Figure 5.
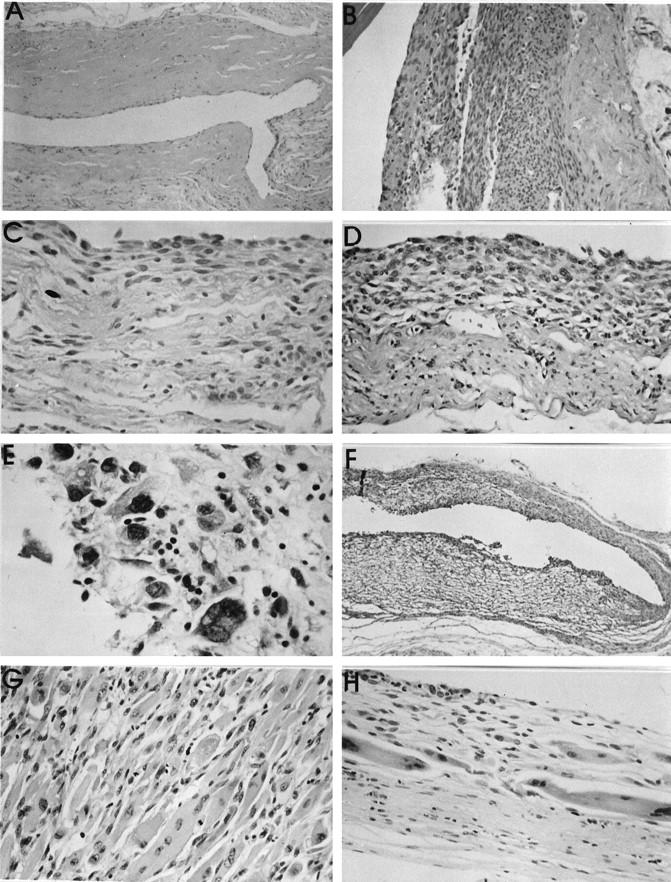
A: paucicellular fibrous tissue capsule from around a NiCr implant at 93 weeks. B: Proliferative lesion around a Ti implant after 106 weeks. No cellular atypia could be distinguished. C: Inner surface of a peri-implant capsule (Si implant at 107 weeks), showing a mixed population of polygonal and spindle-shaped cells, but without atypia. D: Capsule tissue from around a PMMA implant. The capsule is both vascular and cellular, with some pleomorphic, vesicular nuclei. The lesion was classified as a proliferative lesion, possibly preneoplastic. Objective magnification, ×20. E: High-power view (objective magnification, ×40) of a thin capsule around a Si implant. The innermost layer, immediately adjacent to the implant surface shows hyperchromatic nuclei in markedly pleomorphic cells, some of which are multinucleated. The capsule was designated as a preneoplastic lesion. F: Low-power view (objective magnification, ×5) of the entire capsule thickness (ie, both superficial and deep layers) around a PU implant. Both layers are highly cellular, but a hemangiosarcoma has developed in the superficial layer of the capsule (lower half of figure). This was not seen macroscopically. G: Histological appearance of a rhabdomyosarcoma, which developed in the deep capsule layer around a PU implant after 101 weeks. The cells contain abundant eosinophilic cytoplasm and pleomorphism and focal vesicularity of nuclei. Objective magnification, ×20. H: Superficial capsule layer of the same case as in G, showing a thin cellular layer of maximal 12 cell layers. However, large cells with abundant cytoplasm and nuclear pleomorphism are evident. This is a preneoplastic lesion with a rhabdomyoblastic phenotype. Objective magnification, ×20. All stained with HE.
