Abstract
Aim
To determine the temporal retinal vessel angle in babies and its relation to preterm birth.
Methods
Digital images were obtained during routine screening for retinopathy of prematurity (ROP). The temporal retinal vessel angle was measured in 164 eyes of 82 babies born “very preterm” (24–27 weeks gestational age (GA)), “preterm” (28–31 weeks GA), and “near term” (⩾32 weeks GA).
Results
Mean temporal vessel angle (TVA) for all three GA groups together is 80.0° (SD 17.0°) for the right eye and 80.5° (16.7°) for the left eye. The range is right eye 59–106°, left eye 69–97°, with 95% data above 67° for the right and 63° for the left eye. For babies born near term, TVA is 82° in each eye. There is a high degree of interocular symmetry between right and left eyes and a statistically insignificant trend for increasing TVA with increasing GA. The presence and stage of ROP affected one parameter of the left eye alone.
Conclusions
These data provide normative data on the TVA in babies and will facilitate, especially if there is interocular asymmetry, determining whether there is macular displacement.
Keywords: prematurity, retinal vessels, retinopathy of prematurity
The angle between the major temporal retinal vessels as they leave the optic disc and course their way towards the periphery has long been used as a component in the evaluation of the structural and functional integrity of the macular region. Narrowing of this vessel angle is used clinically as an indication of compromised macular function, because of retinal dragging and macular ectopia, and can be seen as sequelae of retinopathy of prematurity (ROP), in association with the inherited vitreoretinopathies and other conditions.
Narrowing of the angle between the major temporal retinal vessels featured in the classification of retrolental fibroplasia of Reese et al1 and in the Classification of Retinal Detachment, the International Classification of Retinopathy of Prematurity.2 More recently the angle has been a component in the evaluation of structural outcome following ROP, by photographic grading,3 and as an ophthalmoscopic outcome variable at 10 years after cryotherapy.4
Despite recognition of the clinical importance of the abnormal, in clinical practice and research, the normal values of the angle between the major temporal retinal vessels have never been defined, nor has the degree of symmetry between the two eyes been determined. In effect, the judgment of whether macular ectopia is present or not is subjective. The purpose of this study therefore was to determine the angle between the superior and inferior temporal vessels, using digital imaging, in the perinatal period in babies born preterm or near full term. For the purpose of simplicity, only retinal veins were measured.
Methods
Digital retinal images were obtained using a RetCam 120 (Massie Labs, Dublin, CA, USA) during routine ROP screening at St Mary's Hospital, London. Images contained no patient identifiable information of any nature at any time and the study was carried in accord with the tenets of the Declaration of Helsinki. Each baby was categorised by gestational age (GA) into three groups comprising: “very preterm” (24–27 weeks GA), “preterm” (28–31 weeks GA), and “near term” (⩾32 weeks GA). The images (640×480 pixels, 24 bit, RGB bitmap) of left and right eyes were obtained, on one occasion only, for babies of all gestational ages between 36 weeks and 44 weeks postmenstrual age (PMA). This permitted comparison of vessel characteristics of babies born at difference GAs at the same period of development. Images were analysed using Paintshop Pro 7.0 (www.jasc.com). ROP was categorised according to the International Classification of ROP.5
The two identifiable points on the retina upon which a consistent reference frame may be based are the optic disc centre and the fovea. Drawing an axis perpendicular to that defined by the fovea and optic disc centre pinpoints the two points at which the vertical axis intersects the superior and inferior temporal veins. The total vessel angle (TVA) was calculated between the optic disc centre and these two intersections. This was subdivided into the superior and inferior vessel angle (SVA and IVA respectively—see fig 1).
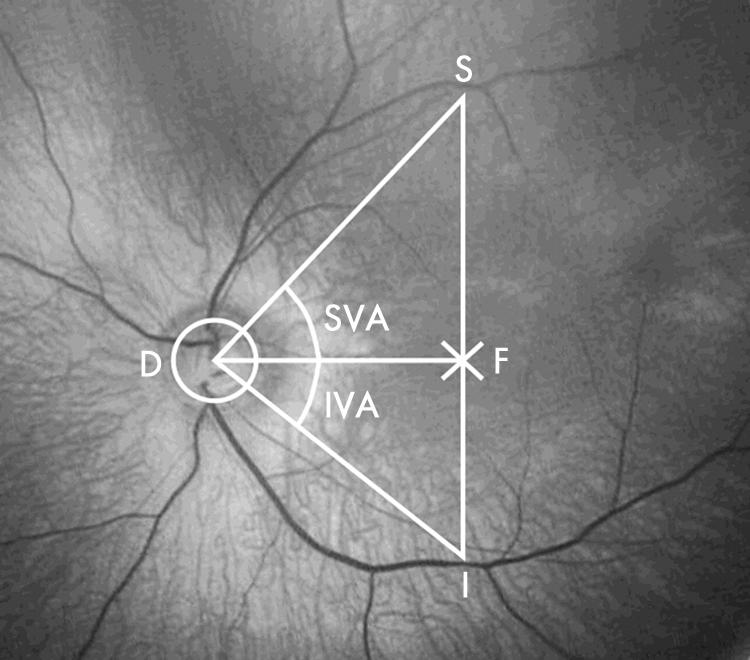
Figure 1 Optic disc (D) and fovea (F) were identified by two independent observers. Horizontal line drawn between disc centre and fovea, and the perpendicular to this (I‐F‐S) was constructed to reach the inferior and superior temporal veins. Lines from points I and S to the optic disc centre enabled angles SVA (superior vessel angle) and IVA (inferior vessel angle) subtended at the optic disc to be calculated.
