Abstract
Objective
To develop, implement, and evaluate the use of virtual patients as a teaching tool for third-professional year PharmD students within an advanced elective self-care course.
Design
Practicing community pharmacists, faculty members, and pharmacy residents with alias e-mail accounts served as virtual patients and corresponded on a weekly basis via e-mail with pharmacy students regarding an assortment of fictional health concerns. Self-care inquiries were e-mailed to the students who replied and then forwarded their response to the course coordinator for evaluation and class discussion. At the end of the course, students were asked to assess the value of the learning activity.
Assessment
Students demonstrated significant improvement in knowledge, problem-solving, communication, and professional skills upon course completion. Student's assessments of the virtual patient activity have suggested positive feedback on developing self-care skills, patient interactions, and group dynamics.
Conclusion
This teaching tool was designed to enhance student's knowledge base, assessment, and counseling skills when interacting with patients in various situations. Instructor evaluation of responses, student feedback, and self-evaluation indicated the activity improved overall knowledge and communication skills.
Keywords: self-care, nonprescription drugs, virtual patients, assessment
INTRODUCTION
Nonprescription medicines account for over $15.1 billion in retail sales in 2004.1 The nonprescription drug market has changed dramatically over the past 30 years, having an additional 700 products available today that were previously available only by prescription. In conjunction with this ever-growing market, the prevalence of dietary supplement use has rapidly increased.1 Since the pharmacist is the most accessible health care resource for patients, the need to educate student pharmacists in self-care measures and effective communication skills is greater than ever.
Various methods have been used to teach communication skills, with or without a focus on nonprescription medications. These include using standardized patients to integrate knowledge with counseling and interpersonal skills in disease-state management, development of modules for written and verbal communication skills, and use of problem-based learning to create consumer web sites for nonprescription drugs.2-5 Medical curricula have employed innovative techniques for improving communication and assessment skills, including teaching clinical skills through videotape review, utilizing standardized video cases in assessing communication skills, and development of interactive virtual patients to improve communication and history-gathering skills.6-9
All students in the third-professional year of the pharmacy curriculum are required to take a 3-credit Self Care 1 course in the fall semester. The Self Care 1 syllabus covers the most prevalent nonprescription topics in practice, such as herbal pharmacotherapy, fever and pain, cough and cold, gastrointestinal ailments, and home monitoring devices. It is a required course with enrollment up to 90 students. Content is mostly lecture based; however, course activities include an in-class game of Herbal Millionaire (based on the television game show Who Wants to be a Millionaire?), round-table discussions on home monitoring devices, and break-out patient case discussions within lectures.
Beginning in the spring semester of 2003, an elective course, Self Care 2, was offered for those students interested in a career in community pharmacy practice. The course includes topics not covered in Self Care 1, such as in-depth pediatrics, pregnancy and lactation, durable medical equipment, nonprescription drugs of abuse, homeopathy, creating a self-care business plan, and evaluation of direct-to-consumer advertising. Additional learning activities include group presentations, role playing, patient cases, and hands-on training in the proper use of medical equipment. Class enrollment is typically less than half that of the required Self Care 1 course, which makes it possible to incorporate more interactive learning and small group work.
Learning objectives for the Self Care 2 course are:
(1) Further develop clinical assessment skills to evaluate appropriate patients for self-management or need for triage,
(2) Exhibit improved oral and written communication skills through providing nonprescription and nonpharmacological education,
(3) Be able to explain to patients, caregivers, and prescribers the efficacy, dosage, adverse effects, administration of nonprescription medicines, dietary supplements, and corresponding nonpharmacologic treatments for common ailments.
Within this elective, correspondence with virtual patients was added to enhance students' self-care knowledge, as well as their communication and assessment skills, through active-learning outside the classroom. The use of virtual patients allows students to have the opportunity to build on knowledge learned from previous courses and apply it to situations that commonly occur in community practice. These dynamic scenarios simulate real-life situations in a controlled, monitored setting.
DESIGN
To recruit virtual patients for the course, e-mails were sent to faculty members, community preceptors, and residents explaining the need. The only requirements to become a virtual patient were that the individual have previous experience working in community pharmacy, and time for e-mailing the students during the week. Over 60% of the volunteers were pharmacists currently in community practice outside the academic environment. Often volunteers were community preceptors looking to become more involved with teaching. Four of the faculty members who have volunteered currently had practices in family medicine, internal medicine, pediatrics, and laboratory instruction. However, all volunteers had at least some experience in community practice. Residents who served as virtual patients were ambulatory or community based, while concurrently sharing in lecturing responsibilities for the course. Over the past 2 years, former students beginning to practice in community pharmacy have asked to participate as patients, partly due to their positive experiences with the activity and their desire to become involved with teaching.
