Abstract
Objective:
To determine whether the routine use of surgical exploration for gastrinoma resection/cure in 160 patients with Zollinger-Ellison syndrome (ZES) altered survival compared with 35 ZES patients who did not undergo surgery.
Summary Background Data:
The role of routine surgical exploration for resection/cure in patients with ZES has been controversial since the original description of this disease in 1955. This controversy continues today, not only because medical therapy for acid hypersecretion is so effective, but also in large part because no studies have shown an effect of tumor resection on survival.
Methods:
Long-term follow-up of 160 ZES patients who underwent routine surgery for gastrinoma/resection/cure was compared with 35 patients who had similar disease but did not undergo surgery for a variety of reasons. All patients had preoperative CT, MRI, ultrasound; if unclear, angiography and somatostatin receptor scintigraphy since 1994 to determine resectability. At surgery, all had the same standard ZES operation. All patients were evaluated yearly with imaging studies and disease activity studies.
Results:
The 35 nonsurgical patients did not differ from the 160 operated in clinical, laboratory, or tumor imaging results. The 2 groups did not differ in follow-up time since initial evaluation (range, 11.8–12 years). At surgery, 94% had a tumor removed, 51% were cured immediately, and 41% at last follow-up. Significantly more unoperated patients developed liver metastases (29% vs. 5%, P = 0.0002), died of any cause (54 vs. 21%, P = 0.0002), or died a disease-related death (23 vs. 1%, P < 0.00001). Survival plots showed operated patients had a better disease-related survival (P = 0.0012); however, there was no difference in non-disease-related survival. Fifteen-year disease-related survival was 98% for operated and 74% for unoperated (P = 0.0002).
Conclusions:
These results demonstrate that routine surgical exploration increases survival in patients with ZES by increasing disease-related survival and decreasing the development of advanced disease. Routine surgical exploration should be performed in ZES patients.
The routine need for surgical exploration for possible cure in patients with Zollinger-Ellison syndrome (ZES) remains controversial. In 195 patients with ZES, of whom 160 underwent surgery and 35 did not, we show that surgery increases survival and disease-related survival and, thus, should be routinely performed.
The role of routine surgical exploration for gastrinoma resection has remained controversial since almost the initial description of this syndrome in 1955 by Zollinger and Ellison.1 Initially, the controversy was between whether to only perform a total gastrectomy or whether attempted tumor resection was an alternative either alone or combined with a total gastrectomy or a lesser acid-reducing procedure.2–4 With the development of effective gastric antisecretory drugs first with histamine H2 antagonists in the 1970s and 1980s and later proton pump inhibitors (PPIs) the nature of the debate has changed; however, the controversy has only increased.5–9 The nature of the debate changed to whether medical treatment alone should be carried out or whether surgery for gastrinoma resection should be considered in patients with potentially resectable disease for all such patients or a subset.5–8 The controversy not only continued but increased because medical therapy is highly effective,7,9,10 in many patients over the short-term the tumor pursues a benign course,7,11 and until recently the long-term natural history of gastrinomas or the ability to cure these patients was largely unclear.12 Even though recently the natural history has been better defined, and it clearly established that an increasing proportion of these patients are dying from the malignant nature of the gastrinoma,13,14 as well as that up to 40% of patients can be cured long-term,8,12,15–17 the place of routine surgical resection for possible cure still remains controversial.7,18 This has occurred in large part because no study has demonstrated that routine surgical exploration with gastrinoma resection leads to increased survival. A previous study by us in 199419 showed that routine surgery decreased the rate of development of liver metastases, the most important prognostic factor for survival in most studies;13,14 however, the follow-up duration and number of patients were not sufficient to show an effect on survival. We now report our experience with a larger group of patients (n = 160) who were followed for a mean of 12 years after surgery. These patients' survival is compared with a nonsurgical group (n = 35) who had potentially resectable disease but did not undergo surgery for a variety of reasons; however, they did not differ from the surgical group in clinical, laboratory features or imaging results in initial evaluations.
METHODS
Since 1980 at the National Institutes of Health, 1997 at the University of California San Francisco and 2004 at Stanford University hospitals, all 195 patients with ZES who were involved in our prospective studies of surgical exploration for cure as described previously8,15,17,19–21 were included in this analysis. All patients after confirming the diagnosis and detailed imaging studies were invited to participate in our surgical studies if they had no comorbid medical condition markedly limiting life expectancy, did not have unresectable metastatic disease or if MEN1 was present, had tumor ≥2.5 cm in diameter.8,16,19,22,23
The diagnosis of ZES was based on acid secretory studies, measurement of fasting serum level of gastrin as well as the results of secretin and calcium provocative tests.24–26 Basal and maximal acid output (BAO, MAO) was determined for each patient using methods described previously.25 Doses of oral gastric antisecretory drug were determined as described previously.9,27,28
A detailed past history of disease was taken at first admission including symptoms related to ZES and past medical/surgical procedures as described previously.26,29 Time from onset of the disease to exploration was determined for all patients.14,24 The time of diagnosis of ZES was the time the diagnosis was first established by appropriate laboratory studies or when a physician established the diagnosis based on clinical presentation.8,26
The localization and the extent of the gastrinoma were evaluated in all patients as described elsewhere15,21,30–32 by using upper gastrointestinal endoscopy and conventional imaging studies (CT scan, MRI, transabdominal ultrasound, selective abdominal angiography, and bone scanning). Prior to surgery, functional localization of the gastrinoma measuring gastrin gradients, was performed with the use of portal venous sampling (from January 1980 to April 1992) or hepatic venous sampling after the selective intra-arterial injection of secretin (January 1988 to present).33–35 Somatostatin receptor scintigraphy was performed since 1994 using [111In-DTPA-DPhe1]-octreotide (6 mCi) with whole body, planar, and SPECT views.31,32
