Abstract
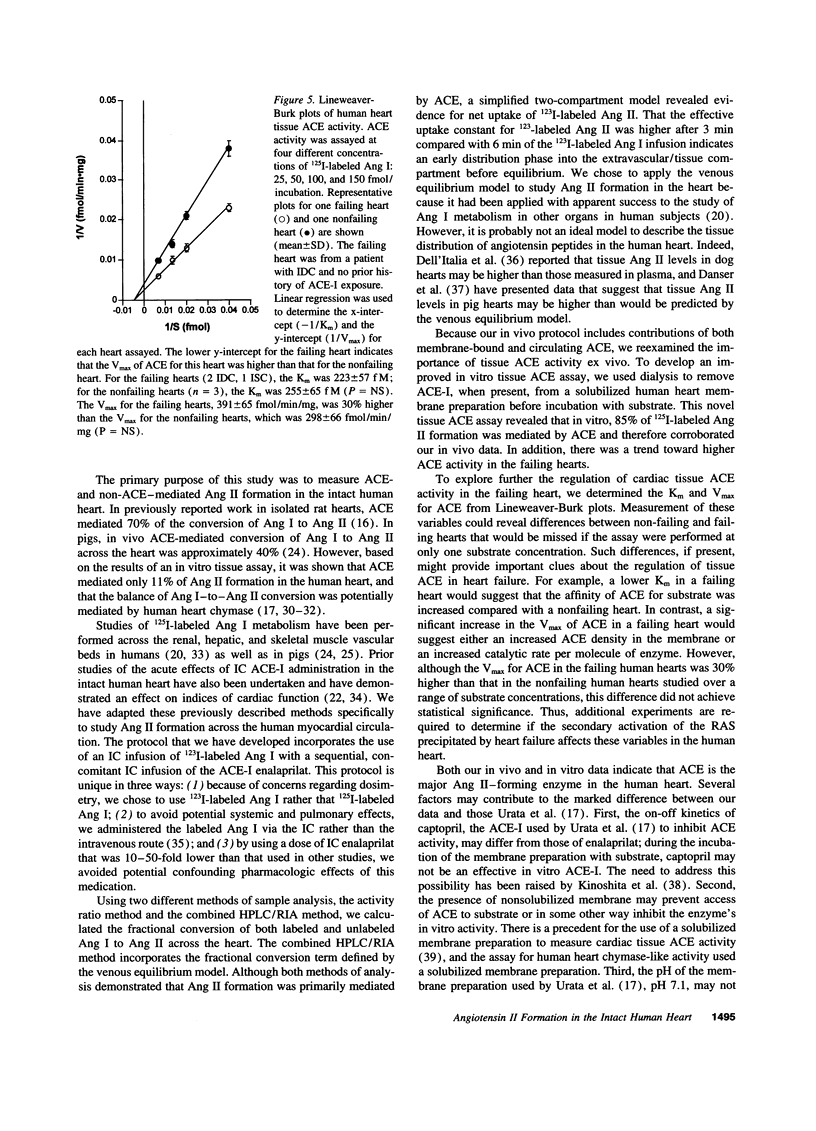
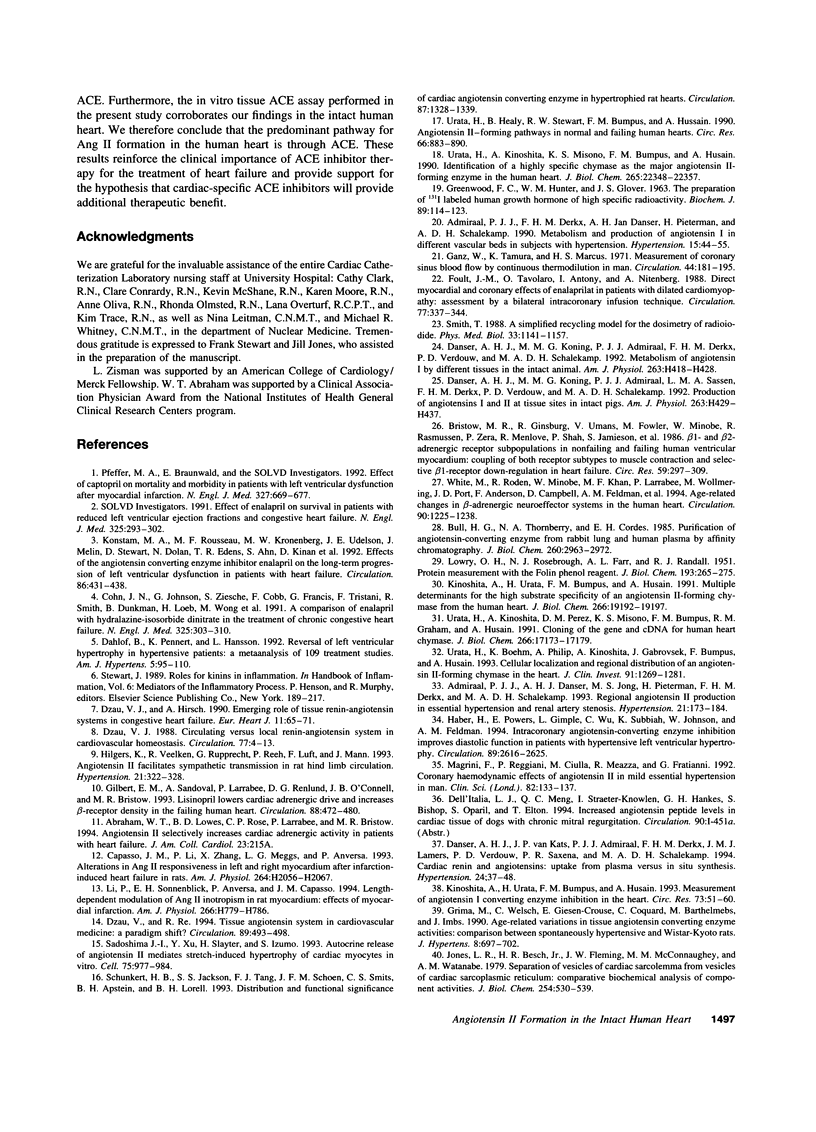
It has been proposed that the contribution of myocardial tissue angiotensin converting enzyme (ACE) to angiotensin II (Ang II) formation in the human heart is low compared with non-ACE pathways. However, little is known about the actual in vivo contribution of these pathways to Ang II formation in the human heart. To examine angiotensin II formation in the intact human heart, we administered intracoronary 123I-labeled angiotensin I (Ang I) with and without intracoronary enalaprilat to orthotopic heart transplant recipients. The fractional conversion of Ang I to Ang II, calculated after separation of angiotensin peptides by HPLC, was 0.415 +/- 0.104 (n = 5, mean +/- SD). Enalaprilat reduced fractional conversion by 89%, to a value of 0.044 +/- 0.053 (n = 4, P = 0.002). In a separate study of explanted hearts, a newly developed in vitro Ang II-forming assay was used to examine cardiac tissue ACE activity independent of circulating components. ACE activity in solubilized left ventricular membrane preparations from failing hearts was 49.6 +/- 5.3 fmol 125I-Ang II formed per minute per milligram of protein (n = 8, +/- SE), and 35.9 +/- 4.8 fmol/min/mg from nonfailing human hearts (n = 7, P = 0.08). In the presence of 1 microM enalaprilat, ACE activity was reduced by 85%, to 7.3 +/- 1.4 fmol/min/mg in the failing group and to 4.6 +/- 1.3 fmol/min/mg in the nonfailing group (P < 0.001). We conclude that the predominant pathway for angiotensin II formation in the human heart is through ACE.