Once the virtual patients were recruited, a packet of information was disseminated to them, as well as oral instructions from the course coordinator. The materials included a detailed letter of instruction on the activity (purpose, e-mailing logistics, interacting with the students, etc), their personal virtual patient profile, and a question calendar to track interactions. They were also provided with a list of standardized topic questions and an example interaction.
Eight to 12 virtual patient personas were developed to accommodate each group of 4-5 students. Each volunteer served as 1 virtual patient. The volunteers were able to draw from their own experiences to construct scenarios similar to those encountered in the community setting. These real-life situations added an authenticity to the correspondence, presenting the students with questions they might actually encounter in practice one day.
As an initial identifier, each virtual patient was assigned an e-mail name that reflected a problem or disease state, such as Iva_Rash@yahoo.com and a baseline patient profile. Although the e-mail name provided a hint about the patient's complaint or disease, the students had to obtain the majority of information by questioning the virtual patient. The real identity of the virtual patient was never revealed to the students; therefore, the volunteers could maintain their anonymity from year to year. Students also developed self-selected group names, and corresponding e-mails. For example, Rash Diva's pharmacist was Dr. Benny Dryl. Humor and puns were often used to engage students' interest and increase participation.
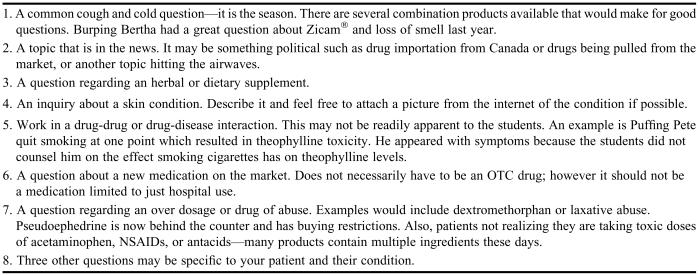
Throughout the semester, the virtual patients e-mailed in-depth questions primarily focusing on self-care topics on a weekly basis and responded to the student's reply. Each group had to submit all correspondence to the instructor each Friday. Virtual patients asked the students a series of questions based on the individual patient profile. Virtual patients were advised to base their questions on a list of provided standard question topics, thereby creating a thread of common questioning throughout the semester. Instructions for virtual patients to develop questions from standardized topics are provided in Table 1. Since each patient had a different profile, the questions varied, but it ensured that pertinent nonprescription topics were covered. The virtual patients were given the flexibility to develop their own way of asking the suggested questions and were encouraged to include 3 elective questions specific to their patient profile.
Table 1.
Sample Guidelines for Developing Standardized Questions Given to Volunteers Serving as Virtual Patients for Pharmacy Students Enrolled in an Advanced Self-care Elective
On the first day of class, patient counseling and interviewing techniques taught in the Self Care 1 course were reviewed and student groups were formed. Each student group was randomly assigned a patient profile. The profile was designed to provide the students with the background information a pharmacist might have about the patient and his/her medications.
After receiving their profiles, a Powerpoint presentation was delivered to introduce the concept of virtual patients as described earlier, provide e-mailing instructions, and review grading procedures. Both virtual patients and students were expected to send a minimum of 2 e-mails each week to ensure appropriate patient assessment. They were also instructed to respond below the previous e-mail; therefore, dialogues could be read down the page and were easier to follow. After the presentation, students were given time to work on a sample case (ie, “Wheezing Wilma” would like to use Echinacea for her cold), encouraged to ask questions, and then reviewed the correspondence with the course instructor. Written materials were also incorporated within course packets and included an activity description, a grading form, a question calendar, and group ground rules.
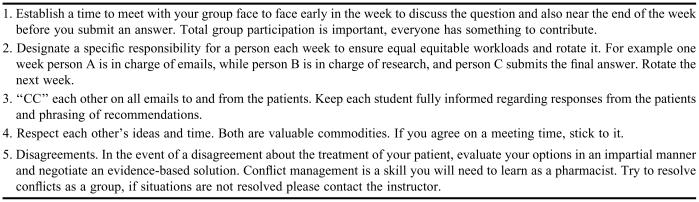
During the first 3 years that the elective was offered, students self-selected their group members; in the fourth-professional year, group members were randomly assigned. Guidelines regarding group work were established during the second-professional year to facilitate participation when answering patient questions. Groups were encouraged to have a regular schedule for meeting and rotating responsibilities from week to week. The group guidelines are listed in Table 2.