All patients referred with a diagnosis of possible ZES underwent an evaluation to establish the diagnosis of ZES and to determine whether MEN1 was present8,22,24,26,29,36 and studies to determine the suitability of surgical exploration for cure.8,22,24,26 These latter studies included tumor localization studies, studies to determine the presence or absence of MEN122,36 and studies to determine the presence of other disease that might make surgery contraindicated. MEN1 was established by assessing plasma hormone levels (PTH [intact, midmolecule], prolactin, insulin, proinsulin, glucagon), serum calcium (ionized, total) and glucose as well as from personal and family history.22,29,36,37
All patients who fit the protocol for surgical exploration, could give informed consent, and agreed to follow the surgical protocol underwent a surgical exploration for possible cure (n = 160). The short-term follow-up (mean, 7 years) on 98 of these patients was reported previously.19 Before 1987, an extensive search for gastrinoma was performed using palpation, intraoperative ultrasonography,21,38 and an extended Kocher maneuver.17,20 In 1987, additional procedures were added for localizing duodenal gastrinomas.16,17,21,39 These included endoscopic transillumination of the duodenum at surgery39 and the use of a duodenotomy.16,17,21 At exploration, an extensive search for endocrine tumors was performed.8,17,19,31 Briefly, palpation was performed first, followed by intraoperative ultrasound with a 10-MHz real-time transducer8,21,38 after the extended Kocher maneuver. Then, since 1987, the endoscopic transillumination of the duodenum was performed39 and since 1987, finally a 3-cm longitudinal duodenotomy was centered on the anterolateral surface of the descending (second) duodenum to search for duodenal tumors.8,16,21
Tumors in the pancreatic head were enucleated. Tumors in the pancreatic body and tail were enucleated if possible; otherwise, they were resected. Distal pancreatectomy was not routinely performed and was done only if multiple pancreatic body and/or tail tumors were present that could not be enucleated.8,12,22 If multiple pancreatic head tumors were present that could not be enucleated, a pancreaticoduodenectomy was performed if the patient had given prior consent. A detailed inspection for peripancreatic, periduodenal, or portohepatic lymph nodes was carried out, and these were routinely removed.15,40 A gastrinoma in a lymph node(s) was termed a primary lymph node tumor if the patient was disease-free after resection of a gastrinoma only in a lymph node.15,40 If liver metastases were present and localized, they were wedge-resected with a 1-cm margin, if possible; if this was not possible and they were localized, a segmental resection or lobectomy was performed.41,42
Postoperatively, patients underwent evaluation for disease-free status immediately after surgery (ie, 2 weeks postresection), within 3 to 6 months postresection, and then yearly.8,17,24,31 Yearly evaluations included conventional imaging studies (CT, ultrasound, MRI, and angiography, if necessary); somatostatin receptor scintigraphy (SRS) since 1994; assessment of disease status (acid secretory studies, fasting gastrin determinations, secretin provocative test); and assessment of endocrine status (parathyroid, pituitary, adrenal function).8,17,24,31 Disease-free was defined as a normal fasting gastrin level, negative secretin test, and no tumor on imaging studies.8,17,24,31 A recurrence postresection was defined as occurring in a patient who was initially disease-free postresection of a gastrinoma but then lost disease-free status on follow-up evaluation by developing an elevated fasting gastrin level (in the presence of pH <3), an abnormal secretin test or positive imaging studies.24,43
Thirty-five patients with ZES who fit the surgical protocol did not undergo surgical exploration either because they could not give informed consent (n = 1), refused surgery after consulting with their family doctor (n = 19), had comorbid conditions increasing surgical risk (n = 5) or had MEN1 with no lesions found on imaging ≥2.5 cm in diameter (n = 10). The short-term follow-up on a subset (n = 29) of these patients was reported previously.19 These patients had the same evaluation and imaging studies outlined above for the surgical patients including angiography,44 but less frequently underwent functional localization studies (ie, portal venous sampling, secretin stimulation with gastrin gradients) to better define tumor location preoperatively, when it became clear that no surgery was to be done. These patients were treated long-term with gastric antisecretory drugs (either H2-blockers or since 1985 PPIs) as described previously.9,27,28,45 They were evaluated every 6 to 12 months with serial imaging studies including conventional imaging studies (ultrasound, CT, MRI) and since 1994 SRS. If results were equivocal and a possible new lesion was seen, selective angiography was also repeated.44
The Fisher exact test and the Mann-Whitney U test were used for 2-group comparisons. All continuous variables were reported as mean ± standard error of the mean. The probabilities of survival were calculated and plotted according to the Kaplan-Meier method and compared using the exact log-rank test46 and the method of Rothman47 to determine the confidence intervals. For the determination of the times to death due to ZES the method of Aalen48 was used to estimate the probabilities and bootstrapping for the confidence intervals. For comparisons of the times to death due to ZES the method of Lunn and McNeil was used.49
RESULTS
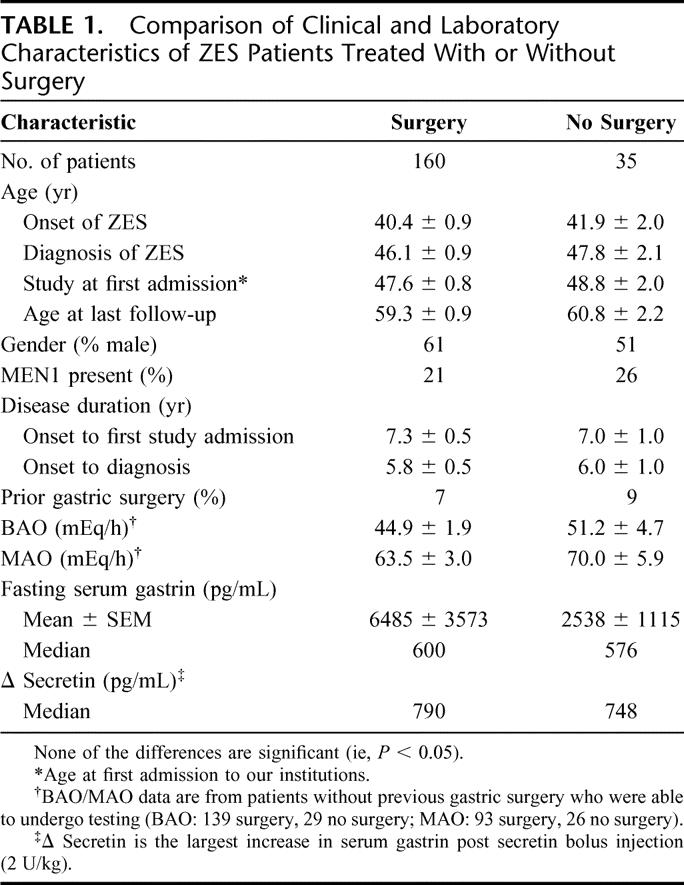
During the period of the study 160 patients with ZES underwent initial surgical exploration to attempt to resect the gastrinoma, whereas 35 patients who had similar disease extent did not undergo surgical exploration. The clinical and laboratory characteristics of these 2 groups of patients are shown in Table 1. The 2 groups did not differ in age whether measured at time of onset of ZES, at diagnosis of ZES, at the time of their first admission for evaluation at our institutions or at the age of last follow-up. They also did not differ in gender, percentage with MEN1 present, disease duration, occurrence of prior gastric acid-reducing surgery, acid secretory rates (BAO, MAO), fasting gastrin level, or fasting gastrin increase with secretin (Δ Secretin) (Table 1).