Full text
PDF





Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Admiraal P. J., Danser A. H., Jong M. S., Pieterman H., Derkx F. H., Schalekamp M. A. Regional angiotensin II production in essential hypertension and renal artery stenosis. Hypertension. 1993 Feb;21(2):173–184. doi: 10.1161/01.hyp.21.2.173. [DOI] [PubMed] [Google Scholar]
- Admiraal P. J., Derkx F. H., Danser A. H., Pieterman H., Schalekamp M. A. Metabolism and production of angiotensin I in different vascular beds in subjects with hypertension. Hypertension. 1990 Jan;15(1):44–55. doi: 10.1161/01.hyp.15.1.44. [DOI] [PubMed] [Google Scholar]
- Altura B. M., Altura B. T. Vascular smooth muscle and prostaglandins. Fed Proc. 1976 Oct;35(12):2360–2366. [PubMed] [Google Scholar]
- Bristow M. R., Ginsburg R., Umans V., Fowler M., Minobe W., Rasmussen R., Zera P., Menlove R., Shah P., Jamieson S. Beta 1- and beta 2-adrenergic-receptor subpopulations in nonfailing and failing human ventricular myocardium: coupling of both receptor subtypes to muscle contraction and selective beta 1-receptor down-regulation in heart failure. Circ Res. 1986 Sep;59(3):297–309. doi: 10.1161/01.res.59.3.297. [DOI] [PubMed] [Google Scholar]
- Bull H. G., Thornberry N. A., Cordes E. H. Purification of angiotensin-converting enzyme from rabbit lung and human plasma by affinity chromatography. J Biol Chem. 1985 Mar 10;260(5):2963–2972. [PubMed] [Google Scholar]
- Capasso J. M., Li P., Zhang X., Meggs L. G., Anversa P. Alterations in ANG II responsiveness in left and right myocardium after infarction-induced heart failure in rats. Am J Physiol. 1993 Jun;264(6 Pt 2):H2056–H2067. doi: 10.1152/ajpheart.1993.264.6.H2056. [DOI] [PubMed] [Google Scholar]
- Caruso A., Ferrazzani S., De Carolis S., Lanzone A., Mancuso S. Low-dose aspirin and vascular response in pregnant patients sensitive to angiotensin II. Int J Gynaecol Obstet. 1991 Jun;35(2):123–128. doi: 10.1016/0020-7292(91)90814-l. [DOI] [PubMed] [Google Scholar]
- Cody R. J., Covit A. B., Schaer G. L., Laragh J. H. Estimation of angiotensin II receptor activity in chronic congestive heart failure. Am Heart J. 1984 Jul;108(1):81–89. doi: 10.1016/0002-8703(84)90548-9. [DOI] [PubMed] [Google Scholar]
- Cohn J. N., Johnson G., Ziesche S., Cobb F., Francis G., Tristani F., Smith R., Dunkman W. B., Loeb H., Wong M. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991 Aug 1;325(5):303–310. doi: 10.1056/NEJM199108013250502. [DOI] [PubMed] [Google Scholar]
- Dahlöf B., Pennert K., Hansson L. Reversal of left ventricular hypertrophy in hypertensive patients. A metaanalysis of 109 treatment studies. Am J Hypertens. 1992 Feb;5(2):95–110. doi: 10.1093/ajh/5.2.95. [DOI] [PubMed] [Google Scholar]
- Danser A. H., Koning M. M., Admiraal P. J., Derkx F. H., Verdouw P. D., Schalekamp M. A. Metabolism of angiotensin I by different tissues in the intact animal. Am J Physiol. 1992 Aug;263(2 Pt 2):H418–H428. doi: 10.1152/ajpheart.1992.263.2.H418. [DOI] [PubMed] [Google Scholar]
- Danser A. H., Koning M. M., Admiraal P. J., Sassen L. M., Derkx F. H., Verdouw P. D., Schalekamp M. A. Production of angiotensins I and II at tissue sites in intact pigs. Am J Physiol. 1992 Aug;263(2 Pt 2):H429–H437. doi: 10.1152/ajpheart.1992.263.2.H429. [DOI] [PubMed] [Google Scholar]
- Danser A. H., van Kats J. P., Admiraal P. J., Derkx F. H., Lamers J. M., Verdouw P. D., Saxena P. R., Schalekamp M. A. Cardiac renin and angiotensins. Uptake from plasma versus in situ synthesis. Hypertension. 1994 Jul;24(1):37–48. doi: 10.1161/01.hyp.24.1.37. [DOI] [PubMed] [Google Scholar]