Table 2.
Group Guidelines for Interacting With Virtual Patients Given to Pharmacy Students Enrolled in an Advanced Self-care Elective
Outcome Measures
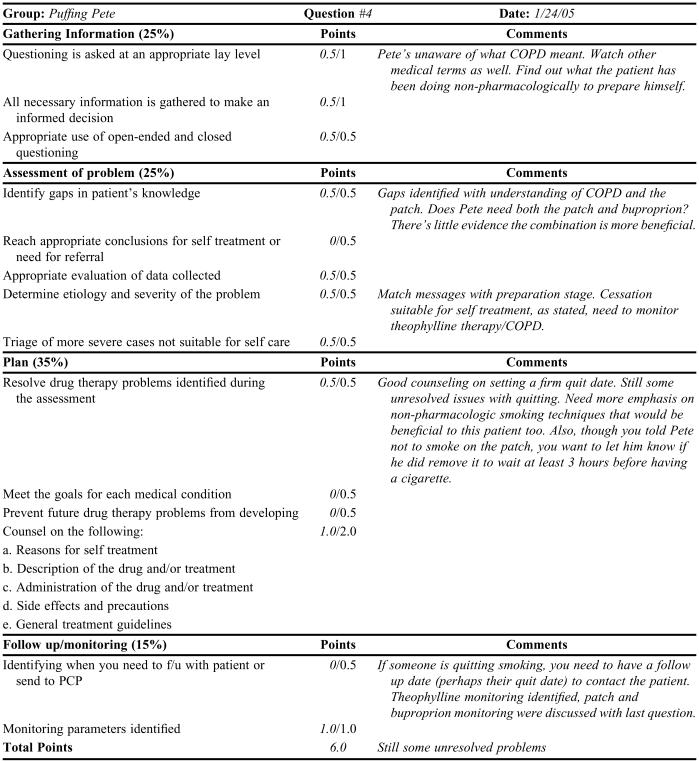
Once a response was completed for the week, the students or virtual patient forwarded the interaction to the course coordinator for grading. Each question was assessed on a 10-point scale to equal 100 points when the semester ends. Appendix 2 illustrates an example of the grading process for an individual question. Since each patient and question varied significantly, it was important to develop a broad grading tool for the self-care consultation. All questions were graded by the course coordinator to ensure consistency in the grading process. Occasionally, the course coordinator discovered an interesting topic that should be presented to the rest of the class or a student or group identified a situation they wished to present to the class, so the topic was discussed within the classroom setting. Since the dialogue between the virtual patients and the students occurred in an electronic format, it could be presented chronologically using an LCD projector.
In spring 2005 and 2006, on the first day of class, students were asked to complete a self-evaluation of their self-care skills on a scale from 1-10 on which 1 = strongly disagree and 10 = strongly agree. The same self-evaluation was administered and collected on the last day of class. To identify any significance difference between individuals at baseline and upon course completion, a paired t test was preformed using the Statistical Package for Social Sciences, v. 9.0 for Windows. The survey instrument was approved by the University of Rhode Island Institutional Review Board.
A survey instrument evaluating students' perceptions of the virtual patient interactions was also given at the end of the semester. Students were also asked to rate the following experiences on a scale from 1-5 on which 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree. The instrument also collected basic demographic data and space was included for students to provide constructive comments. This survey was also approved by the University of Rhode Island Institutional Review Board and administered in 2003, 2005, and 2006.
Finally, students were asked to evaluate other group members' participation in interacting with virtual patients at midterm and upon course completion. The purpose of this assessment was to assure that all group members had contributed to the care of the group's virtual patient. On a scale from 1-10, on which 1 indicated “never” and 10 indicated “always,” students anonymously ranked their group members on attending scheduled meetings, contributions to solving patient problems, and playing a direct role in patient correspondence. A section was also included for self-assessment of group participation.