TABLE 1. Comparison of Clinical and Laboratory Characteristics of ZES Patients Treated With or Without Surgery
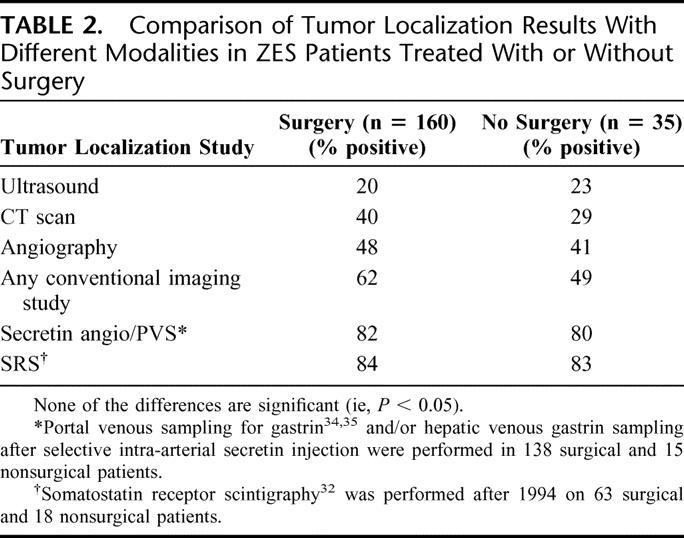
During the initial admissions to our institutions all patients underwent detailed imaging to evaluate tumor location and extent. For each of the imaging modalities, there were no significant differences in the percentage of patients in whom a tumor was localized in the surgical and nonsurgical groups (Table 2). Specifically, ultrasound was the least sensitive modality. It localized a tumor in 20% to 23%; CT scan localized a tumor in 40% of the surgical and 29% of the nonsurgical group, a difference that was not significant (P = 0.25). Angiography localized a tumor in 41% to 48% of patients and any conventional imaging study was positive in 62% of surgical and 49% of nonsurgical patients (P = 0.18). Functional localization measuring gastrin gradients and SRS (performed since 1994) was done on a subset of the patients and was more sensitive than conventional imaging studies being positive in 80% to 82% and 83% to 84%, respectively (Table 2).
TABLE 2. Comparison of Tumor Localization Results With Different Modalities in ZES Patients Treated With or Without Surgery
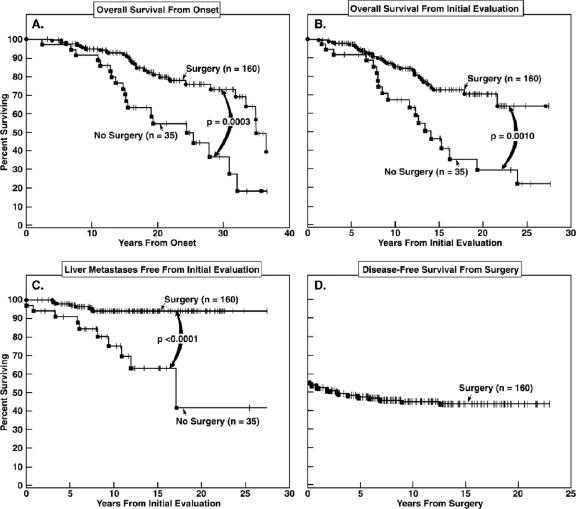
At surgical exploration 150 of 160 patients (94%) had a gastrinoma found and removed. The last 106 patients who underwent surgery each had a gastrinoma found and the 10 patients without a gastrinoma found were all operated prior to the routine use of duodenotomy.16,17,21 The primary tumor location and tumor extent found at surgery are summarized in Table 3. Similar to other recent surgical series duodenal tumors were 3 times more frequent than pancreatic gastrinoma (52% vs. 17%, respectively).8,50,51 Similar to recently reported,8,15,40 lymph node primaries were not infrequent occurring in 12% of patients and primary gastrinomas were found in nonduodenal, nonpancreatic, or a nonlymph node location in 7.5% of patients (bile duct or liver, ovary, heart, pyloric canal, jejunum, and omentum) (Table 3). In 16% of patients the primary site was indeterminate either because no tumor was found or only a lymph node or liver metastasis was found at surgery and the patient was not made disease-free postresection (Table 3). Forty-one percent of the surgical patients had only a primary tumor found, 43% a primary tumor associated with lymph node metastases and 0.6% had a primary with liver metastases (Table 3). In 9% of patients only lymph node metastases were found and in 1 patient only liver metastases (Table 3). Immediately postoperation, 51% were disease-free17,24 with normal secretin tests, normal fasting serum gastrin, and negative imaging (Fig. 1D). During the follow-up period, 23 patients had a relapse and the remaining 59 patients demonstrated a long-term cure. The mean time to relapse was 3.3 ± 0.6 years with a range from 0.32 to 12.8 years.
TABLE 3. Findings Related to Tumor Location and Extent at Surgical Exploration in 160 Patients
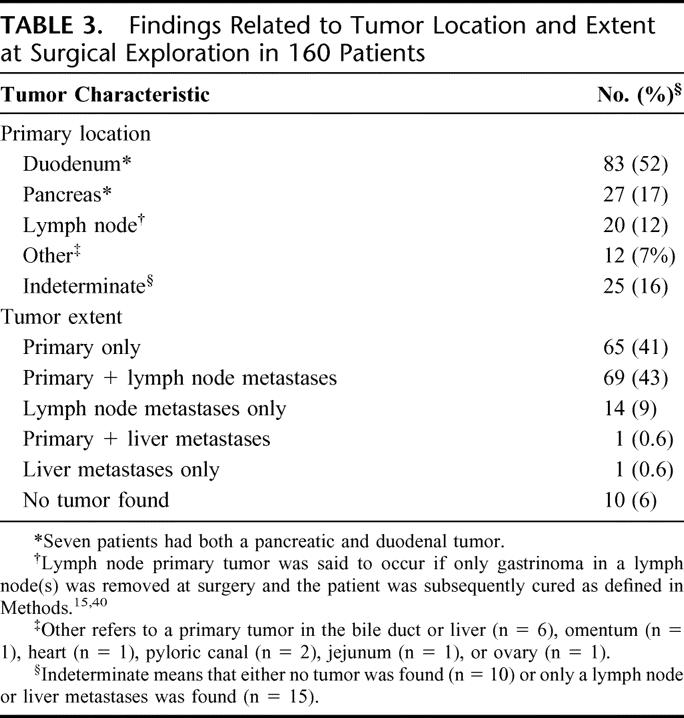
FIGURE 1. Total survival, disease-free survival postresection, and liver metastases-free survival. Total survival from onset of ZES (A) and from the time of the initial ZES evaluation at our institutions (B) is shown for the 160 surgical and 35 nonsurgical patients. Shown in the lower panels is the percent of surgical and nonsurgical patients who remained free of liver metastases with time (C) and the disease-free survival (D) for the surgical group (n = 160) expressed as a percentage of the total surgical group.
