Abstract
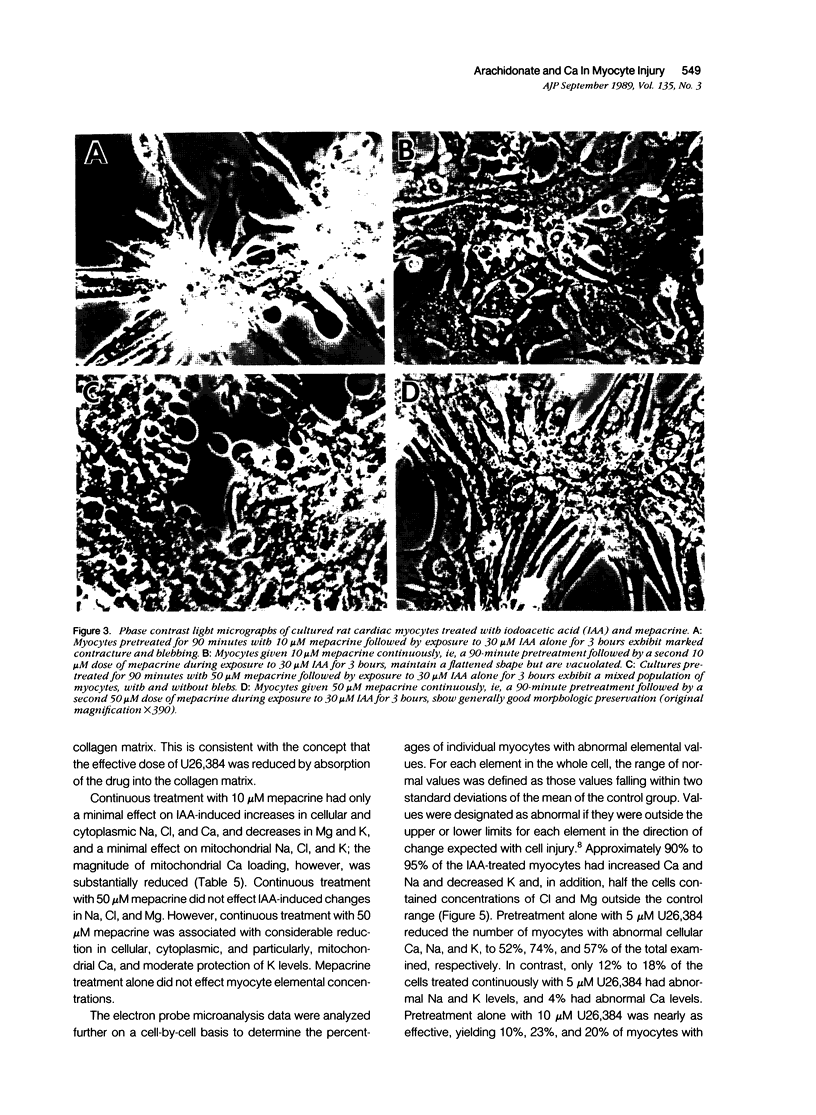
The development of irreversible myocardial ischemic injury is associated with progressive degradation of membrane phospholipids, accumulation of arachidonate and other free fatty acids, and electrolyte derangements, including calcium accumulation. To study the relationship between arachidonate release and calcium loading during adenosine triphosphate (ATP) depletion in cardiac myocytes, the effects of two purported phospholipase inhibitors, mepacrine and U26,384, were evaluated. Cultured neonatal rat ventricular myocytes were pretreated for 90 minutes with 5 to 10 microM U26,384 (a steroidal diamine) or 10 to 50 microM mepacrine (an alkyl acridine) and then treated for 3 hours with 30 microM of the metabolic inhibitor, iodoacetic acid (IAA), with or without an additional dose of drug. IAA treatment resulted in a marked reduction in ATP level and a several-fold increase in free fatty acid radioactivity released from myocytes prelabeled with tritiated arachidonic acid (3H-AA). U26,384 produced substantial inhibition of the increased 3H-AA release, and was effective when given as a single pretreatment dose before IAA exposure or as continuous treatment before and during IAA exposure (for example, with 5 microM U26,384, the percentage of 3H-AA release versus IAA alone was 8% +/- 2% [SEM] [N = 15] for pretreatment only and 13% +/- 4% [N = 10] for continuous treatment). Mepacrine also resulted in significant reduction in 3H-AA release, but was more effective when given as continuous treatment (for example, with 50 microM mepacrine, the percentage of 3H-AA release versus IAA alone was 43% +/- 9% [N = 6] for pretreatment only and 22% +/- 7% [N = 9] for continuous treatment). More detailed analysis showed that U26,384 and mepacrine blocked the IAA-induced redistribution of 3H-AA into free fatty acids from other lipid species. Electron probe x-ray microanalysis of freeze-dried cryosections revealed marked electrolyte derangements in myocytes exposed to IAA, including a 24-fold increase in cellular Ca, a four fold increase in cellular Na, and a seven fold decrease in cellular K, and associated changes in cytoplasm and mitochondria. U26,384 treatment markedly reduced these electrolyte abnormalities, and maintained normal Ca levels in some protocols. Mepacrine treatment was less effective, but did produce normal Ca levels in 50% of myocytes. Prevention of IAA-induced cellular hypercontraction and blebbing also was observed. These data support the hypothesis that reduction of free fatty acid accumulation by inhibition of accelerated phospholipid degradation is associated with protection of myocytes from calcium loading and morphologic damage during inhibition of ene
Full text
PDF













Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alonso F., Henson P. M., Leslie C. C. A cytosolic phospholipase in human neutrophils that hydrolyzes arachidonoyl-containing phosphatidylcholine. Biochim Biophys Acta. 1986 Sep 12;878(2):273–280. doi: 10.1016/0005-2760(86)90156-6. [DOI] [PubMed] [Google Scholar]