ASSESSMENT
The number of e-mails exchanged between the students and virtual patients varied from week to week, ranging from a minimum of 2 responses to a maximum of 8. If the students answered the question without questioning the problem (ie, just provided one response), it was evident that the student did not fully assess the problem and therefore lost points. Feedback on weekly questions was given within 1-2 weeks after submission. Students received detailed information on the positive aspects of their discussion and areas for improvement for future questions. Weekly grading for the activity took the course coordinator 1-3 hours to complete.
Although students enrolled in Self Care 2 had already completed the required Self Care I course, grades tended to be lower earlier in the semester as students often omitted major assessment questions and failed to provide follow-up advice within the first 3 weeks. For example, in 2006, the first week of grades averaged 80%, midpoint grades averaged 86%, and grades for the final week of the course averaged 92%. Students demonstrated improvement and growth in their assessment and responses as the semester progressed. The majority of responses included a complete and appropriate treatment plan for the patient as a result of collecting all the necessary information through patient questioning. Students achieved the course objectives of patient assessment and formulating treatment plans through their correspondence. From 2003-2006, final grades on the virtual patient activity ranged from 65%-98%, with an average grade of 88%. Appendices 1 and 2 provide an example of a group's correspondence and subsequent assessment that occurred early in the semester.
Written communication skills also improved over the semester. Within the assessment forms, students were graded on gathering all pertinent patient information, use of open- and closed-ended questions, providing clear nonprescription and non-pharmacological education, and communicating with the patient at a lay level.
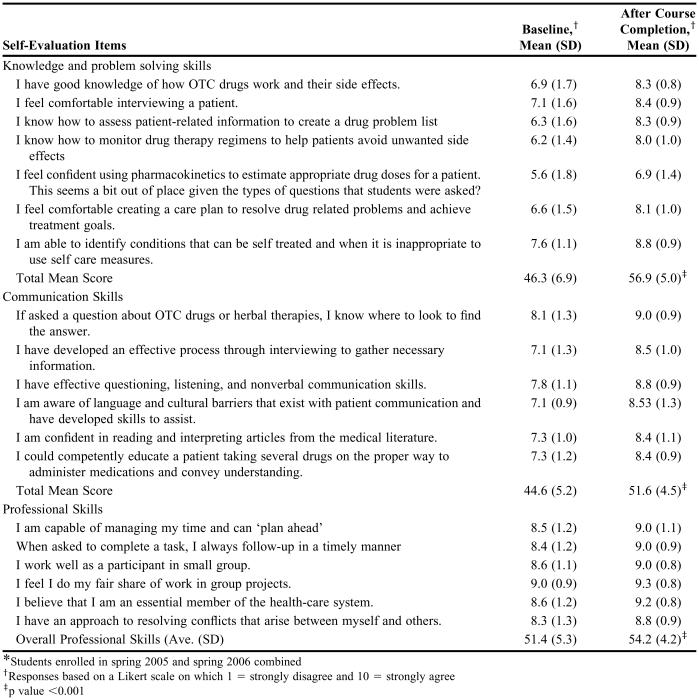
Self-Evaluation
Eighty-one students participated in the self-evaluation of skills at baseline and upon course completion. Students felt significantly more confident in their self-care competencies at the end of the semester than at the beginning. A composite of overall knowledge and problem solving, communication, and professional skills is presented in Table 3. Compared to baseline, students' self-assessment of skills upon completion of the course significantly improved in all categories (p < 0.001). Students perceived that they had achieved the stated objectives for the course.
Table 3.
Self-evaluation Data of Pharmacy Students Enrolled in an Advanced Self-care Elective (N = 81*)
*Students enrolled in spring 2005 and spring 2006 combined
†Responses based on a Likert scale on which 1 = strongly disagree and 10 = strongly agree
‡p value <0.001
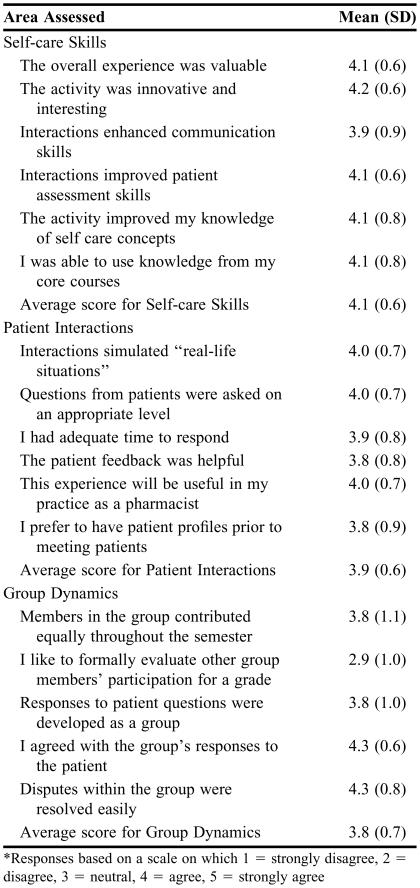
Activity Evaluation
The majority of the students who completed the elective were women (71%). Seventy-two percent of the students stated they had previous professional experience in a community setting and 65% envisioned being involved in community pharmacy practice within 5 years.