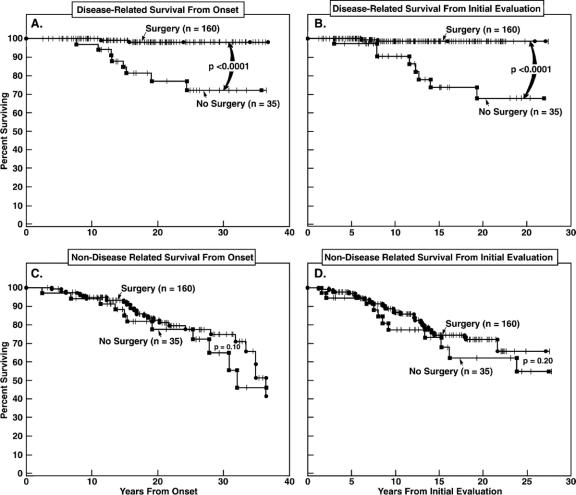
After the initial evaluation with or without surgical exploration patients were all reevaluated for acid control, tumor status, presence of MEN1, and cure status in surgical patients yearly. There was no difference in the mean duration of follow-up in the surgical and nonsurgical patients either from the time of onset of the ZES to the last follow-up (19.2 vs. 19.1 years, respectively) or from the time of the first study admission to the last follow-up (11.8 vs. 12.1 years, respectively) (Table 4; Figs. 1, 2). During this follow-up time, 5 times more patients in the nonsurgical group developed liver metastases than in the surgical group (29% vs. 5%, P = 0.0002) (Table 4; Fig. 1C). The mean time to the development of liver metastases between the 2 groups of patients did not differ (5–7 years) (Table 4). During the follow-up time, twice as many patients also developed new lesions on imaging studies in the nonsurgical compared with the surgical group (37% vs. 16%, P = 0.0092) (Table 4). During the follow-up time, the death rate from any cause was 2.5 times greater in the nonsurgical than the surgical patients (54% vs. 21%, P = 0.0002) (Table 4; Fig. 1A, B). This difference was due to a marked difference in the disease-related death rate, which was 23 times higher in the nonsurgical than the surgical patients (23% vs. 1%, P < 0.00001) (Table 4; Fig. 2A, B). In contrast, there was no difference in the non-disease-related death rates in the nonsurgical and surgical group over this follow-up time (31% vs. 20%, P = 0.18) (Table 4; Fig. 2C, D). These important differences existed whether the data were analyzed from time of onset of ZES (Fig. 2A, C) of from the time of the initial evaluation at our institutions (Fig. 2B, D). The 10 disease-related deaths were due to the tumor per se or tumor progression in 90% of the cases with only 1 patient with nonsurgical treatment dying due to acid-related causes when his acid hypersecretion was inadequately controlled while admitted at an outside hospital for pneumonia resulting in upper gastrointestinal bleeding leading to death.
TABLE 4. Long-term Follow-up of Surgical and Nonsurgically Treated ZES Patients
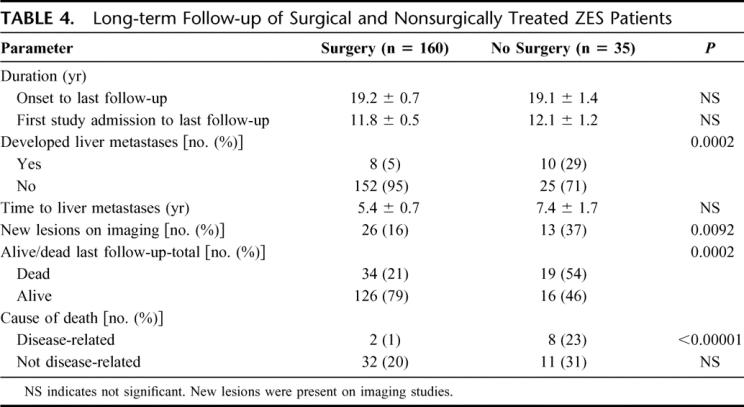
FIGURE 2. Disease-related and non-disease-related survival from onset of ZES (A, C) or first evaluation at our institutions (B, D). Data are plotted in the form of Kaplan-Meier. Shown are the survival results in the 160 surgical patients or 35 patients who did not undergo surgery.
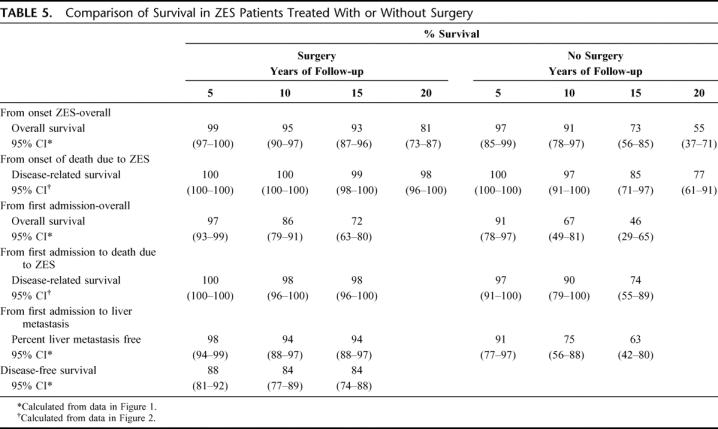
The 5-, 10-, 15-, and 20-year survival rates were calculated for the nonsurgical and surgical patients from both the onset of the ZES as well as from the first admission at our institutions for evaluation (Table 5; Figs. 1, 2). Both the overall survival for the surgical group calculated from the onset (P = 0.0003) of the ZES (20-year survival, 81% vs. 55%) or from the first admission (P = 0.0010) to our institutions (15-year survival, 72% vs. 46%) was highly significantly different (Table 5; Fig. 1). Furthermore, the disease-related survival for the surgical and nonsurgical patients was highly significantly different whether calculated from onset (20-year survival, 98% vs. 77%) or from the first admission (P < 0.0001 for each) at our institutions (15-year survival, 98% vs. 74%) (Table 5; Fig. 2). The percentage of surgical patients who remained free of liver metastases was also significantly greater (P < 0.0001) than the patients who had nonsurgical treatment (15 years, 94% vs. 63%) (Table 5; Fig. 1C).