- Dzau V. J. Circulating versus local renin-angiotensin system in cardiovascular homeostasis. Circulation. 1988 Jun;77(6 Pt 2):I4–13. [PubMed] [Google Scholar]
- Dzau V. J., Hirsch A. T. Emerging role of the tissue renin-angiotensin systems in congestive heart failure. Eur Heart J. 1990 Apr;11 (Suppl B):65–71. doi: 10.1093/eurheartj/11.suppl_b.65. [DOI] [PubMed] [Google Scholar]
- Dzau V. J., Re R. Tissue angiotensin system in cardiovascular medicine. A paradigm shift? Circulation. 1994 Jan;89(1):493–498. doi: 10.1161/01.cir.89.1.493. [DOI] [PubMed] [Google Scholar]
- Foult J. M., Tavolaro O., Antony I., Nitenberg A. Direct myocardial and coronary effects of enalaprilat in patients with dilated cardiomyopathy: assessment by a bilateral intracoronary infusion technique. Circulation. 1988 Feb;77(2):337–344. doi: 10.1161/01.cir.77.2.337. [DOI] [PubMed] [Google Scholar]
- GREENWOOD F. C., HUNTER W. M., GLOVER J. S. THE PREPARATION OF I-131-LABELLED HUMAN GROWTH HORMONE OF HIGH SPECIFIC RADIOACTIVITY. Biochem J. 1963 Oct;89:114–123. doi: 10.1042/bj0890114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz W., Tamura K., Marcus H. S., Donoso R., Yoshida S., Swan H. J. Measurement of coronary sinus blood flow by continuous thermodilution in man. Circulation. 1971 Aug;44(2):181–195. doi: 10.1161/01.cir.44.2.181. [DOI] [PubMed] [Google Scholar]
- Gilbert E. M., Sandoval A., Larrabee P., Renlund D. G., O'Connell J. B., Bristow M. R. Lisinopril lowers cardiac adrenergic drive and increases beta-receptor density in the failing human heart. Circulation. 1993 Aug;88(2):472–480. doi: 10.1161/01.cir.88.2.472. [DOI] [PubMed] [Google Scholar]
- Grima M., Welsch C., Giesen-Crouse E. M., Coquard C., Barthelmebs M., Imbs J. L. Age-related variations in tissue angiotensin converting enzyme activities: comparison between spontaneously hypertensive and Wistar-Kyoto rats. J Hypertens. 1990 Aug;8(8):697–702. doi: 10.1097/00004872-199008000-00002. [DOI] [PubMed] [Google Scholar]
- Haber H. L., Powers E. R., Gimple L. W., Wu C. C., Subbiah K., Johnson W. H., Feldman M. D. Intracoronary angiotensin-converting enzyme inhibition improves diastolic function in patients with hypertensive left ventricular hypertrophy. Circulation. 1994 Jun;89(6):2616–2625. doi: 10.1161/01.cir.89.6.2616. [DOI] [PubMed] [Google Scholar]
- Hilgers K. F., Veelken R., Rupprecht G., Reeh P. W., Luft F. C., Mann J. F. Angiotensin II facilitates sympathetic transmission in rat hind limb circulation. Hypertension. 1993 Mar;21(3):322–328. doi: 10.1161/01.hyp.21.3.322. [DOI] [PubMed] [Google Scholar]
- Hirsch A. T., Talsness C. E., Schunkert H., Paul M., Dzau V. J. Tissue-specific activation of cardiac angiotensin converting enzyme in experimental heart failure. Circ Res. 1991 Aug;69(2):475–482. doi: 10.1161/01.res.69.2.475. [DOI] [PubMed] [Google Scholar]
- Iwai J., Kanayama Y., Inoue N. N., Okamura M., Takeda T. Increased endothelial gene expression of angiotensin AT1A receptor in cyclosporine induced hypertensive rats. Eur J Pharmacol. 1993 Dec 1;248(4):341–344. doi: 10.1016/0926-6917(93)90011-e. [DOI] [PubMed] [Google Scholar]
- Jones L. R., Besch H. R., Jr, Fleming J. W., McConnaughey M. M., Watanabe A. M. Separation of vesicles of cardiac sarcolemma from vesicles of cardiac sarcoplasmic reticulum. Comparative biochemical analysis of component activities. J Biol Chem. 1979 Jan 25;254(2):530–539. [PubMed] [Google Scholar]
