Abstract
A 50‐year‐old man with alcoholic liver disease presented with fever, tenosynovitis, polyarthritis and a vasculitic rash on the hands and feet for 4 days. He had neutrophilia and raised inflammatory markers. He had no history of sore throat, urethral discharge or travel abroad. His initial blood cultures were negative, and he was treated for vasculitis with steroids. The rash and arthritis seemed to improve initially, but he had another episode of fever. Repeat blood cultures grew Neisseria gonorrhoeae,and he received intravenous ceftriaxone followed by oral ciprofloxacin. He had marked improvement in rash, tenosynovitis and arthritis, and the fever dropped. He also had chlamydial urethritis and received azithromycin. The presentation of disseminated gonococcal infection after a presumptive episode of asymptomatic urethral gonorrhoea is highlighted.
A 50‐year‐old car mechanic was admitted with a 4‐day history of fever (39.4°C) with chills and swollen, tender, stiff hands and feet. He also had red spots on the hands and feet. There was no history of sore throat, urethral discharge, red eye or tick bite. He had alcoholic liver disease but continued to drink >60 units of alcohol weekly. He had had attacks of gout in the first metatarsophalangeal joints and osteoarthritis of the right knee in the past.
On examination, he had asymmetrical arthritis involving the wrists, ankles, and metacarpophalangeal, proximal interphalangeal and metatarsophalangeal joints. There was tenosynovitis on the dorsal aspect of the wrists and ankles. There was an erythematous maculopapular non‐pruritic vasculitic rash on the upper and lower extremities.
Laboratory findings showed a slightly raised white blood cell count of 11.3, with a C reactive protein (CRP) level of 139 mg/l. Tests for rheumatoid factor, antinuclear antibody and antineutrophil cytoplasmic antibody were negative. Immunoglobulins were normal, C3 was normal but C4 was slightly low. Cryoglobulin was not detected. Hepatitis screen was negative. The initial two sets of blood cultures showed no growth. He was treated for cutaneous vasculitis with intravenous methylprednisolone followed by oral prednisolone. He was afebrile, the rash resolved, and the arthritis and tenosynovitis showed improvement in the first week.
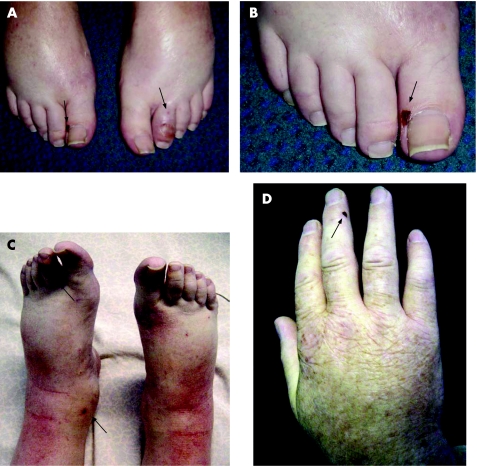
In the second week, he was unwell with fever (39°C), tenosynovitis, arthritis and rash (fig 1A–D). Investigations showed white cell count 37.4×109, neutrophils 94%, and CRP 42. Repeat blood cultures grew Neisseria gonorrhoeae. He was treated with intravenous ceftriaxone 2 g daily for 5 days followed by oral ciprofloxacin 500 mg twice daily for a week. He became afebrile with complete resolution of the rash and marked improvement in the arthritis and tenosynovitis 3 days after starting ceftriaxone treatment. CRP dropped to 12 mg/L. On inquiry, he admitted having had a casual sexual contact 6 weeks preceding the illness. Further screening for sexually transmitted diseases confirmed infection with Chlamydia trachomatis, for which he was given 1 g of azithromycin. His regular partner was also treated.
Figure 1 (A–D) Photographs of the tenosynovitis, arthritis and rash affected areas of the patient. Informed consent from patient/guardian obtained.
Discussion
Gonorrhoea is a common bacterial infection transmitted almost exclusively by sexual contact or perinatally. It can affect the mucous membrane of the urethra, cervix, rectum, oropharynx and conjunctivae. It is most prevalent in adolescent and young adults (15–24 years) living in high‐density urban areas.1
As for other sexually transmitted diseases, multiple sexual partners is one risk factor among others. Male to female transmission is more efficient than female to male.1 Our patient recalled having had unprotected sex with a new partner 6 weeks before the episode.
Disseminated gonococcal infection (DGI) generally occurs several days to 2 weeks after primary genital infection. It results from bacteraemic dissemination of N gonorrhoeae, although immune complexes and other indirect immunological mechanism may contribute to pathogenesis and symptoms in some cases.2
Septic arthritis with dermatological lesions confined to the extremities is the typical presentation of DGI.2 The strains of N gonorrhoeae associated with disseminated disease are usually very susceptible to penicillin and harbour the gonococcal specific membrane protein called 1A.3 The gonococcal strain in our patient was sensitive to penicillin, rifampicin, cefotaxime, ceftriaxone, ciprofloxacin and chloramphenicol. A combination of carbohydrate utilisation tests for detection of pre‐formed enzymes (API NH, Biomerieux, France) was used to identify N gonorrhoeae biochemically. Using the N gonorrhoeae co‐agglutination kit (Phadebact, Huddinge, Sweden), the bacteria were confirmed to have the gonococcal specific membrane protein A1.3
Strains causing DGI do not usually present with symptoms of urethral discharge,3 which was the case in our patient. Gonococcal bacteraemia is often intermittent1 and is probably the reason the first two sets of blood culture were negative. It is therefore suggested that three sets of blood cultures be obtained when DGI is suspected.1 Our patient was receiving prednisolone treatment, which would have also contributed to obtaining positive blood cultures on the third occasion.
Although disseminated gonococcal infection is very rare now and is estimated to occur in only 0.5–3% of infected patients, it should be suspected when a patient presents with tenosynovitis, arthritis and vasculitic skin lesions.2,4,5 The timely diagnosis of DGI relies heavily on consideration of its possibility and taking a careful sexual history. Appropriate samples such as urethral, pharyngeal and blood culture would be useful adjuncts to a final diagnosis.
Abbreviations
CRP - C reactive protein
DGI - Disseminated gonococcal infection
Footnotes
Competing interests: None declared.
References
- 1.Handsfield H, Spaling P. Neisseria gonorrhoea. In: Mandell GL, Bernett JE, Dolin R, eds. Principles and practice of infectious diseases. Philadelphia: Elsevier Churchill Livingstone, 20052514–2527.
- 2.Holmes K K, Counts G W, Beaty H N. Disseminated gonococcal infection. Annu Int Med 197174979–983. [DOI] [PubMed] [Google Scholar]
- 3.Taspall J W, Phillips E A, Schultz T R.et al Strain characteristics and antibiotic susceptibility of isolates of Neisseria gonorrhoea causing disseminated gonococcal infection in Australia. Int J STD AIDS 19923273–327. [DOI] [PubMed] [Google Scholar]
- 4.Mehany K, Kist J, O'Connor W.et al Disseminated gonococcemia. Int J Dermatol 200342208–209. [DOI] [PubMed] [Google Scholar]
- 5.Walters N, Butani L. A 16‐year‐old girl with recent disseminated gonococcemia now presenting with a facial rash. Annu Allergy Asthma Immunol 200594224–227. [DOI] [PubMed] [Google Scholar]