TABLE 5. Comparison of Survival in ZES Patients Treated With or Without Surgery
DISCUSSION
Gastrinomas, from their first description,1 have presented some unique surgical controversies among all functioning pancreatic endocrine tumors (PETs). In contrast to other functional PETs (insulinomas, VIPomas, glucagonomas, etc.) from the beginning, effective surgical (total gastrectomy)1,52,53 and later, medical (H2 blockers, PPIs)6,9,10 strategies were developed that controlled the effects of the hormone excess in almost every case. This led to the possibility of treating the clinically important effects of the hypergastrinemia (acid hypersecretion) rather than directing treatment against the gastrinoma.1,52,53 Initially, because the gastrinomas were usually small, frequently associated with metastatic lymph nodes, and it was not realized they were primarily in the duodenum rather than the pancreas,3,54 they were missed at surgery or not completely resected and the patient was rarely cured, this approach was warranted, and total gastrectomy became the standard treatment.1,2,52,53 With the development of increasingly effective medical treatments in the late 1970s to 1990s,6,9,10 reports of the slow growth of the gastrinomas in many patients and low cure rates in some studies, the routine use of medical therapy without the routine need for attempted gastrinoma resection and cure was proposed and is, in fact, widely carried out at present.5,7,18 However, it has long been known that 60% to 90% of gastrinomas are malignant54,55 as well as more recent studies showing that a subset pursue an aggressive course11,13,14,56,57 and the natural history of the gastrinoma is becoming the main determinant of long-term survival in these patients.2,56,58 Recent studies show that 30% to 50% of ZES patients with sporadic disease can be cured long-term8,15,16,50 and that the routine surgical exploration can decrease the rate at which patients develop liver metastases.19 Although these results suggest the routine use of surgery in ZES patients should be considered because the presence of liver metastases has been shown to be the most important predictor of survival in most studies,14,56 they alone do not establish that surgery increases survival. The establishment that routine surgery increases the survival of patients with gastrinomas has not been reported because this study is more difficult to perform than with a number of other tumors for a number of reasons. First, gastrinomas are uncommon, occurring in 1 to 3 persons/million/year,59 and approximately 25% to 33% of patients present with hepatic metastases and have unresectable disease.51,59 Second, 20% to 25% of the patients have ZES with MEN129 and the role of surgery is controversial in these patients because they are rarely if ever cured and thus in many centers, they do not under routine exploration for gastrinoma resection.8,22,23,59 Third, because only 25% of gastrinomas demonstrate aggressive growth11,13 and the remaining 75% very indolent growth, long-term studies with a large number of patients are needed to determine an effect on survival. This point is well demonstrated by our previous study,19 which included following 98 surgical patients with ZES and 26 patients without surgery for a mean of 7 years; and even though a decrease in the development of liver metastases could be demonstrated (P < 0.003), the effect on survival did not reach a significant level (P = 0.085). The present study attempted to address the question of survival by including additional patients with ZES who were followed for a longer time period.
In this study with 195 ZES patients (160 surgery, 35 no surgery) followed for a mean of 11.9 years after their initial evaluation with or without surgery and 19.2 years after onset of the ZES, we could demonstrate that routine use of surgery significantly increased survival (P = 0.002).
At the last follow-up, a 2.5 times greater proportion of nonsurgical patients had died than in the surgical group from any cause (54% vs. 21%). Our analysis supported the conclusion that this increase in total survival in the surgery patients was due to the effect of surgery on disease-related survival. This conclusion was supported by our finding that disease-related survival was increased 23-fold at the last follow-up in the nonsurgical group over the surgical group (23% vs. 1%), which was a highly significant difference (P < 0.00001). In contrast, at last follow-up, there was no significant difference in non-disease-related survival in the nonsurgical and surgical groups (31% vs. 20%, P = 0.14). The Kaplan-Meier plots of these data supported each of the above findings and demonstrated that disease-related survival was highly significantly different (P < 0.0001) between the surgical and nonsurgical group with a 15-year disease-related survival of 98% in the surgical group and 74% in the nonsurgical group. A number of our results support the conclusion that surgery extended disease-related survival through its effect on the natural history of the gastrinoma and not on acid hypersecretion due to hypergastrinemia. First, this conclusion was supported by the finding that at last follow-up the nonsurgical group had a 6 times higher rate of liver metastases (29% vs. 5%), which was a highly significant difference (P = 0.0002). Furthermore, on Kaplan-Meier plots, there was a significant difference in the percentage of patients who remained free of liver metastases (P < 0.0001) between surgical and nonsurgical patients with the rates at 15 years being 94% vs. 63%, respectively. Second, at last follow-up, the proportion of nonsurgical patients who had developed new lesions was twice as high as in the surgical group (37% vs. 16%, P = 0.0092). Third, in the 10 patients who had a disease-related death, in only 1 nonsurgical patient was the cause of death likely related to the acid hypersecretion and in the other 9 patients was directly related to the tumor.
Although the differences in the survival results in this study between the surgical and nonsurgical groups are highly significantly different, it is important to remember this study has at least one potential limitation. This study is not a randomized study. At the initial evaluations, all patients were determined to have potentially completely resectable disease and thus to be candidates for surgery. Thus, the extent of tumor was similar in the surgical and nonsurgical groups. However, the 35 patients who did not undergo surgery did so for a variety of reasons, including refusal after discussion with their referring physician (55%), other concurrent illnesses, and inability to give informed consent or due to limitations of the MEN1 surgical protocol. Nevertheless, our analysis shows that the surgical and nonsurgical groups did not differ in any clinical parameter; in the percentage with MEN1; in laboratory results such as the fasting gastrin level or increase in fasting gastrin with secretin or in the results of the initial tumor imaging with either conventional imaging studies (CT, ultrasound), angiography, or in the subsets who had functional localization studies measuring fasting gastrin gradients or somatostatin receptor scintigraphy. Furthermore, there was no difference in the follow-up times whether measured from the onset of ZES or from the time of the initial evaluation at our institutions. Important parameters that have been shown to be predictive for aggressive disease include gender, MEN1 status, disease duration, fasting gastrin level, and tumor imaging results13,14,56,60 were not significantly different in the 2 groups of patients. These results support the conclusion that these 2 study groups were comparable at the start of the study and therefore provide no evidence for any biases.