- Anderson F. S., Murphy R. C. Isocratic separation of some purine nucleotide, nucleoside, and base metabolites from biological extracts by high-performance liquid chromatography. J Chromatogr. 1976 Jun 23;121(2):251–262. doi: 10.1016/s0021-9673(00)85021-9. [DOI] [PubMed] [Google Scholar]
- BLIGH E. G., DYER W. J. A rapid method of total lipid extraction and purification. Can J Biochem Physiol. 1959 Aug;37(8):911–917. doi: 10.1139/o59-099. [DOI] [PubMed] [Google Scholar]
- Best L., Sener A., Mathias P. C., Malaisse W. J. Inhibition by mepacrine and p-bromophenacylbromide of phosphoinositide hydrolysis, glucose oxidation, calcium uptake and insulin release in rat pancreatic islets. Biochem Pharmacol. 1984 Aug 15;33(16):2657–2662. doi: 10.1016/0006-2952(84)90641-5. [DOI] [PubMed] [Google Scholar]
- Buja L. M., Hagler H. K., Parsons D., Chien K., Reynolds R. C., Willerson J. T. Alterations of ultrastructure and elemental composition in cultured neonatal rat cardiac myocytes after metabolic inhibition with iodoacetic acid. Lab Invest. 1985 Oct;53(4):397–412. [PubMed] [Google Scholar]
- Buja L. M., Willerson J. T. Abnormalities of volume regulation and membrane integrity in myocardial tissue slices after early ischemic injury in the dog: effects of mannitol, polyethylene glycol, and propranolol. Am J Pathol. 1981 Apr;103(1):79–95. [PMC free article] [PubMed] [Google Scholar]
- Burton K. P., Buja L. M., Sen A., Willerson J. T., Chien K. R. Accumulation of arachidonate in triacylglycerols and unesterified fatty acids during ischemia and reflow in the isolated rat heart. Correlation with the loss of contractile function and the development of calcium overload. Am J Pathol. 1986 Aug;124(2):238–245. [PMC free article] [PubMed] [Google Scholar]
- Burton K. P., Hagler H. K., Willerson J. T., Buja L. M. Abnormal lanthanum accumulation due to ischemia in isolated myocardium: effect of chlorpromazine. Am J Physiol. 1981 Nov;241(5):H714–H723. doi: 10.1152/ajpheart.1981.241.5.H714. [DOI] [PubMed] [Google Scholar]
- Chien K. R., Abrams J., Pfau R. G., Farber J. L. Prevention by chlorpromazine of ischemic liver cell death. Am J Pathol. 1977 Sep;88(3):539–557. [PMC free article] [PubMed] [Google Scholar]
- Chien K. R., Abrams J., Serroni A., Martin J. T., Farber J. L. Accelerated phospholipid degradation and associated membrane dysfunction in irreversible, ischemic liver cell injury. J Biol Chem. 1978 Jul 10;253(13):4809–4817. [PubMed] [Google Scholar]
- Chien K. R., Han A., Sen A., Buja L. M., Willerson J. T. Accumulation of unesterified arachidonic acid in ischemic canine myocardium. Relationship to a phosphatidylcholine deacylation-reacylation cycle and the depletion of membrane phospholipids. Circ Res. 1984 Mar;54(3):313–322. doi: 10.1161/01.res.54.3.313. [DOI] [PubMed] [Google Scholar]
- Chien K. R., Reeves J. P., Buja L. M., Bonte F., Parkey R. W., Willerson J. T. Phospholipid alterations in canine ischemic myocardium. Temporal and topographical correlations with Tc-99m-PPi accumulation and an in vitro sarcolemmal Ca2+ permeability defect. Circ Res. 1981 May;48(5):711–719. doi: 10.1161/01.res.48.5.711. [DOI] [PubMed] [Google Scholar]