- King S. J., Oparil S. Converting-enzyme inhibitors increase converting-enzyme mRNA and activity in endothelial cells. Am J Physiol. 1992 Oct;263(4 Pt 1):C743–C749. doi: 10.1152/ajpcell.1992.263.4.C743. [DOI] [PubMed] [Google Scholar]
- Kinoshita A., Urata H., Bumpus F. M., Husain A. Measurement of angiotensin I converting enzyme inhibition in the heart. Circ Res. 1993 Jul;73(1):51–60. doi: 10.1161/01.res.73.1.51. [DOI] [PubMed] [Google Scholar]
- Kinoshita A., Urata H., Bumpus F. M., Husain A. Multiple determinants for the high substrate specificity of an angiotensin II-forming chymase from the human heart. J Biol Chem. 1991 Oct 15;266(29):19192–19197. [PubMed] [Google Scholar]
- Konstam M. A., Rousseau M. F., Kronenberg M. W., Udelson J. E., Melin J., Stewart D., Dolan N., Edens T. R., Ahn S., Kinan D. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. SOLVD Investigators. Circulation. 1992 Aug;86(2):431–438. doi: 10.1161/01.cir.86.2.431. [DOI] [PubMed] [Google Scholar]
- LOWRY O. H., ROSEBROUGH N. J., FARR A. L., RANDALL R. J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951 Nov;193(1):265–275. [PubMed] [Google Scholar]
- Li P., Sonnenblick E. H., Anversa P., Capasso J. M. Length-dependent modulation of ANG II inotropism in rat myocardium: effects of myocardial infarction. Am J Physiol. 1994 Feb;266(2 Pt 2):H779–H786. doi: 10.1152/ajpheart.1994.266.2.H779. [DOI] [PubMed] [Google Scholar]
- Magrini F., Reggiani P., Ciulla M., Meazza R., Fratianni G. Coronary haemodynamic effects of angiotensin II in mild essential hypertension in man. Clin Sci (Lond) 1992 Feb;82(2):133–137. doi: 10.1042/cs0820133. [DOI] [PubMed] [Google Scholar]
- Meyer-Lehnert H., Bokemeyer D., Friedrichs U., Drechsler S., Kramer H. J. Cellular signaling by cyclosporine A in contractile cells: interactions with atrial natriuretic peptide. Clin Investig. 1993 Feb;71(2):153–160. doi: 10.1007/BF00179998. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Funakoshi T., Arakawa N., Yoshida H., Makita S., Hiramori K. Effect of angiotensin-converting enzyme inhibitors on endothelium-dependent peripheral vasodilation in patients with chronic heart failure. J Am Coll Cardiol. 1994 Nov 1;24(5):1321–1327. doi: 10.1016/0735-1097(94)90115-5. [DOI] [PubMed] [Google Scholar]
- Pfeffer M. A., Braunwald E., Moyé L. A., Basta L., Brown E. J., Jr, Cuddy T. E., Davis B. R., Geltman E. M., Goldman S., Flaker G. C. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992 Sep 3;327(10):669–677. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- Pfeilschifter J., Rüegg U. T. Cyclosporin A augments angiotensin II-stimulated rise in intracellular free calcium in vascular smooth muscle cells. Biochem J. 1987 Dec 15;248(3):883–887. doi: 10.1042/bj2480883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadoshima J., Xu Y., Slayter H. S., Izumo S. Autocrine release of angiotensin II mediates stretch-induced hypertrophy of cardiac myocytes in vitro. Cell. 1993 Dec 3;75(5):977–984. doi: 10.1016/0092-8674(93)90541-w. [DOI] [PubMed] [Google Scholar]
- Schunkert H., Ingelfinger J. R., Hirsch A. T., Pinto Y., Remme W. J., Jacob H., Dzau V. J. Feedback regulation of angiotensin converting enzyme activity and mRNA levels by angiotensin II. Circ Res. 1993 Feb;72(2):312–318. doi: 10.1161/01.res.72.2.312. [DOI] [PubMed] [Google Scholar]