CONCLUSION
This study for the first time demonstrates that routine surgical exploration for gastrinoma removal/cure in patients with ZES increases patient survival. It does this by increasing disease-related survival without altering non-disease-related survival. The effect of surgery on disease-related survival is due to its effects on the tumor (ie, preventing progression, development of liver metastases, tumor growth) and not the acid secretory rate, as was the case with total gastrectomy in the past. These results show that routine surgical exploration should be performed in all ZES patients with resectable tumor and sporadic ZES and any patient with MEN1/ZES with a tumor >2 to 2.5 cm.
Discussions
Dr. Murray F. Brennan (New York, New York): I am grateful for the invitation to discuss this paper by Dr. Norton and thank him for the timely delivery of the manuscript. It is now 61 years since Dr. Zollinger first presented the subject to this organization.
As a much younger man, I presented a paper on Zollinger-Ellison at this meeting 24 years ago in 1982. The discussants at that time were Drs. Friesen, McClelland, Thompson, and Zollinger. And, Dr. Norton, you can rest assured you cannot possibly have the tachycardia I had that day!
Robert Jensen was the senior author on the paper that I presented, and now he is the senior author on Dr. Norton's paper. Some things at the NIH just never change.
It does, however, reflect the extraordinary commitment by this group, Dr. Norton in particular, and his colleagues Drs. Fraker, Alexander, and Jensen, to the study of patients with these complicated neuroendocrine disorders. It makes a very strong argument, as others have made in the past, that surgeons have an obligation to provide long-term and continuous follow-up to determine the true outcome of management of patients, particularly those with complex neuroendocrine disease. This is a very fine paper. It is a challenging title, which in the absence of a randomized trial is as close as we can come.
Comparative studies inevitably run the risk of association because of favorable selection. The key to prove that surgery (I might actually prefer operation) increases survival is its comparative use to those who are eligible for operation but did not undergo it. In the control group, there were 19 who refused, 5 who had comorbidities, and 10 who had multiple endocrine neoplasia with less than 2.35-cm tumors. The key is the 19 patients who were eligible but refused operation.
In the late 1970s and early 1980s, when this study began, we were at the NIH working on an elective premise that the new drug, cimetidine, would control the disease and avoid total gastrectomy. The first question then, as your study began in 1980, Dr. Norton, were any of the patients who were deliberately maintained on cimetidine included in the control group?
The 19 patients who refused operation are a very small group. And as Dr. Norton emphasizes, in the absence of a randomized trial, only data of this maturity and length can be utilized to make a cause-and-effect association. I actually take solace in the fact that we concluded in 1982 that “aggressive attempts at preoperative localization with laparotomy and tumor resection seemed justified.”
It is also important to emphasize that 54% were cured immediately, but only 40% in long-term follow-up. This is not about cure for all patients, this is about increased survival, which Dr. Norton did point out. Some judgment is still required; 75% of people not operated on are alive at 10 years, so selectivity remains a judgment call. It is interesting that the 10-year survival in the 1982 paper presented here was also 70%. And most patients were treated with cimetidine.
The best data, however, that Dr. Norton provides that there is a difference is that there was a marked decrease in the prevalence of liver metastasis in those undergoing primary operation and that death from disease is decreased in the surgery group. Dr. Norton, you made no comment about operative morbidity or mortality. Can you comment on that?
So while patient selection may be the reason for these impressive results, Dr. Norton has, I believe, made a very persuasive argument for an aggressive operative approach to patients with these lesions. It does allow selectivity. But I congratulate him and his coauthors on the diligence with which the follow-up has been performed, and it is wonderful that he has adhered to this long-term interest begun so many years ago.
My final question is a little bit off the presentation, but it is one that we all struggle with both in functional and nonfunctional neuroendocrine tumors in the familial setting. Dr. Norton excluded patients who had tumors less than 2.5 cm. I have historically only done that for tumors at 4 cm. So I ask him, does he still keep to that role in the familial disease?
Dr. Jeffrey A. Norton (Stanford, California): The cimetidine patients were not included in this study. The study began in 1982 right after your paper with the cimetidine. The operative mortality was zero. But the morbidity was significant. It was approximately 20% to 30%. There was no long-term morbidity. It was only postoperative morbidity.
In MEN 1 patients we still hold to the 2- to 2.5-cm tumor size for doing surgery. The reason we developed that number is if the tumor gets to be 3 to 4 cm in size, patients have a significant probability (30% to 40%) of developing liver metastases. So we try to operate on the patients when they have clearly identifiable tumor without liver metastases. The other reason is the cure rate in MEN 1 patients is zero. So we try to operate only if they have clearly identifiable tumor.
Dr. Keith D. Lillemoe (Indianapolis, Indiana): Dr. Norton, that was a very nice paper. It actually just touched on my question, which is related to your strategy with the MEN I patients. As you know, imaging studies are getting better, and smaller and smaller tumors are being identified. Patients are seeing data like this and able to see improved cure rates by surgical resection even with MEN 1. You talked a little about your strategies. Does your study shed any light on the management of MEN 1 patients with this gastrinomas?
Dr. Jeffrey A. Norton (Stanford, California): Our study indicates that we are prolonging the survival of MEN 1 patients by doing surgery when a neuroendocrine tumor measures 2 to 2.5 cm. It suggests that the surgery is indicated for MEN 1 patients with identifiable tumors. It is not clear what is the best tumor size, but we used a size between 2 and 2.5 cm.
Dr. E. Christopher Ellison (Columbus, Ohio): Another outstanding paper with tremendous contributions in this area. I had basically 2 questions. First, how many of the patients who had no tumor identified at surgery lived for a prolonged period of time? In other words, what was the survival of that group? And do you think that patients that have negative imaging should undergo routine exploration, or should they be observed, given the natural history of this disease?
Dr. Jeffrey A. Norton (Stanford, California): The patients with no tumor identified did well, as did the other patients. The survival was almost identical. Those patients probably had duodenal gastrinomas missed because we started doing duodenotomy; that is, opening the duodenum as Dr. Norman Thompson described in 1996, and after that we found tumor in every single patient. So I do recommend surgery for sporadic patients who have clear biochemical evidence of Zollinger Ellison syndrome but have no tumor identified on imaging. They probably will have a small duodenal gastrinoma that we can find and remove.
Footnotes
Reprints: Jeffrey A. Norton, MD, Stanford University Medical Center, Department of Surgery, Room H-3591, 300 Pasteur Drive, Stanford, CA 94305-5641. E-mail: janorton@stanford.edu.
