 204.0 | 214.0 | −9.9 | (−10.6, −9.2) | −0.35 | 0.59 |
| 60–69 | 4,539 | 213.4 | 222.1 | −8.7 | (−9.9, −7.5) | 0.42 | 0.63 |
| 70–79 | 780 | 212.6 | 222.6 | −10.0 | (−12.8, −7.1) | −0.37 | 0.83 |
| >80 | 33 | 210.6 | 218.7 | −8.1 | (−22.2, 6.0) | 2.33 | 0.75 |
| P‡ = 0.45 | |||||||
| Race | |||||||
| White | 22,729 | 202.2 | 211.9 | −9.7 | (−10.2, −9.2) | Referent | |
| Hispanic | 246 | 202.9 | 210.7 | −7.8 | (−12.9, −2.8) | 2.55 | 0.33 |
| African American | 441 | 198.3 | 209.8 | −11.6 | (−15.4, −7.7) | −1.37 | 0.47 |
| Asian American | 344 | 199.5 | 209.4 | −9.8 | (−13.8, −5.9) | 0.07 | 0.97 |
| American Indian/others | 101 | 203.7 | 211.7 | −7.9 | (−17.8, 1.9) | 1.69 | 0.68 |
| P‡ = 0.76 | |||||||
| Education | |||||||
| LPN/LVN | 2,805 | 204.3 | 215.4 | −11.1 | (−12.6, −9.6) | Referent | |
| 2-y Associate’s degree RN | 2,597 | 200.1 | 211.6 | −11.5 | (−13.1, −9.9) | −0.46 | 0.70 |
| 3-y RN diploma | 7,697 | 205.4 | 214.4 | −8.9 | (−9.8, −8.1) | 1.84 | 0.05 |
| BS | 5,630 | 200.0 | 209.2 | −9.2 | (−10.2, −8.2) | 1.71 | 0.08 |
| MS | 3,660 | 198.8 | 208.8 | −10.1 | (−11.3, −8.9) | 1.02 | 0.36 |
| Doctorate/MD | 1,291 | 199.6 | 208.2 | −8.6 | (−10.5, −6.8) | 3.38 | 0.02 |
| P‡ = 0.01 | |||||||
| Income | |||||||
| <$10,000 | 139 | 206.2 | 217.9 | −11.7 | (−19.1, −4.2) | Referent | |
| $10,000–19,999 | 931 | 210.2 | 222.4 | −12.3 | (−15.0, −9.5) | −3.05 | 0.40 |
| $20,000–29,999 | 2,159 | 208.1 | 218.0 | −9.9 | (−11.6, −8.2) | −0.73 | 0.83 |
| $30,000–39,999 | 3,127 | 205.4 | 214.1 | −8.7 | (−10.1, −7.3) | 0.38 | 0.92 |
| $40,000–49,999 | 3,782 | 202.4 | 212.2 | −9.8 | (−11.0, −8.6) | −1.05 | 0.76 |
| $50,000–99,999 | 9,608 | 199.8 | 209.3 | −9.5 | (−10.2, −8.7) | −1.05 | 0.76 |
| >$100,000 | 3,060 | 196.8 | 207.7 | −10.9 | (−12.2, −9.5) | −2.13 | 0.54 |
| P‡ = 0.14 | |||||||
| Marital status | |||||||
| Married | 17,500 | 201.8 | 210.8 | −9.1 | (−9.6, −8.5) | Referent | |
| Single | 1,309 | 204.4 | 212.3 | −8.0 | (−10.0, −5.9) | 0.83 | 0.49 |
| Divorced | 3,086 | 200.4 | 212.7 | −12.3 | (−13.7, −10.9) | −3.34 | <0.001 |
| Widowed | 1,457 | 208.6 | 219.7 | −11.1 | (−13.3, −8.9) | −2.33 | 0.05 |
| P‡ < 0.001 | |||||||
| Baseline history of diabetes | |||||||
| No | 23,470 | 201.9 | 211.6 | −9.7 | (−10.2, −9.2) | Referent | |
| Yes | 586 | 207.6 | 217.8 | −10.2 | (−13.6, −6.8) | −3.17 | 0.07 |
| P‡ = .74 | |||||||
| Smoking status | |||||||
| Never | 12,573 | 201.4 | 210.5 | −9.1 | (−9.8, −8.5) | Referent | |
| Current | 2,535 | 204.2 | 217.0 | −12.8 | (−14.4, −11.2) | −3.10 | 0.001 |
| Past | 8,940 | 202.5 | 212.1 | −9.6 | (−10.4, −8.8) | −0.36 | 0.53 |
| P‡ < .001 | |||||||