The macula is not well defined in the neonatal eye and was identified, in order of maturity: central position within the temporal vascular arcades, annular macular ring reflex, and the pit of the fovea centralis.6 The optic disc centre and the position of the fovea were determined by two independent observers. Pixel values of the x and y coordinates for these points were recorded. The image was then rotated to align disc and fovea along the horizontal meridian. A vertical line perpendicular to the horizontal meridian was drawn through the fovea to the inferior and superior temporal vascular arcades. The coordinates of the points of intersection were then measured. The distance from the inferior and superior vessels to fovea was then measured. The emergent angle was then calculated using the inverse tan law. Angles were expressed in degrees as the mean (SD) and range. The difference in the angle between the two eyes was expressed as the mean difference between left and right eye angle plus or minus 95% confidence interval with the intraclass correlation coefficient. Tests used to compare between gestational age groups were one way ANOVA or ANOVA on ranks. For comparison of vessel angles between ROP stage groups the tests used were one way ANOVA or Kruskal‐Wallis where equal variance test failed. Where significant differences were detected a post hoc Tukey test was applied.
Results
One image of 164 right and left eyes of 82 babies taken at 36–44 weeks PMA (very preterm, n = 26; preterm, n = 27; near term, n = 29) were analysed. The results for individual groups are presented in table 1 and the mean TVA for all GA groups taken together was 80.0° (SD 17.0°) right eye and 80.5° (16.7°) left eye with 95% data above 67° for the right and 63° for the left eye. With one exception there was no significant difference between SVA, IVA, or TVA for the three GA groups (one way ANOVA, see table 1), either considering the groups individually or analysing groups I and II versus group III. The exception was between left eye SVA and IVA for when GA groups were considered together (p = 0.048). There was a high degree of interocular symmetry for mean TVA, SVA, and IVA (paired t test, p>0.05). The mean difference between the angle in the left and right eye is shown in table 1 as the 95% confidence interval and intraclass correlation coefficient. While a trend of increasing TVA with increasing GA was observed, this did not reach statistical significance.
Table 1 Vessel angle (in degrees) according to gestational age (GA) groups expressed as mean (SD) and range in parenthesis.
| Eye | SVA | IVA | TVA | |
|---|---|---|---|---|
| Group 1, very preterm 24–27 weeks GA | Right (n = 26) | 38.1 (11.8) (28.0–49.0) | 39.2 (7.9) (31.0–48.9) | 77.3 (16.1) (65.3–96.1) |
| Left (n = 26) | 40.8 (11.4) (27.7–51.7) | 38.3 (10.8) (25.9–46.3) | 79.1 (16.1) (54.6–95.2) | |
| Left‐right | 2.8 (15.1) (0.1) | –0.9 (9.6) (0.5) | 1.8 (15.4) (0.5) | |
| Group II, preterm 28–31 weeks GA | Right (n = 27) | 41.0 (11.8) (30.4–51.7) | 39.5 (9.7) (27.3–47.5) | 80.5 (14.9) (65.2–99.2) |
| Left (n = 27) | 40.7 (10.9) (27.9–53.3) | 39.7 (11.7) (27.1–50.1) | 80.4 (19.7) (66.1–98.4) | |
| Left‐right | −0.3 (15.5) (0.1) | 0.2 (13.7) (0.2) | −0.1 (24.1) (0.1) | |
| Group III, near term ⩾32 weeks GA | Right (n = 29) | 40.8 (11.9) (26.7–53.8) | 41.1 (11.4) (26.2–51.8) | 81.9 (18.9) (58.5–105.6) |
| Left (n = 29) | 41.2 (10.2) (31.7–54.0) | 40.5 (6.8) (30.2–47.5) | 81.7 (14.0) (68.8–96.7) | |
| Left‐ right | 0.4 (16.4) (−0.1) | −0.6 (11.1) (0.3) | −0.1 (21.4) (0.2) | |
| Groups I, II, and III all groups 24 weeks GA to near term | Right (n = 82) | 40.0 (12.0) (26.7–54.0) | 40.0 (9.8) (26.2–51.8) | 80.0 (17.0) (58.5–105.6) |
| Left (n = 82) | 40.9 (10.7) (27.7–54.0) | 39.5 (9.9) (25.9–50.1) | 80.5 (16.7) (54.6–98.4) | |
| Left‐right | 0.9 (15.7) (0.0) | −0.4 (11.5) (0.3) | 0.5 (20.5) (0.3) |
Left‐right, denotes the mean difference between left and right eye angle ±95% confidence interval with the intraclass correlation coefficient in parenthesis. SVA, IVA, and TVA are respectively: superior, inferior, and total temporal retinal vessel angles. See text for other details.
