Abstract
Aim
To investigate the association between central corneal thickness (CCT) and the degree of myopia among Chinese.
Methods
In this prospective observational study, 714 consecutive patients were recruited from a refractive surgery clinic. CCT was measured in both eyes of each patient using the Orbscan (Bausch and Lomb, Rochester, New York, USA), and data of the right eye were selected for analysis. CCT was correlated with the degree of myopia in dioptres (D) using Pearson's correlation coefficient and Dunnett's t test with multiple comparisons.
Results
The age of the patients ranged from 15 to 59 years. The mean CCT was 534.5 μm, with a standard deviation (SD) of 38.1 (range 305–684) μm. The mean (SD) myopic spherical equivalent was 5.30 (2.74) D, range −17.5–−0.625 D. No correlation was found between CCT and the degree of myopia (r = −0.13, p = 0.719).
Conclusions
Among Chinese with myopia, CCT was distributed over a large range but did not correlate with the degree of myopia.
Myopia is increasing in prevalence among the populations of East Asian origin. Estimates of the proportion of myopia in the young population of Singapore range from 30% to 65%,1,2 and the prevalence was found to be greater among the Chinese,3,4 and to increase with higher educational achievements.3,4 With increasing rates of myopia, refractive surgery such as laser in situ keratomileusis (LASIK) has become popular in Asia. When undertaking such surgery to correct myopia, central corneal thickness (CCT) is an important consideration to prevent the cornea from becoming too thin after treatment.
Studies that have attempted to investigate the effect of refractive errors on CCT have reported conflicting results. One report showed no correlation between corneal thickness and the level of myopia,5 whereas another study found the cornea to be thinner in more myopic eyes.6 The two studies used different techniques of measuring CCT and there was some variability in the study population. The aim of this study was to prospectively investigate the relationship between CCT and the degree of myopia in a large sample of Asian adults with myopia who were being assessed for refractive surgery.
Methods
Patients consisted of 714 consecutive ethnic Chinese refractive surgery candidates who presented at a refractive surgery clinic for LASIK assessment. The institutional review board provided approval for the protocol of this study and written informed consent was obtained from all patients. Exclusion criteria were previous ocular surgery, ocular pathology such as keratoconus or glaucoma, or recent contact lens wear in the previous 2 weeks.
Manifest refraction and CCT measurements with the Orbscan II (Bausch and Lomb, Rochester, New York, USA) were carried out on both eyes of all the patients. Only data from the right eyes were used in the analysis. Pearson correlation analysis was carried out to examine the relationship between the degree of myopia and CCT. The Dunnett t test (two‐sided) multiple comparisons were used to compare CCT among the classes of myopes, such as 0 to –4 D, −4 to –8 D and >–8 D, with the last group being used as the test group. A similar comparison was made of the degree of myopia among CCT groups, such as those <500 μm, 500–550 μm, 550–600 μm and >600 μm. Data were analysed using SPSS V.11.0, and significance was assumed at p<0.05.
Results
A total of 714 patients were recruited. All patients were Chinese, most were women (66.7%) and the mean age of the patients was 32.9 (range 15–59) years. The distributions of CCT and spherical equivalent are shown in figs 1 and 2. Overall, 20 (2.8%) patients were below 2 standard deviations (SDs) from the mean—that is, 458.3 μm—and 13 (1.8%) were above 2 SDs from the mean—that is, 610.7 μm. The mean (SDs) myopic spherical equivalent was –5.30 (2.74) D, range −17.5 to −0.625 D (fig 2). Table 1 shows the demographic characteristics and degree of myopia of the study patients.
Figure 1 Histogram showing the distribution of corneal pachymetry in this study population.
Figure 2 Histogram showing the distribution of spherical equivalent in this study population.
Table 1 Demographic features and degree of myopia of study patients (n = 714).