| Hypertension | |||||||
| Normotensive | 17,899 | 199.2 | 209.6 | −10.4 | (−11.0, −9.9) | Referent | |
| Untreated | 2,777 | 210.2 | 217.9 | −7.6 | (−9.1, −6.2) | 2.27 | 0.01 |
| Treated | 3,372 | 210.5 | 218.0 | −7.5 | (−8.8, −6.1) | 1.87 | 0.02 |
| P‡ < .001 | |||||||
| Lipid-lowering agents | |||||||
| No | 23,168 | 201.0 | 211.0 | −10.0 | (−10.5, −9.5) | Referent | |
| Yes | 883 | 231.1 | 232.2 | −1.1 | (−3.9, 1.7) | 9.22 | <0.001 |
| P‡ < .001 | |||||||
| BMI | |||||||
| <25 | 12,254 | 197.6 | 208.1 | −10.5 | (−11.1, −9.8) | Referent | |
| 25–30 | 7,273 | 206.3 | 216.5 | −10.2 | (−11.1, −9.3) | −0.20 | 0.74 |
| ≥30 | 4,074 | 207.5 | 213.8 | −6.3 | (−7.5, −5.1) | 3.70 | <0.001 |
| P‡ < .001 | |||||||
| Alcohol | |||||||
| Never/rarely | 10,505 | 203.0 | 212.4 | −9.4 | (−10.1, −8.6) | Referent | |
| <2 drinks/day | 12,645 | 201.0 | 211.0 | −9.9 | (−10.6, −9.3) | 0.41 | 0.47 |
| ≥2 drinks/day | 913 | 205.7 | 215.4 | −9.7 | (−12.3, −7.2) | −0.12 | 0.93 |
| P‡ = .58 | |||||||
| Exercise | |||||||
| Never/rarely | 8,706 | 205.4 | 214.0 | −8.6 | (−9.4, −7.8) | Referent | |
| <1 time/week | 4,653 | 201.6 | 211.2 | −9.6 | (−10.7, −8.5) | −0.73 | 0.33 |
| 1–3 times/week | 7,847 | 200.2 | 210.8 | −10.6 | (−11.4, −9.7) | −1.36 | 0.03 |
| ≥4 times/week | 2,855 | 198.0 | 208.7 | −10.7 | (−12.1, −9.2) | −1.79 | 0.05 |
| P‡ = .006 | |||||||
| HRT | |||||||
| Never | 10,744 | 197.8 | 207.6 | −9.8 | (−10.5, −9.1) | Referent | |
| Past | 2,407 | 208.9 | 218.6 | −9.7 | (−11.3, −8.0) | −0.38 | 0.69 |
| Current | 10,870 | 204.9 | 214.5 | −9.6 | (−10.3, −8.9) | −0.05 | 0.93 |
| P‡ = .94 | |||||||
*Number of women in each category may not add up to total 24,069 due to missing data,
†Difference adjusted for all variables in linear regression with overall R2 = .008
‡Overall P value for difference between mean self-reported and blood cholesterol for each characteristic
Estimates of the prevalence of hypercholesterolemia by self-report were lower than those by objective blood measurement. Prevalence of hypercholesterolemia (>200 mg/dl) was estimated to be 52.9% by self-report and 59.5% by measured cholesterol. With >240 mg/dL used as the cutoff point, the estimated prevalence was 14.2% by self-report and 22.0% by blood test.
Predictive Value of Self-reported Cholesterol
Baseline levels of self-reported and measured blood cholesterol each predicted the risk of incident cardiovascular outcomes in women (Table 3). A difference of 40 mg/dL in self-reported cholesterol at baseline was significantly associated with a 23% increase in the hazard of incident cardiovascular event (95% CI: 15%–33%).
Table 3.