REFERENCES
- 1.Zollinger RM, Ellison EH. Primary peptic ulcerations of the jejunum associated with islet cell tumors of the pancreas. Ann Surg. 1955;142:709–728. [PMC free article] [PubMed] [Google Scholar]
- 2.Fox PS, Hofmann JW, Wilson SD, et al. Surgical management of the Zollinger-Ellison syndrome. Surg Clin North Am. 1974;54:395–407. [DOI] [PubMed] [Google Scholar]
- 3.Oberhelman HA Jr, Nelsen TS, Johnson AN, et al. Ulcerogenic tumors of the duodenum. Ann Surg. 1961;153:214–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oberhelman HA Jr. Excisional therapy for ulcerogenic tumors of the duodenum: long- term results. Arch Surg. 1972;104:447–453. [DOI] [PubMed] [Google Scholar]
- 5.McCarthy DM. The place of surgery in the Zollinger-Ellison syndrome. N Engl J Med. 1980;302:1344–1347. [DOI] [PubMed] [Google Scholar]
- 6.Jensen RT, Doppman JL, Gardner JD, et al. eds. The Exocrine Pancreas: Biology, Pathobiology and Disease. New York: Raven Press, 1986:727–744. [Google Scholar]
- 7.Hirschowitz BI. Clinical course of nonsurgically treated Zollinger-Ellison syndrome. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Frontiers of Gastrointestinal Research. Basel, Switzerland: Karger, 1995:360–371. [Google Scholar]
- 8.Norton JA, Fraker DL, Alexander HR, et al. Surgery to cure the Zollinger-Ellison syndrome. N Engl J Med. 1999;341:635–644. [DOI] [PubMed] [Google Scholar]
- 9.Collen MJ, Howard JM, McArthur KE, et al. Comparison of ranitidine and cimetidine in the treatment of gastric hypersecretion. Ann Intern Med. 1984;100:52–58. [DOI] [PubMed] [Google Scholar]
- 10.Jensen RT. Use of omeprazole and other proton pump inhibitors in the Zollinger-Ellison syndrome. In: Olbe L, ed. Milestones in Drug Therapy. Basel, Switzerland: Birkhauser Verlag, 1999:205–221. [Google Scholar]
- 11.Stabile BE, Passaro E Jr. Benign and malignant gastrinoma. Am J Surg. 1985;49:144–150. [DOI] [PubMed] [Google Scholar]
- 12.Norton JA, Jensen RT. Resolved and unresolved controversies in the surgical management of patients with Zollinger-Ellison syndrome. Ann Surg. 2004;240:757–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu F, Venzon DJ, Serrano J, et al. Prospective study of the clinical course, prognostic factors and survival in patients with longstanding Zollinger-Ellison syndrome. J Clin Oncol. 1999;17:615–630. [DOI] [PubMed] [Google Scholar]
- 14.Weber HC, Venzon DJ, Lin JT, et al. Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Gastroenterology. 1995;108:1637–1649. [DOI] [PubMed] [Google Scholar]
- 15.Norton JA, Alexander HA, Fraker DL, et al. Possible primary lymph node gastrinomas. Occurrence, natural history and predictive factors: a prospective study. Ann Surg. 2003;237:650–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norton JA, Alexander HR, Fraker DL, et al. Does the use of routine duodenotomy (DUODX) affect rate of cure, development of liver metastases or survival in patients with Zollinger-Ellison syndrome (ZES)? Ann Surg. 2004;239:617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norton JA, Doppman JL, Jensen RT. Curative resection in Zollinger-Ellison syndrome: results of a 10-year prospective study. Ann Surg. 1992;215:8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirschowitz BI, Simmons J, Mohnen J. Clinical outcome using lansoprazole in acid hypersecretors with and without Zollinger-Ellison syndrome: a 13-year prospective study. Clin Gastroenterol Hepatol. 2005;3:39–48. [DOI] [PubMed] [Google Scholar]
- 19.Fraker DL, Norton JA, Alexander HR, et al. Surgery in Zollinger-Ellison syndrome alters the natural history of gastrinoma. Ann Surg. 1994;220:320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norton JA, Doppman JL, Collen MJ, et al. Prospective study of gastrinoma localization and resection in patients with Zollinger-Ellison syndrome. Ann Surg. 1986;204:468–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sugg SL, Norton JA, Fraker DL, et al. A prospective study of intraoperative methods to diagnose and resect duodenal gastrinomas. Ann Surg. 1993;218:138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Norton JA, Alexander HR, Fraker DL, et al. Comparison of surgical results in patients with advanced and limited disease with multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome. Ann Surg. 2001;234:495–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacFarlane MP, Fraker DL, Alexander HR, et al. A prospective study of surgical resection of duodenal and pancreatic gastrinomas in multiple endocrine neoplasia-Type 1. Surgery. 1995;118:973–980. [DOI] [PubMed] [Google Scholar]
- 24.Fishbeyn VA, Norton JA, Benya RV, et al. Assessment and prediction of long-term cure in patients with Zollinger-Ellison syndrome: the best approach. Ann Intern Med. 1993;119:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy P, Venzon DJ, Feigenbaum KM, et al. Gastric secretion in Zollinger-Ellison syndrome. Correlation with clinical expression, tumor extent and role in diagnosis: a prospective NIH study of 235 patients and review of the literature in 984 cases. Medicine (Baltimore). 2001;80:189–222. [DOI] [PubMed] [Google Scholar]
- 26.Roy P, Venzon DJ, Shojamanesh H, et al. Zollinger-Ellison syndrome: clinical presentation in 261 patients. Medicine. 2000;79:379–411. [DOI] [PubMed] [Google Scholar]
- 27.Raufman JP, Collins SM, Pandol SJ, et al. Reliability of symptoms in assessing control of gastric acid secretion in patients with Zollinger-Ellison syndrome. Gastroenterology. 1983;84:108–113. [PubMed] [Google Scholar]
- 28.Metz DC, Pisegna JR, Fishbeyn VA, et al. Currently used doses of omeprazole in Zollinger-Ellison syndrome are too high. Gastroenterology. 1992;103:1498–1508. [DOI] [PubMed] [Google Scholar]
- 29.Gibril F, Schumann M, Pace A, et al. Multiple endocrine neoplasia type 1 and Zollinger-Ellison syndrome: a prospective study of 107 cases and comparison with 1009 patients from the literature. Medicine. 2004;83:43–83. [DOI] [PubMed] [Google Scholar]