Acute phase ROP stage was symmetrical in 79 of 82 babies, two babies had stage 1 left eye and stage 0 right eye. One baby had stage 1 right eye and stage 0 left eye. Of the 14 babies with stage 3 this reached threshold in 10 and these babies were treated. A significant level of vessel angle acuteness was associated between stages 0 and 1, 1 and 2, and 1 and 3 ROP in left IVA (table 2).
Table 2 Comparison of vessel angles between ROP stage groups: angles expressed in degrees as mean (SD).
| Right eye: | ||||
|---|---|---|---|---|
| ROP stage | No | SVA | IVA | TVA |
| 0 | 43 | 41.3 (6.2) | 40.5 (5.8) | 81.8 (9.4) |
| 1 | 14 | 40.6 (4.9) | 40.7 (4.1) | 81.3 (5.5) |
| 2 | 11 | 38.2 (5.7) | 38.5 (2.4) | 76.7 (6.1) |
| 3 | 14 | 36.9 (6.4) | 38.8 (4.5) | 75.7 (9.3) |
| Left eye: | ||||
|---|---|---|---|---|
| ROP stage | No | SVA | IVA | TVA |
| 0 | 42 | 40.3 (5.4) | 39.5 (4.5) | 79.7 (8.3) |
| 1 | 15 | 42.7 (5.3) | 43.4 (4.8) | 86.1 (7.0) |
| 2 | 11 | 40.5 (4.2) | 37.2 (3.5) | 77.7 (6.3) |
| 3 | 14 | 41.3 (6.7) | 37.5 (6.1) | 78.8 (10.2) |
| 0 v 1: p = 0.038 | ||||
| 1 v 2: p = 0.009 | ||||
| 1 v 3: p = 0.008 | ||||
Only IVA of the population of left eyes showed significant differences between ROP stages.
Discussion
The results of this study show that for babies born near full term the mean temporal vessel angle (TVA) ranges from 59° to 106°. These results provide normative data on the temporal retinal vessel angle in babies. There is a high degree of interocular symmetry, the mean TVA being 82° for both right and left eyes and indicate that interocular angle asymmetry above about 14–20° (95% confidence intervals) should be regarded with suspicion. The normal angle range is large (right 59–106°, left 69–97°), thus, determining whether symmetrical angles are abnormal, or not, can be problematic, unless they fall outside the 95% confidence intervals—that is, below 67° for the right and 63° for the left eye,
In our opinion there are no major technical factors that might have influenced validity of the measurements in this study. Decentration was minimised by using images with the optic disc located in the centre. Ametropia only affects magnification if exceeding 3 dioptres7 and as measurements were taken over a short postmenstrual age range the variation is unlikely to be great.
Blood is delivered to tissues by a vascular system that is geometrically designed in accord with the principles of maintaining steady state and minimum work—Murray's law.8 According to this principle, the total flow of any vascular system is carried by a set of vessels whose radii cubed sum a constant value.9 The fractal geometric dimensions seen in normal retinas are disturbed in disease.10 Retinal vessel bifurcation angles may reflect microvascular density11 and if this is low a narrower angle results, as has been reported in men who were born with low birth weights. It is likely that the TVA obeys Murray's law, and that this increases with time in utero probably reflecting increased retinal metabolic activity. Further work is required to determine the possible influences of gestational age and acute phase ROP on vessel angle development. While the fovea is inferiorly displaced with respect to the optic nerve head in the preterm eye as in the normal adult eye,12,13 we did not detect a significant asymmetry with respect to the distance of the superior and inferior veins from the fovea.