Relative Hazard of Cardiovascular Disease for Measured and Self-reported Cholesterol
| Models | Hazard ratio* | P value | Likelihood ratio statistic |
|---|---|---|---|
| Univariate models with level of cholesterol† | |||
| Measured | 1.18 (1.10–1.25) | <0.001 | 393.71 |
| Self-reported | 1.23 (1.15–1.33) | <0.001 | 400.86 |
| Average of measured and self-reported | 1.28 (1.18–1.38) | <0.001 | 405.56 |
| Two-covariate model with level of cholesterol‡ | |||
| Self-reported | 1.17 (1.07–1.27) | <0.001 | 406.32 |
| Measured | 1.10 (1.02–1.18) | 0.02 | |
| Categorical model of knowledge and measured cholesterol§ | |||
| Women with measured cholesterol ≤ 240 and self-reported | 1.00 (referent) | ||
| Women with measured cholesterol ≤ 240 and did not report | 0.94 (0.74–1.20) | 0.62 | |
| Women with measured cholesterol > 240 and self-reported | 1.33 (1.14–1.56) | <0.001 | |
| Women with measured cholesterol > 240 and did not report | 1.88 (1.40–2.51) | <0.001 | |
*Hazard ratio calculated for a 40 mg/dL elevation in cholesterol
†Relationship of individual cholesterol variables with the hazard of first cardiovascular events; proportional hazards model adjusted for age in 24,069 women followed for a median of 10 years, 741 developed CVD
‡Joint relationship of self-reported and measured cholesterol with the hazard of first cardiovascular events
§Proportional hazard model adjusted for age in 27,938 women followed for a median of 10 years, 867 developed CVD
In univariate models, the log likelihood statistic was higher for self-reported cholesterol than for measured blood cholesterol. The two-covariate model was significantly better than univariate models (likelihood-ratio test P < .05). On average, for every 40 mg/dL increase in self-reported cholesterol, the hazard of CVD increased 17% (95% CI: 7%–27%), and for every 40 mg/dL increase in measured cholesterol, the hazard of CVD increased 10% (95% CI: 2%–18%) after controlling for age. With adjustment for additional traditional CVD risk factors (included control for cholesterol-lowering agents and HRT), no apparent confounding was noted. Upon exclusion of women using cholesterol-lowering drugs, both self-reported and measured cholesterol remained jointly and significantly related to risk of CVD. The hypothesis of a linear relationship between cholesterol and the log-hazard of CVD was not rejected for either measured or self-reported cholesterol.
Joint consideration of the relationship of elevated measured cholesterol (>240 mg/dL) and knowledge of cholesterol found a significant interaction between these two variables (P = .04). Among women with measured cholesterol ≤240 mg/dL, those who reported their cholesterol level had similar CVD risk to those who did not report, whereas women with elevated cholesterol who did not report their level had markedly increased risk (HR = 1.88, P < .0001).
DISCUSSION
Awareness of cholesterol is a cornerstone to the prevention of CVD, yet our results show that women with one or more important risk factor tend to have less accurate knowledge of their cholesterol level than do women without such risk factors. Even health professionals underestimate their cholesterol levels and have only moderate knowledge of whether their cholesterol is elevated. In particular, cigarette smoking, lack of exercise, and obesity are all independently associated with decreased awareness of cholesterol levels. Despite their much greater risk of cardiovascular disease, women with untreated hypertension also have less awareness of cholesterol than those with treated hypertension, and women with diabetes are no more knowledgeable of their cholesterol levels than those without diabetes. Lower income and education also correlated with decreased cholesterol awareness, yet the significant associations of other risk factors with decreased awareness did not change after controlling for these variables.
Population-based surveys have demonstrated that awareness of cholesterol level is becoming more prevalent in the general population. In a recent survey, 71% of US adults reported that they had a cholesterol screening within the previous 5 years,9 and in a separate study, 49% of US adults surveyed in 2001 reported that they knew their total cholesterol.7 In 2000, Harawa et al.23 found that 23% of those ≥55 reported HDL, and in a 2003 American Heart Association National Study, Mosca et al.11 found that 29% of women reported knowing their HDL level. In comparison to our data obtained 10 years ago, the evidence from recent studies indicated only a slight increase with time in levels of cholesterol awareness.
While overall cholesterol awareness was higher among participants in the WHS, the factors affecting awareness were generally consistent with findings from previous studies. Two previous studies4,6 found poorer cholesterol knowledge among current smokers and sedentary people. Lower income and educational levels were also associated with decreased cholesterol awareness across studies.4,6,23,24 Some studies4,8,24 also reported lower cholesterol screening and lower knowledge among blacks than among whites, but our results suggest that racial differences may not be present among people with similar occupations. Previous studies had equivocal results about the relationships of diabetes, BMI, and alcohol consumption with cholesterol awareness. Although one report4,10 suggested better knowledge of cholesterol levels among those with diabetes and obesity, other reports failed to demonstrate this association.6,24 Thus, the differences in our results might be because of comparable educational levels in our population and greater knowledge of risk factors than in the general population. Our finding of greater awareness of cholesterol among users of HRT is consistent with other evidence of better health care knowledge among users of HRT during the study period.25
Previous studies with smaller samples12–18 have examined factors related to the validity of self-reported total cholesterol. In a study of 192 adults, Bowlin et al.12 found that women underreported their cholesterol by an average of 1 mg/dL, and men underreported it by an average of 3 mg/dL. In addition to problems with recall, differences between reported and measured cholesterol might also be because of the natural seasonal and diurnal variability of cholesterol or to assay variability across laboratories. Our main finding on validity is that personal characteristics had little ability to explain the discrepancies between reported and measured cholesterol (R2 < .01); observed differences were equivalently substantial across all major subgroups of our population.