| Sex | |
| Male | 238 (33.3%) |
| Female | 476 (66.7%) |
| Age (years) | |
| Mean (SD) | 32.9 (8.3%) |
| Range | 15.4–59.0 |
| Median | 33.0 |
| Spherical equivalent (D) | |
| >−2 to 0 | 53 (7.4%) |
| >−4 to −2 | 189 (26.5%) |
| >−6 to −4 | 225 (31.5%) |
| >−8 to −6 | 137 (19.2%) |
| ⩾−8 | 110 (15.4%) |
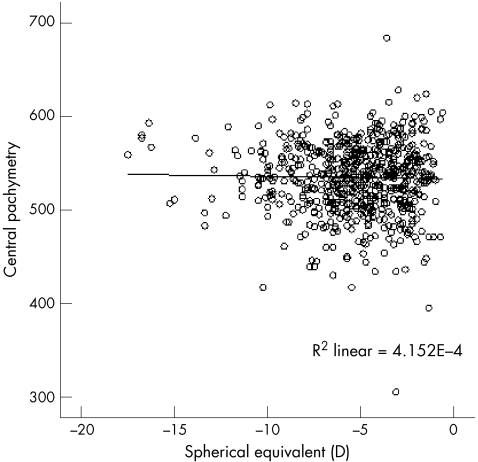
We found no correlation between CCT and the degree of myopic spherical equivalent (r = −0.13, p = 0.72). Figure 3 shows the scatter plot between the degree of myopia (in spherical equivalent) and CCT.
Figure 3 Scatter plot showing the association between central corneal thickness (CCT) and myopic spherical equivalent in the study patients. Note that there is no significant association between CCT and the degree of myopia.
When CCT was split into groups and compared with the degree of myopia, there was no significant difference. Table 2 shows the comparison of means in the myopia and CCT groups.
Table 2 Comparison of myopia group and central corneal thickness (CCT) group.
| Compared groups | Number | Mean (SD) | Range | p Value | |
|---|---|---|---|---|---|
| Myopia groups | CCT μm | ||||
| 1 | 0 to –4 D | 258 | 536.6 (42.7) | 305–684 | 0.48*? |
| 2 | >–4 to –8 D | 349 | 531 (35.5) | 417–613 | 0.04* |
| 3 | >–8 D* | 107 | 540.9 (33.7) | 417–614 | NA |
| CCT groups | Myopia (D) | ||||
| 1 | <500 μm | 112 | −5.1 (2.5) | −0.75––13.37 | 0.52 |
| 2 | 500 to <550 μm | 345 | −5.3 (2.6) | −1––15.25 | |
| 3 | 550 to 600 μm | 237 | −5.5 (3) | −0.75––17.5 | |
| 4 | >600 μm | 20 | −4.7 (2.9) | −0.63––9.88 |
*The group compared with the other groups in the Dunnett t test (two sided). †Overall significance level was p = 0.04.
Discussion
This study reports a large series of CCT measurements over a large range of myopic refractive error in Chinese patients. The mean CCT of these young adults with myopia was 9.1 μm less than that reported in Singaporean school children and 12.6 μm less than that of another sample of Singaporean adults (mean CCTs of Singaporean school children and Singaporean adults 543.6 and 547.1 μm, respectively).5,7 However, the method used for CCT measurement in those studies was optical pachymetry. von Bahr7 first generated interest in this type of patient when he reported thinner corneas in myopia of <−4 D.8 Similar findings were also reported by Tokoro et al9 and Chang et al.6 However, other studies by Liu et al and Pflugfelder,10 Price et al11 and Pedersen et al12 could find no correlation between CCT and the degree of myopia as reported in our study.
The mean CCT in our series was very close (1.5 μm difference) to that found in Chang's series,6 which had a mean of 533 μm. However, in the study by Price et al11 in which patients were Caucasian, the mean CCT was thicker (mean of 550 μm). Recently, Vijaya et al13 reported the mean (SD) CCT in a normal rural south Indian population to be 505.9 (31.1) μm. Further, racial variation in CCT has been reported, with African Americans having thinner corneas on average than Caucasians. Hence, this may suggest an ethnic difference in CCT between Asians and Caucasians with myopia, similar to reports among normal populations.14,15
The relationship between CCT and intraocular pressure has been a much deliberated.16 The prevalent risk of glaucoma in myopes seems to be higher than in a normal population, and CCT may be important in this context.17 The report by Quigley et al18 on the morphology of the lamina cribrosa correlating with neural loss in open angle glaucoma draws attention to the possible predisposition of people with myopia towards a thin scleral bed of lamina cribrosa, and to a higher risk of glaucoma. Shimmoyo and Orloff,19 in a study of 546 patients correlating axial length and CCT, found that the intraocular pressure measured by applanation tonometry in these eyes can have an error of up to 14 mm Hg using Ehler's correction. This indicates that caution should be exercised in interpreting risk of glaucoma associated with people with myopia with thin corneas.