The results of the survey questions evaluating the activity are listed in Table 4. The students agreed that the overall experience was valuable and improved their current self-care skills. Student feedback also demonstrated this activity was practical because it reflected situations that commonly occur in a community pharmacy setting. They appreciated the opportunity to communicate with virtual patients in this monitored setting prior to starting their advanced pharmacy practice experiences.
Table 4.
Pharmacy Students' Assessment of a Virtual Patient Activity (N = 132)
*Responses based on a scale on which 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree
Survey comments indicated students' awareness of the level of language they use with patients, and that they realized many of their words would not be recognized by the general population.
Students were also asked if they would have preferred taking another examination than work with the virtual patients, to which 12 of 132 students (9%) responded “yes.”
Peer Evaluation
Most students ranked their peers' performance in the 8-10 range at the course midpoint and upon activity completion. The performance ratings of a few students who did not fully participate in the group activities ranged from 2-5 in some categories.
DISCUSSION
Since the Self Care 2 course was developed, the virtual patient activity has been incorporated with the intent that students will be able to build upon knowledge from the prior Self Care 1 course. A role-playing patient participating in a class case presentation will not react in the same manner as a real patient encountered in a pharmacy. Neither will he/she display the consequences of appropriate or incorrect advice days later, nor develop additional patient problems as a real patient might. For these reasons, the virtual patient activity provides the best approach to meeting the course objectives. Through correspondence with virtual patients, students were able to gain more in-depth knowledge of nonprescription products and appropriately triage problems while also developing effective communication skills. An array of topics have been covered, from common ailments such as cough and cold, skin conditions, and analgesic use to more nontraditional therapies such as homeopathy or herbal remedies.
Initially students struggle with gathering information using open- and closed-ended questions early, but become proficient in this skill as the semester progresses. Almost all groups have used medical terminology that a patient would not recognize at least once in the semester but avoid this in subsequent correspondence. This is another key element in developing communication skills for effectively transferring information on an appropriate level and recognizing that people may misinterpret what the pharmacist or another health care provider has conveyed to them. In addition, there have been a number of students, and there will continue to be more students, who do not use English as their first language. Again, this provides a format for practicing communication skills in terms of grammar and comprehension.
The activity was successful due to the volunteers' effective portrayal of the virtual patients. Each semester, 8-12 pharmacists devote time and effort to helping these students learn appropriate assessment and counseling skills. It is also an excellent opportunity to include preceptors from the community who desire to become more involved with teaching but who have limited time. It allows any interested pharmacist to participate. Having committed volunteers, organization, and access to the Internet have contributed to the success of the virtual patient program.
Several lessons have been learned during the 4 years since this activity was implemented, and each year steps are taken to improve the quality of the virtual patients. Student feedback from surveys has been useful in determining these changes. Some of the modifications made in response to students' requests include implementation of ground rules to promote equal participation, timely feedback for improvement, and incorporating patient profiles as a baseline of information for students to have. A change made independently of student feedback was providing a list of standardized question topics. For example “Puffing Pete's” group had a large amount of smoking cessation questions the first year with little time for other self-care topics. Creating the standardized questions allowed patients to work on other topics, but still tailor them to the specific patient. Another difficult patient for student's to interact with was “Harry Leukoplakia”, who had tested positive for the human immunodeficiency virus (HIV+). Due to his HIV+ status, students were very wary of making self-care recommendations even in situations where it would be appropriate to self-treat, and in almost all interactions referred the patient to his physician rather than offering self-care advice. Due to the limited amount of self-care recommendations that could be made, this patient persona was not included the following year.
To address the situations where not all students equally participated according to group evaluations, those individuals made appointments with the course coordinator to discuss the group dynamics and role in patient consultations. In most cases, bringing the lack of participation to their attention resulted in more active contributions for the second half of the semester. If students still failed to contribute, new groups have been formed consisting of all those not regularly participating in group activities with a new patient. The new group seemed to work better for these individuals, creating a situation where all needed to take a more active role.