Limitations of self-reported cholesterol include errors in recall of measured values and changes in lifestyle that may affect cholesterol. Indeed, changes in diet or initiation of medications affecting cholesterol such as hormone therapy since last assessment of cholesterol would increase differences between measured and self-reported cholesterol levels. Initiation of lipid-lowering therapy would also influence cholesterol levels, although women would presumably have their cholesterol checked after beginning such treatment. We asked women to report their cholesterol level if checked within the past 5 years. A narrower window would probably have decreased the average difference between self-reported and measured cholesterol, although it would also likely have introduced potential selection bias because of a greater number of missing values. Indeed, Adult Treatment Panel III1 recommends screening of lipid profiles every 5 years in low risk persons, so a narrower window would be expected to selectively eliminate such people. Despite the clear limitations of self-reported cholesterol, it was a strong predictor of subsequent cardiovascular events. Self-reported cholesterol may represent a person’s integration of several recent cholesterol measurements, and to health professionals, may be useful for risk stratification. Furthermore, our results suggest that women with elevated cholesterol who do not know their level may be at a particularly increased risk of CVD, further emphasizing the value of cholesterol knowledge.
Other limitations of our study include the restricted range of occupations and the inclusion of women willing to participate in this trial. This limits the generalizability of overall rates, and the observed 84% of women who reported their TC levels is surely higher than that of the general population. Nonetheless, use of this population can enhance the validity of relationships between risk factors and cholesterol knowledge because of the more reliable reporting of other risk factors. This study also addresses the role of cholesterol knowledge when controlled for socioeconomic status. Furthermore, the observed 10 mg/dL difference between self-reported and measured cholesterol likely provides lower bounds on these discrepancies in the general population. In addition to the above limitation, our data on HDL were collected at 48-month follow-up; validity of this self-report might have improved with contemporaneous blood samples. Also, LDL awareness was not assessed in this study because TC was still being recommended by contemporary NCEP II guidelines as an initial screen for hypercholesterolemia and an overall marker of cholesterol status in patients on cholesterol therapy.2
The results suggest that cholesterol education programs should especially target persons with one or more additional cardiovascular risk factors because of their greater risk of CVD and their likely poorer knowledge of their cholesterol level. Although there are clear limitations to the accuracy of cholesterol knowledge, people should know that their lack of awareness of elevated cholesterol is associated with an increased risk of subsequent CVD and take steps to reduce this risk.
Acknowledgement
This study was supported by grants (HL43851, CA47988) from the National Institutes of Health and by philanthropic support from Elizabeth and Alan Doft and their family. The abstract was presented at the 2nd International Conference on Women, Heart Disease and Stroke, February 16–19, 2005 (Circulation 2005;111: e40–e88).
Conflict of Interest Dr. Huang has no potential conflicts of interest. Dr. Buring has received investigator-initiated research funding and support from Dow Corning Corporation, research support for pills and/or packaging on NIH-funded studies from Bayer Health Care and the Natural Source Vitamin E Association, honoraria from Bayer for speaking engagements, and she serves on an external scientific advisory committee for a study by Procter & Gamble. Dr. Ridker has received investigator-initiated research support from Astra-Zeneca, Bayer, Bristol-Myers Squibb, Dade-Behring, Novartis, Pharmacia, Roche, Sanofi-Aventis, and Variagenics. Dr. Ridker is listed as a coinventor on patents held by the Brigham and Women’s Hospital that relate to the use of inflammatory biomarkers in cardiovascular disease and has served as a consultant to Schering-Plough, Sanofi-Aventis, Astra Zeneca, Isis Pharmaceutical, and Dade-Behring. Dr. Glynn has received investigator-initiated research support from Astra-Zeneca, Bristol-Myers Squibb, and Novartis.
References
- 1.Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97. [DOI] [PubMed]
- 2.National Cholesterol Education Program. Second Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). Circulation. 1994;89:1333–445. [DOI] [PubMed]
- 3.U.S. Department of Health and Human Services. Healthy People 2010. 2nd ed. With Understanding and Improving Health and Objectives for Improving Health. 2 vols. Washington, DC: U.S. Government Printing Office; 2000.