As mentioned in the introduction, for over 50 years the angle between the major temporal vessels has been used as a pointer to the structural integrity of the posterior pole of the retina. Abnormalities can be associated with a number of retinal conditions—notably the sequelae of ROP. To date, all assessments of narrowing of the temporal vessel angle and macular ectopia have been qualitative, and clinicians have been required to make the binary normal/abnormal judgment. Photographic grading in the CRYO‐ROP Study3 included assessment of vessel traction, which by locating the superior and inferior temporal vessels within 30° sectors was, in effect, an evaluation of the temporal vessel angle, but this study did not define the normal range. Interocular symmetry is a feature of acute phase ROP but not necessarily the later stages14,15; therefore, our finding that, in the absence of pathology, the temporal vessel angle is symmetrical facilitates differentiating the normal from the abnormal, particularly when the abnormality is relatively subtle.
Currently, the correlation of function from the posterior pole sequelae of ROP is unpredictable,16 especially if these sequelae are relatively mild.17 Hopefully, the results from babies presented here will contribute data to what constitutes a normal temporal retinal vessel angle in the infant eye, the underlying physiological factors that determine its magnitude, and how it is affected when the fetal period is shortened by premature birth. It will also help clinicians develop a more robust quantifiable and graded assessment of the posterior pole of the retina. Whether this facilitates the accurate prediction of function from the structural appearance can only be determined by future studies.
Abbreviations
GA - gestational age
IVA - inferior vessel angle
PMA - postmenstrual age
SVA - superior vessel angle
TVA - temporal vessel angle
References
- 1.Reese A B, King M J, Owens W C. A classification of retrolental fibroplasia. Am J Ophthalmol 1953361333–1335. [PubMed] [Google Scholar]
- 2.The International Committee for the Classification of the Late Stages of Retinopathy of Prematurity An international classification of retinopathy of prematurity. II. The classification of retinal detachment. Arch Ophthalmol 1987105906–912. [PubMed] [Google Scholar]
- 3.Watzke R C, Robertson J E, Palmer E A.et al Photographic grading in the retinopathy of prematurity cryotherapy trial. Arch Ophthalmol 1990108950–955. [DOI] [PubMed] [Google Scholar]
- 4.Cryotherapy for Retinopathy of Prematurity Cooperative Group Multicentre trial of cryotherapy for retinopathy of prematurity: ophthalmological outcomes at 10 years. Arch Ophthalmol 20011191110–1118. [DOI] [PubMed] [Google Scholar]
- 5.An International Committee for the Classification of Retinopathy of Prematurity The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 2005123991–999. [DOI] [PubMed] [Google Scholar]
- 6.Isenberg S J. Macular development in the premature infant. Am J Ophthalmol 198610174–80. [DOI] [PubMed] [Google Scholar]
- 7.Pach J, Pennell D O, Romana P E. Optic disc photogrammetry: magnification factors for eye position, centration, and ametropias, refractive and axial; and their application in the diagnosis of optic nerve hypoplasia. Ann Ophthalmol 198921454–462. [PubMed] [Google Scholar]
- 8.Murray C D. The physiological principle of minimum work applied to the angle of branching of arteries. Proc Natl Acad Sci 192612835–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherman T F. On connecting large vessels to small. J Gen Physiol 198178431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daxer A. The fractal geometry of proliferative diabetic retinopathy: implications for the diagnosis and the process of retinal vasculogenesis. Curr Eye Res 1993121103–1109. [DOI] [PubMed] [Google Scholar]
- 11.Chapman N, Mohamudally A, Cerutti A.et al Retinal vascular network architecture in low birth weight men. J Hypertens 1997151449–1453. [DOI] [PubMed] [Google Scholar]
- 12.Williams T D, Wilkinson J M. Position of the fovea centralis with respect to the optic nerve. Optom Vis Sci 199269369–377. [DOI] [PubMed] [Google Scholar]
- 13.Bixenman W W, von Noorden G K. Apparent foveal displacement in normal subjects and in cyclotropia. Ophthalmology 19828958–62. [DOI] [PubMed] [Google Scholar]
- 14.Fielder A R, Shaw D E, Robinson J.et al Natural history of retinopathy of prematurity: a prospective study. Eye 19926233–242. [DOI] [PubMed] [Google Scholar]
- 15.Quinn G E, Dobson V, Repka M X, The Cryotherapy for Retinopathy of Prematurity Cooperative Group et al Correlation of retinopathy of prematurity in fellow eyes in the cryotherapy for retinopathy of prematurity study. Arch Ophthalmol 1995113469–473. [DOI] [PubMed] [Google Scholar]
- 16.Gilbert W S, Dobson V, Quinn G E.et al The Cryotherapy for Retinopathy of Prematurity Cooperative Group. The correlation of visual function with posterior retinal structure in severe retinopathy of prematurity. Arch Ophthalmol 1992110625–631. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds J, Dobson V, Quinn G E.et al The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Prediction of visual function in eyes with mild to moderate posterior pole residua of retinopathy of prematurity. Arch Ophthalmol 19931111050–1056. [DOI] [PubMed] [Google Scholar]