Some limitations of the applicability of the findings are apparent. Students were not focusing on verbal communication skills when working with the virtual patients. Also, they were unable to interpret the patient's nonverbal communication such as facial expressions, tone of voice, demeanor, and appearance. Though these skills were not addressed with virtual patients, they were adequately covered in the classroom setting in Self Care 2 and in other courses such as the Pharmacy Practice Laboratory. An additional limitation of our study was the lack of formal assessment of actual virtual patients on their satisfaction and perception of student learning. This information would be useful in making future modifications to the virtual patient program.
As discussed earlier, grading time for the group interactions varied from 1-3 hours per week, depending on the class size; thus, this activity would work best in smaller elective classes. However, it could be adjusted by assigning fewer questions or involving pharmacy residents in the grading process if there were a larger class size. The activity is also not limited to self-care concepts, since prescription medication questions encountered in practice are sometimes intertwined with inquiries about nonprescription medications.
This activity is easily transferable to other colleges or schools of pharmacy. Developing the patient profiles and organizing virtual patients and students take a significant amount of dedication and time to set up. Since presenting this learning activity at the American Pharmacists Association 4th Annual Self Care Institute in Boston, other schools have implemented and modified virtual patient use in their courses.
CONCLUSION
The integration of virtual patients in the Self Care 2 course promoted active-learning outside the classroom. There was clear application to community pharmacy practice by preparing students for future practice situations. This activity incorporated writing skills and group work as well as ongoing interaction with patients over several weeks. Students also learned about building pharmacist-patient relationships, resulting in a number of student groups developing personal relationships with their virtual patients each semester.
ACKNOWLEDGEMENTS
I would like to thank Anne Hume, PharmD, FCCP, BCPS, and Brett Feret, PharmD, for their assistance in developing the virtual patients and preparation of this manuscript; Brian Quilliam, PhD for his statistical expertise; and all the current and past virtual patients who have made this learning activity possible. I would also like to thank Karen Bastianelli, PharmD, from the University of Minnesota in Duluth, and Jennifer Smith, PharmD, CDE, from Campbell University, for sharing their experiences after adapting the virtual patient activity in their own courses.
Appendix 1. Sample interaction with a virtual patient
PUFFING PETE: Dr. Nick O'Tine, I decided to use the patch to quit smoking. I saw my doctor on Friday and he told me just to stop taking the Slo-Bid® stuff- I am happy about that! That Zyban® was just too expensive though- I'm not made out of money. Now when do I start using the patch? Should I just put it on now and quit? I am a little nervous about that. What if I really need a cigarette? Can I just peel it off and then stick it back on? I think I should cut down first- what do you think? Pete.
STUDENTS: Dear Mr. Puffing, Previously, we had stated you set a firm quit date that is free of what compels you to smoke. We recommend you plan on this date and not just quit tomorrow. We still firmly believe you should use generic not brand Zyban®. Smoking 1.5 packs a day costs about $200 a month. Generic Zyban® will cost roughly half the price and increases your chances of quitting considerably. If you have prescription coverage the savings will be even greater. We recommend you start generic Zyban® now and set a firm quit date 2 weeks in the future or so free of stress. For example, we wouldn't want you to quit smoking during the Superbowl especially if the patriots loose. Now the patch- on the date you choose to quit smoking, put the patch on in the morning. You CANNOT smoke while on the patch. You CANNOT take the patch off and smoke then replace the patch. If you still have our previous email we explained the exact taper and strengths. If you don't remember just let us know and we will explain again. You have a right to be nervous about quitting smoking. It is a tough task. Many people try and many fail. Since you have quit in the past, studies show your chances of quitting increase with each new attempt. We will be here to help you through it. We believe a firm quit date, generic Zyban®, the patch, and our support is the best recipe to help you quit successfully. Problems may arise and we will help you through it. Now the Slo-bid® - did your doctor tell you to taper? Is he going to monitor your COPD to see if the Combivent® is adequate? Please email with any additional questions or concerns. We look forward to hearing from you. Sincerly, Nick O'Tine.
PUFFING PETE: Dr. Nick O'Tine, I don't think I can use the patch then, what if I really need a cigarette?! I thought I could just peel it off in an emergency situation. Maybe I will just take the generic Zyban® then since I can smoke while I am taking it. How much do I take? So I will get that, start tomorrow and quit in 2 weeks.