- 30.Orbuch M, Doppman JL, Strader DB, et al. Imaging for pancreatic endocrine tumor localization: recent advances. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Frontiers of Gastrointestinal Research. Basel, Switzerland: Karger, 1995:268–281. [Google Scholar]
- 31.Alexander HR, Fraker DL, Norton JA, et al. Prospective study of somatostatin receptor scintigraphy and its effect on operative outcome in patients with Zollinger-Ellison syndrome. Ann Surg. 1998;228:228–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Termanini B, Gibril F, Reynolds JC, et al. Value of somatostatin receptor scintigraphy: a prospective study in gastrinoma of its effect on clinical management. Gastroenterology. 1997;112:335–347. [DOI] [PubMed] [Google Scholar]
- 33.Strader DB, Doppman JL, Orbuch M, et al. Functional localization of pancreatic endocrine tumors. In: Mignon M, Jensen RT, eds. Endocrine Tumors of the Pancreas: Recent Advances in Research and Management. Frontiers of Gastrointestinal Research. Basel, Switzerland: Karger, 1995:282–297. [Google Scholar]
- 34.Cherner JA, Doppman JL, Norton JA, et al. Selective venous sampling for gastrin to localize gastrinomas: a prospective study. Ann Intern Med. 1986;105:841–847. [DOI] [PubMed] [Google Scholar]
- 35.Thom AK, Norton JA, Doppman JL, et al. Prospective study of the use of intraarterial secretin injection and portal venous sampling to localize duodenal gastrinomas. Surgery. 1992;112:1002–1008. [PubMed] [Google Scholar]
- 36.Benya RV, Metz DC, Venzon DJ, et al. Zollinger-Ellison syndrome can be the initial endocrine manifestation in patients with multiple endocrine neoplasia-type 1. Am J Med. 1994;97:436–444. [DOI] [PubMed] [Google Scholar]
- 37.Norton JA, Cornelius MJ, Doppman JL, et al. Effect of parathyroidectomy in patients with hyperparathyroidism, Zollinger-Ellison syndrome and multiple endocrine neoplasia Type I: a prospective study. Surgery. 1987;102:958–966. [PubMed] [Google Scholar]
- 38.Norton JA, Cromack DT, Shawker TH, et al. Intraoperative ultrasonographic localization of islet cell tumors: a prospective comparison to palpation. Ann Surg. 1988;207:160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frucht H, Norton JA, London JF, et al. Detection of duodenal gastrinomas by operative endoscopic transillumination: a prospective study. Gastroenterology. 1990;99:1622–1627. [DOI] [PubMed] [Google Scholar]
- 40.Arnold WS, Fraker DL, Alexander HR, et al. Apparent lymph node primary gastrinoma. Surgery. 1994;116:1123–1130. [PubMed] [Google Scholar]
- 41.Norton JA, Doherty GM, Fraker DL, et al. Surgical treatment of localized gastrinoma within the liver: a prospective study. Surgery. 1998;124:1145–1152. [DOI] [PubMed] [Google Scholar]
- 42.Norton JA, Sugarbaker PH, Doppman JL, et al. Aggressive resection of metastatic disease in selected patients with malignant gastrinoma. Ann Surg. 1986;203:352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jaskowiak NT, Fraker DL, Alexander HR, et al. Is reoperation for gastrinoma excision in Zollinger-Ellison syndrome (ZES) indicated? Surgery. 1996;120:1057–1063. [DOI] [PubMed] [Google Scholar]
- 44.Maton PN, Miller DL, Doppman JL, et al. Role of selective angiography in the management of Zollinger- Ellison syndrome. Gastroenterology. 1987;92:913–918. [DOI] [PubMed] [Google Scholar]
- 45.Miller LS, Vinayek R, Frucht H, et al. Reflux esophagitis in patients with Zollinger-Ellison syndrome. Gastroenterology. 1990;98:341–346. [DOI] [PubMed] [Google Scholar]
- 46.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 47.Rothman KJ. Estimation of confidence limits for the cumulative probability of survival in life table analysis. J Chron Dis. 1978;31:557–560. [DOI] [PubMed] [Google Scholar]
- 48.Aalen O. Nonparametic estimation of partial transition probabilities in multiple decrement models. Ann. Stat. 1978;6:534–545. [Google Scholar]
- 49.Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;51:524–532. [PubMed] [Google Scholar]
- 50.Howard TJ, Zinner MJ, Stabile BE, et al. Gastrinoma excision for cure: a prospective analysis. Ann Surg. 1990;211:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jensen RT. Zollinger-Ellison syndrome. In: Doherty GM, Skogseid B, eds. Surgical Endocrinology: Clinical Syndromes. Philadelphia: Lippincott Williams & Wilkins, 2001:291–344. [Google Scholar]
- 52.Zollinger RM, Ellison EC, Fabri PJ, et al. Primary peptic ulcerations of the jejunum associated with islet cell tumors: twenty-five-year appraisal. Ann Surg. 1980;192:422–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thompson JC, Lewis BG, Wiener I, et al. The role of surgery in the Zollinger-Ellison syndrome. Ann Surg. 1983;197:594–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ellison EH, Wilson SD. The Zollinger-Ellison syndrome: re-appraisal and evaluation of 260 registered cases. Ann Surg. 1964;160:512–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Creutzfeldt W, Arnold R, Creutzfeldt C, et al. Pathomorphologic, biochemical and diagnostic aspects of gastrinomas (Zollinger-Ellison syndrome). Hum Pathol. 1975;6:47–76. [DOI] [PubMed] [Google Scholar]
- 56.Jensen RT. Natural history of digestive endocrine tumors. In: Mignon M, Colombel JF, eds. Recent Advances in Pathophysiology and Management of Inflammatory Bowel Diseases and Digestive Endocrine Tumors. Paris: John Libbey, 1999:192–219. [Google Scholar]
- 57.Gibril F, Venzon DJ, Ojeaburu JV, et al. Prospective study of the natural history of gastrinoma in patients with MEN1: definition of an aggressive and a nonaggressive form. J Clin Endocrinol Metab. 2001;86:5282–5293. [DOI] [PubMed] [Google Scholar]
- 58.Zollinger RM, Martin EW Jr, Carey LC, et al. Observations on the postoperative tumor growth behavior of certain islet cell tumors. Ann Surg. 1976;184:525–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jensen RT, Gardner JD. Gastrinoma. In: Go VLW, DiMagno EP, Gardner JD, et al. eds. The Pancreas: Biology, Pathobiology and Disease. New York: Raven Press, 1993:931–978. [Google Scholar]
- 60.Sutliff VE, Doppman JL, Gibril F, et al. Growth of newly diagnosed, untreated metastatic gastrinomas and predictors of growth patterns. J Clin Oncol. 1997;15:2420–2431. [DOI] [PubMed] [Google Scholar]