Our study has a few limitations. The axial lengths of the patients were not been measured to differentiate people with axial myopia from those with index myopia. However, the study patients were recruited from a refractive surgery clinic and comprised patients with myopia who were assessed for LASIK; such patients are not expected to have index myopia. We have not used an emmetropic sample for comparison; however, we tried to compare our data with population‐based study data from the same region.
In conclusion, our study has shown that CCT has no correlation with myopia in Chinese adults; however, CCT values seem to be less than values reported in Caucasians. This information may be useful for refractive surgeons when selecting patients for refractive surgery.
Abbreviations
CCT - central corneal thickness
LASIK - laser in situ keratomileusis
Footnotes
Funding: TA is supported by the National Medical Research Council, Singapore.
Competing interests: None declared.
References
- 1.Saw S M, Katz J, Schein O D.et al Epidemiology of myopia. Epidemiol Rev 199618175–187. [DOI] [PubMed] [Google Scholar]
- 2.Chow Y C, Dhillon B, Chew P T.et al Refractive errors in Singapore medical students. Singapore Med J 199031472–473. [PubMed] [Google Scholar]
- 3.Wensor M, McCarty C A, Taylor H R. Prevalence and risk factors of myopia in Victoria, Australia. Arch Ophthalmol 1999117658–663. [DOI] [PubMed] [Google Scholar]
- 4.Sperduto R D, Seigel D, Roberts J.et al Prevalence of myopia in the United States. Arch Ophthalmol 1983101405–407. [DOI] [PubMed] [Google Scholar]
- 5.Tong L, Saw S M, Siak J K.et al Corneal thickness determination and correlates in Singaporean schoolchildren. Invest Ophthalmol Vis Sci 2004454004–4009. [DOI] [PubMed] [Google Scholar]
- 6.Chang S W, Tsai I L, Hu F R.et al The cornea in young myopic adults. Br J Ophthamol 200185916–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foster P J, Machin D, Wong T Y.et al Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest Ophthalmol Vis Sci 2003443885–3891. [DOI] [PubMed] [Google Scholar]
- 8.von Bahr G. Corneal thickness: its measurement and changes. Am J Ophthalmol 195642251–266. [PubMed] [Google Scholar]
- 9.Tokoro T, Hayashi K, Muto M.et al Central corneal thickness in high myopia. Folia Ophthalmol Jpn 197627610 [Google Scholar]
- 10.Liu Z, Pflugfelder S C. The effects of long‐term contact lens wear on corneal thickness, curvature, and surface regularity. Ophthalmology 2000107105–111. [DOI] [PubMed] [Google Scholar]
- 11.Price F W, Jr, Koller D L, Price M O. Central corneal pachymetry in patients undergoing laser in situ keratomilieusis. Opthalmology 19991062216–2220. [DOI] [PubMed] [Google Scholar]
- 12.Pederson L, Hjortdal J, Ehlers N. Central corneal thickness in high myopia. Acta Ophthalmol Scand 200583539–542. [DOI] [PubMed] [Google Scholar]
- 13.Vijaya L, George R, Paul P G.et al Prevalence of open‐angle glaucoma in a rural South Indian population. Invest Ophthalmol Vis Sci 2005464461–4467. [DOI] [PubMed] [Google Scholar]
- 14.Aghaian E, Choe J E, Lin S.et al Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology 20041112211–2219. [DOI] [PubMed] [Google Scholar]
- 15.Yo C, Ariyasu R G. Racial differences in central corneal thickness and refraction among refractive surgery candidates. J Refract Surg 200521194. [DOI] [PubMed] [Google Scholar]
- 16.Gordon M O, Beiser L A, Brandt J D.et al The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open‐angle glaucoma. Arch Ophthalmol 2002120829–830. [DOI] [PubMed] [Google Scholar]
- 17.Saw S M, Gazzard G, Shih‐Yen E C.et al Myopia and associated pathological complications. Ophthalmic Physiol Opt 200525381–391. [DOI] [PubMed] [Google Scholar]
- 18.Quigley H A, Hahman R M, Addicks E M.et al Morphologic changes in the lamina cribrosa correlated with neural loss in open‐angle glaucoma. Am J Ophthalmol 198395673–691. [DOI] [PubMed] [Google Scholar]
- 19.Shimmoyo M, Orloff P N. Corneal thickness and axial length. Am J Ophthalmol 2005139553–554. [DOI] [PubMed] [Google Scholar]