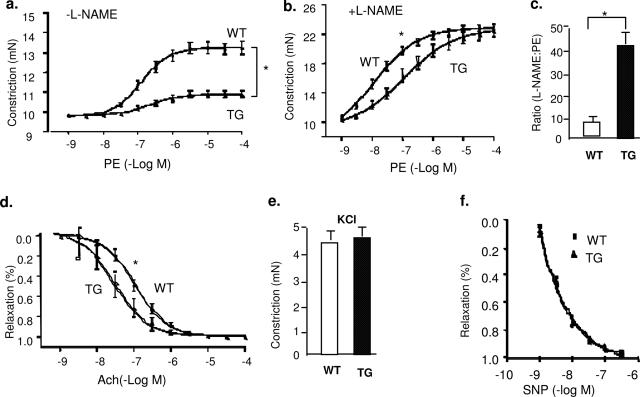
Figure 3.
Trx2 transgene expression increases basal NO release in aortic endothelium. a: Aortas from Trx2 TG show an attenuated response to PE. Aortic rings were contracted with PE at a full range of doses (10−9 to 10−4 mol/L). Constriction force (mN) is shown. b: Basal NO is increased in Trx2 TG. Aortic rings were incubated with the NOS inhibitor l-NAME to remove basal NO synthesis and then contracted with PE as in a. c: Ratio of EC50 to PE in the presence versus absence of l-NAME (100 μmol/L). d: Aortas from Trx2 TG alter the response to ACh. Aortic rings were precontracted with PE and then relaxed with ACh at a full range of doses (10−9 to 10−4 mol/L). Percentage of relaxation is shown. e: Trx2 expression had no effects on vessel constriction in response to KCl. Aortic rings were contracted with 50 mmol/L KCl. f: Trx2 expression had no effects on vessel relaxation to the NO donor drug SNP. Aortic rings were incubated with a NOS inhibitor l-NAME to remove basal NO synthesis followed by a precontraction with PE as in b and were then relaxed with SNP at a full range of doses (10−9 to 10−6 mol/L). Data are presented are mean ± SEM, with n = 5 animals and eight aortic rings per animal. *P < 0.05 indicates statistical significance by comparing WT versus TG at a dose, which causes 50% of constriction (PE) or relaxation (ACh).