- Chien K. R., Sen A., Reynolds R., Chang A., Kim Y., Gunn M. D., Buja L. M., Willerson J. T. Release of arachidonate from membrane phospholipids in cultured neonatal rat myocardial cells during adenosine triphosphate depletion. Correlation with the progression of cell injury. J Clin Invest. 1985 Jun;75(6):1770–1780. doi: 10.1172/JCI111889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das D. K., Engelman R. M., Rousou J. A., Breyer R. H., Otani H., Lemeshow S. Role of membrane phospholipids in myocardial injury induced by ischemia and reperfusion. Am J Physiol. 1986 Jul;251(1 Pt 2):H71–H79. doi: 10.1152/ajpheart.1986.251.1.H71. [DOI] [PubMed] [Google Scholar]
- Farber J. L. Biology of disease: membrane injury and calcium homeostasis in the pathogenesis of coagulative necrosis. Lab Invest. 1982 Aug;47(2):114–123. [PubMed] [Google Scholar]
- Ganote C. E., Vander Heide R. S. Cytoskeletal lesions in anoxic myocardial injury. A conventional and high-voltage electron-microscopic and immunofluorescence study. Am J Pathol. 1987 Nov;129(2):327–344. [PMC free article] [PubMed] [Google Scholar]
- Hagler H. K., Lopez L. E., Flores J. S., Lundswick R. J., Buja L. M. Standards for quantitative energy dispersive X-ray microanalysis of biological cryosections: validation and application to studies of myocardium. J Microsc. 1983 Aug;131(Pt 2):221–234. doi: 10.1111/j.1365-2818.1983.tb04248.x. [DOI] [PubMed] [Google Scholar]
- Jennings R. B., Hawkins H. K., Lowe J. E., Hill M. L., Klotman S., Reimer K. A. Relation between high energy phosphate and lethal injury in myocardial ischemia in the dog. Am J Pathol. 1978 Jul;92(1):187–214. [PMC free article] [PubMed] [Google Scholar]
- Jorgensen A. O., Broderick R., Somlyo A. P., Somlyo A. V. Two structurally distinct calcium storage sites in rat cardiac sarcoplasmic reticulum: an electron microprobe analysis study. Circ Res. 1988 Dec;63(6):1060–1069. doi: 10.1161/01.res.63.6.1060. [DOI] [PubMed] [Google Scholar]
- LOWRY O. H., ROSEBROUGH N. J., FARR A. L., RANDALL R. J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951 Nov;193(1):265–275. [PubMed] [Google Scholar]
- Löffler B. M., Bohn E., Hesse B., Kunze H. Effects of antimalarial drugs on phospholipase A and lysophospholipase activities in plasma membrane, mitochondrial, microsomal and cytosolic subcellular fractions of rat liver. Biochim Biophys Acta. 1985 Jul 31;835(3):448–455. doi: 10.1016/0005-2760(85)90114-6. [DOI] [PubMed] [Google Scholar]
- McDonald J. M., Bruns D. E., Jarett L., Davis J. E. A rapid microtechnique for the preparation of biological material for the simultaneous analysis of calcium, magnesium and protein. Anal Biochem. 1977 Oct;82(2):485–492. doi: 10.1016/0003-2697(77)90187-7. [DOI] [PubMed] [Google Scholar]
- Morris A. C., Hagler H. K., Willerson J. T., Buja L. M. Relationship between calcium loading and impaired energy metabolism during Na+, K+ pump inhibition and metabolic inhibition in cultured neonatal rat cardiac myocytes. J Clin Invest. 1989 Jun;83(6):1876–1887. doi: 10.1172/JCI114094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayler W. G. The role of calcium in the ischemic myocardium. Am J Pathol. 1981 Feb;102(2):262–270. [PMC free article] [PubMed] [Google Scholar]