What is COPD? I don't know if he is going to monitor me for that. Can you monitor it for me? My doctor said he didn't think the Slo-Bid® was really doing much for me and that I should just use my inhaler everyday. Do you think I should taper the Slo-Bid®? Thanks, Pete.
STUDENTS: Dear Peter, We need to find out how serious you are about quitting. If you are serious about quitting and have the will, you should never NEED a cigarette. You mentioned not using the patch just because you think you'll want a cigarrette. Of course you will! You've been smoking for 20 years. Medications will help you quit but YOU are the one that says yes or no to the desire. We cannot provide a medication that magically makes you quit. We can give medications and advice for ones that have proven to be most effective. We still believe you need to set a firm quit date. You need to start thinking about how quitting will help improve your life (more energy to walk and for your live-in girlfriend). Think about how walking up stairs used to be, how easy it was. You also need to tell people around you to support you. Don't go around places or people that smoke. We believe you should start Zyban® 150mg for 3 days then increase to 150mg twice daily for now, and set a quit date 2 weeks or 1 month in the future in which you should use the patch. In the meantime you should make a list of how quitting will benefit you. You should make a list of how you will deal with difficult situations. In 2 weeks to a month, when you quit, we still believe a nicotine patch will help you. You will be well prepared and ready to deal with situations you feel as if you “need” a cigarette. COPD is the umbrella term for your chronic bronchitis. It is the reason you've been placed on Combivent®, guafenesin, and Slo-bid®. These help manage your symptoms. We know the doctor told you he doesn't feel as if the Slo-bid® is working for you, but do you feel as if it has helped you? How was your breathing before being placed on Slo-bid® compared to now (after recieving Slo-bid®)? COPD progression is typically monitored by your physcian with regular pulmonary function tests. There is no published recommended taper for Slo-bid® but we first want to know if YOU felt it worked. Have a nice day.
Appendix 2. Example question grading form: Puffing Pete
REFERENCES
- 1. Consumer Health Products Association. OTC Facts and Figures. Available at: http://www.chpa-info.org/ChpaPortal/PressRoom/Statistics/OTCFactsandFigures.htm. Accessed on August 8, 2006.
- 2.Monaghan MS, Gardner SF, Hastings JK, Reinhardt GL, Knoll R, Vanderbush RE, et al. Student attitudes toward the use of standardized patients in a communication course. Am J Pharm Educ. 1997;61:131–7. [Google Scholar]
- 3.Glasser D, Ahrens R, Caffee A, Johnson M. Standardized patient assessment in a disease state management model. Am J Pharm Educ. 2002;66:72–8. [Google Scholar]
- 4.Holiday-Goodman M, Lively BT, Nemire R, Mullin J. Development of a teaching module on written and verbal communication skills. Am J Pharm Educ. 1994;58:257–61. [Google Scholar]
- 5.Sibbald D. Bridging the gap from the classroom to practice: PBL students develop consumer website for nonprescription drugs. Am J Pharm Educ. 2000;61:339–48. [Google Scholar]
- 6.Parish SJ, Weber CM, Steiner-Grossman P, Milan FB, Burton WB, Marantz PR. Teaching clinical skills through videotape review: a randomized trial of group versus individual reviews. Teach Learn Med. 2006;18(2):92–8. doi: 10.1207/s15328015tlm1802_1. [DOI] [PubMed] [Google Scholar]
- 7.Hulsman RL, Mollema ED, Oort FJ, Hoos AM, de Haes JC. Using standardized video cases for assessment of medical communication skills: reliability of an objective structured video examination by computer. Patient Educ Couns. 2004;60(1):24–31. doi: 10.1016/j.pec.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Bearman M, Cesnik B, Liddell M. Random comparison of ‘virtual patient’ models in the context of teaching clinical communication skills. Med Educ. 2001;35:824–32. doi: 10.1046/j.1365-2923.2001.00999.x. [DOI] [PubMed] [Google Scholar]
- 9.Stevens A, Hernandez J, Johnsen K, Dickerson R, Raij A, Harrison C, et al. The use of virtual patients to teach medical students history taking and communication skills. Am J Surg. 2006;191:806–11. doi: 10.1016/j.amjsurg.2006.03.002. [DOI] [PubMed] [Google Scholar]