- Schunkert H., Jackson B., Tang S. S., Schoen F. J., Smits J. F., Apstein C. S., Lorell B. H. Distribution and functional significance of cardiac angiotensin converting enzyme in hypertrophied rat hearts. Circulation. 1993 Apr;87(4):1328–1339. doi: 10.1161/01.cir.87.4.1328. [DOI] [PubMed] [Google Scholar]
- Semple P. F. The effects of hemorrhage and sodium depletion on plasma concentrations of angiotensin II and [des-Asp1]angiotensin II in the rat. Endocrinology. 1980 Sep;107(3):771–773. doi: 10.1210/endo-107-3-771. [DOI] [PubMed] [Google Scholar]
- Simon R., Koch M., Reil G. H., Herrmann G., Amende I., Quante W., Lichtlen P. R. Effects of intracoronary nitroglycerin on coronary vascular volume in man, assessed by a double-indicator dilution technique. Eur Heart J. 1988 Jan;9 (Suppl A):89–93. doi: 10.1093/eurheartj/9.suppl_a.89. [DOI] [PubMed] [Google Scholar]
- Smith T. A simplified recycling model for the dosimetry of radioiodide. Phys Med Biol. 1988 Oct;33(10):1141–1157. doi: 10.1088/0031-9155/33/10/004. [DOI] [PubMed] [Google Scholar]
- Studer R., Reinecke H., Müller B., Holtz J., Just H., Drexler H. Increased angiotensin-I converting enzyme gene expression in the failing human heart. Quantification by competitive RNA polymerase chain reaction. J Clin Invest. 1994 Jul;94(1):301–310. doi: 10.1172/JCI117322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlins B., Harding S. E., Kirby M. S., Poole-Wilson P. A., Williams A. J. Contamination of a cardiac sarcolemmal preparation with endothelial plasma membrane. Biochim Biophys Acta. 1986 Mar 27;856(1):137–143. doi: 10.1016/0005-2736(86)90020-9. [DOI] [PubMed] [Google Scholar]
- Urata H., Boehm K. D., Philip A., Kinoshita A., Gabrovsek J., Bumpus F. M., Husain A. Cellular localization and regional distribution of an angiotensin II-forming chymase in the heart. J Clin Invest. 1993 Apr;91(4):1269–1281. doi: 10.1172/JCI116325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urata H., Healy B., Stewart R. W., Bumpus F. M., Husain A. Angiotensin II-forming pathways in normal and failing human hearts. Circ Res. 1990 Apr;66(4):883–890. doi: 10.1161/01.res.66.4.883. [DOI] [PubMed] [Google Scholar]
- Urata H., Kinoshita A., Misono K. S., Bumpus F. M., Husain A. Identification of a highly specific chymase as the major angiotensin II-forming enzyme in the human heart. J Biol Chem. 1990 Dec 25;265(36):22348–22357. [PubMed] [Google Scholar]
- Urata H., Kinoshita A., Perez D. M., Misono K. S., Bumpus F. M., Graham R. M., Husain A. Cloning of the gene and cDNA for human heart chymase. J Biol Chem. 1991 Sep 15;266(26):17173–17179. [PubMed] [Google Scholar]
- White M., Roden R., Minobe W., Khan M. F., Larrabee P., Wollmering M., Port J. D., Anderson F., Campbell D., Feldman A. M. Age-related changes in beta-adrenergic neuroeffector systems in the human heart. Circulation. 1994 Sep;90(3):1225–1238. doi: 10.1161/01.cir.90.3.1225. [DOI] [PubMed] [Google Scholar]
- Wollert K. C., Studer R., von Bülow B., Drexler H. Survival after myocardial infarction in the rat. Role of tissue angiotensin-converting enzyme inhibition. Circulation. 1994 Nov;90(5):2457–2467. doi: 10.1161/01.cir.90.5.2457. [DOI] [PubMed] [Google Scholar]
- van Wijngaarden J., Smit A. J., de Graeff P. A., van Gilst W. H., van der Broek S. A., van Veldhuisen D. J., Lie K. I., Wesseling H. Effects of acetylsalicylic acid on peripheral hemodynamics in patients with chronic heart failure treated with angiotensin-converting enzyme inhibitors. J Cardiovasc Pharmacol. 1994 Feb;23(2):240–245. [PubMed] [Google Scholar]