- Neely J. R., Grotyohann L. W. Role of glycolytic products in damage to ischemic myocardium. Dissociation of adenosine triphosphate levels and recovery of function of reperfused ischemic hearts. Circ Res. 1984 Dec;55(6):816–824. doi: 10.1161/01.res.55.6.816. [DOI] [PubMed] [Google Scholar]
- Sen A., Miller J. C., Reynolds R., Willerson J. T., Buja L. M., Chien K. R. Inhibition of the release of arachidonic acid prevents the development of sarcolemmal membrane defects in cultured rat myocardial cells during adenosine triphosphate depletion. J Clin Invest. 1988 Oct;82(4):1333–1338. doi: 10.1172/JCI113735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somlyo A. V., McClellan G., Gonzalez-Serratos H., Somlyo A. P. Electron probe X-ray microanalysis of post-tetanic Ca2+ and Mg2+ movements across the sarcoplasmic reticulum in situ. J Biol Chem. 1985 Jun 10;260(11):6801–6807. [PubMed] [Google Scholar]
- Steenbergen C., Hill M. L., Jennings R. B. Cytoskeletal damage during myocardial ischemia: changes in vinculin immunofluorescence staining during total in vitro ischemia in canine heart. Circ Res. 1987 Apr;60(4):478–486. doi: 10.1161/01.res.60.4.478. [DOI] [PubMed] [Google Scholar]
- Steenbergen C., Hill M. L., Jennings R. B. Volume regulation and plasma membrane injury in aerobic, anaerobic, and ischemic myocardium in vitro. Effects of osmotic cell swelling on plasma membrane integrity. Circ Res. 1985 Dec;57(6):864–875. doi: 10.1161/01.res.57.6.864. [DOI] [PubMed] [Google Scholar]
- Vincent R., Nadeau D. Adjustment of the osmolality of Percoll for the isopycnic separation of cells and cell organelles. Anal Biochem. 1984 Sep;141(2):322–328. doi: 10.1016/0003-2697(84)90049-6. [DOI] [PubMed] [Google Scholar]
- Volpi M., Sha'afi R. I., Epstein P. M., Andrenyak D. M., Feinstein M. B. Local anesthetics, mepacrine, and propranolol are antagonists of calmodulin. Proc Natl Acad Sci U S A. 1981 Feb;78(2):795–799. doi: 10.1073/pnas.78.2.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh L. G., Tormey J. M. Subcellular electrolyte shifts during in vitro myocardial ischemia and reperfusion. Am J Physiol. 1988 Oct;255(4 Pt 2):H917–H928. doi: 10.1152/ajpheart.1988.255.4.H917. [DOI] [PubMed] [Google Scholar]
- Wendt-Gallitelli M. F., Isenberg G. X-ray microanalysis of single cardiac myocytes frozen under voltage-clamp conditions. Am J Physiol. 1989 Feb;256(2 Pt 2):H574–H583. doi: 10.1152/ajpheart.1989.256.2.H574. [DOI] [PubMed] [Google Scholar]
- Wendt-Gallitelli M. F., Jacob R. Rhythm-dependent role of different calcium stores in cardiac muscle: X-ray microanalysis. J Mol Cell Cardiol. 1982 Aug;14(8):487–492. doi: 10.1016/0022-2828(82)90157-2. [DOI] [PubMed] [Google Scholar]
- Wheeler-Clark E. S., Tormey J. M. Electron probe x-ray microanalysis of sarcolemma and junctional sarcoplasmic reticulum in rabbit papillary muscles: low sodium-induced calcium alterations. Circ Res. 1987 Feb;60(2):246–250. doi: 10.1161/01.res.60.2.246. [DOI] [PubMed] [Google Scholar]
- de la Peña P., Reeves J. P. Inhibition and activation of Na+-Ca2+ exchange activity by quinacrine. Am J Physiol. 1987 Jan;252(1 Pt 1):C24–C29. doi: 10.1152/ajpcell.1987.252.1.C24. [DOI] [PubMed] [Google Scholar]