- 4.Centers for Disease Control and Prevention. Progress in chronic disease prevention factors related to cholesterol screening and cholesterol level awareness—United States, 1989. MMWR Morb Mortal Wkly Rep. 1990;39:633–7. [PubMed]
- 5.Schucker B, Wittes J, Santanello N, et al. Change in cholesterol awareness and action: results from national physician and public surveys. Arch Intern Med. 1991;151:666–73. [DOI] [PubMed]
- 6.Pieper RM, Arnett DK, McGovern PG, Shahar E, Blackburn H, Luepker RV. Trend in cholesterol knowledge and screening and hypercholesterolemia awareness and treatment, 1980–1992: the Minnesota Heart Survey. Arch Intern Med. 1997;157:2326–32. [DOI] [PubMed]
- 7.Nash IS, Mosca L, Blumenthal RS, Davidson MH, Smith SC, Pasternak RC. Contemporary awareness and understanding of cholesterol as a risk factor. Arch Intern Med. 2003;163:1597–1600. [DOI] [PubMed]
- 8.Nieto FJ, Alonso J, Chambless L, et al. Population awareness and control of hypertension and hypercholesterolemia. The Atherosclerosis Risk in Communities study. Arch Intern Med. 1995;155:677–84. [DOI] [PubMed]
- 9.Centers for Disease Control and Prevention. State-specific cholesterol screening trends—United States, 1991–1999. MMWR Morb Mortal Wkly Rep. 2000;49:750–5. [PubMed]
- 10.Centers for Disease Control and Prevention. Cholesterol screening and awareness—Behavioral Risk Factor Surveillance System, 1990. MMWR Morb Mortal Wkly Rep. 1992;41(36). [PubMed]
- 11.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease—an American Heart Association National Study. Circulation 2004;109:573–9 [DOI] [PubMed]
- 12.Bowlin SJ, Morrill BD, Nafziger AN, Jenkins PL, Lewis C, Pearson TA. Validity of cardiovascular disease risk factors assess by telephone survey: the Behavioral Risk Factor Study. J Clin Epidemiol. 1993;46:561–71. [DOI] [PubMed]
- 13.Bowlin S, Morrill B, Nafziger A, Lewis C, Pearson T. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: The Behavioral Risk Factor Survey. J Clin Epidemiol. 1996;49:511–7. [DOI] [PubMed]
- 14.Natarajan S, Lipsitz SR, Nietert PJ. Self-report of high cholesterol-determinants of validity in U.S. adults. Am J Prev Med. 2002;23:13–21. [DOI] [PubMed]
- 15.Colditz GA, Martin P, Stampfer MJ, et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol. 1986;123:894–900. [DOI] [PubMed]
- 16.Newell S, Girgis A, Sanson-Fisher R, Ireland M. Accuracy of patients’ recall of Pap and cholesterol screening. Am J Public Health. 2000;90:1431–5. [DOI] [PMC free article] [PubMed]
- 17.Murdoch M, Wilt TJ. Cholesterol awareness after case-finding: do patients really know their cholesterol numbers? Am J Prev Med. 1997;13:284–9. [PubMed]
- 18.Bairey Merz CN, Felando MN, Klein J. Cholesterol awareness and treatment in patients with coronary artery disease participating in cardiac rehabilitation. J Cardiopulm Rehabil. 1996;16:117–22. [DOI] [PubMed]
- 19.Rexrode KM, Lee I, Cook NR, Hennekens CH, Buring JE. Baseline characteristics of participants in the Women’s Health Study. J Womens Health Gend Based Med. 2000;9:19–27. [DOI] [PubMed]
- 20.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–304. [DOI] [PubMed]
- 21.Lee IM, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer. The Women’s Health Study: a randomized controlled trial. JAMA 2005;294:47–55. [DOI] [PubMed]
- 22.Hosmer DW, Lemeshow S. Applied Logistic Regression, 2nd edition. New York: John Wiley and Sons; 2000.
- 23.Harawa NT, Morgenstern H, Beck J, Moore A. Correlates of knowledge of one’s blood pressure and cholesterol levels among older members of a managed care plan. Aging. 2001;13:95–104. [DOI] [PubMed]
- 24.Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity—data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162:929–35 [DOI] [PubMed]
- 25.Brennan RM, Crespo CJ, Wactawski-Wende J. Health behaviors and other characteristics of women on hormone therapy: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Menopause 2004;11:536–42. [DOI] [PubMed]


