Abstract
One of the most commonly cited reasons for retaining the posterior cruciate ligament (PCL) during total knee arthroplasty is to preserve femoral rollback and theoretically improve extensor mechanism efficiency (lengthening the moment arm). This study was undertaken to assess PCL function in this regard and to delineate the effects of joint line elevation that can be manipulated intraoperatively by the surgeon. The anterior movement of tibiofemoral contact following PCL resection at flexion angles 60 degrees demonstrated the beneficial effect of the PCL on extensor function. This anterior translation and the concomitant increases in quadriceps tendon load and patellofemoral contact pressures were consistently observed. This study demonstrated that small changes of the joint line position significantly influenced PCL strain and knee kinematics. In order to preserve the desired functions that would be lost with an overly lax PCL and to avoid the potential adverse effects of an overly tight PCL (posterior edge loading and increased tibiofemoral contact), the surgeon should make every effort to restore the preoperative joint line. If this is not possible, consideration should be given to posterior cruciate recession or use of a posterior cruciate substituting design.
INTRODUCTION
The decision to retain or sacrifice the posterior cruciate ligament (PCL) during total knee arthroplasty (TKA) remains a controversial issue. Rational arguments have been proposed to support the use of both PCL-retaining and PCL-sacrificing implants.2,4,5,18,20,25–27,31,35,55 Despite the theoretical advantages of each design type, there have been no substantial differences in clinical performance and both have enjoyed greater than 90% good or excellent outcomes at 1- to 10-year follow-up in most series.1,8,11,15,20,23,29,33,44,45,48–52 Yet, for a variety of reasons there is a widespread preference for retention of the PCL.18
The many arguments for retaining the PCL during TKA include improved stability, reduced shear stresses at the fixation interface, improved proprioception, and more efficient gait patterns during level walking and stair climbing.2,11,12,18,25–27,49,55 However, one of the most commonly cited reasons for retaining the PCL is to preserve femoral rollback, which improves extensor efficiency by lengthening the moment arm and improves the range of flexion by minimizing the potential for impingement of the femur on the tibial component. 2,6,12,13,18,26,49,54
Physiologic rollback in the normal knee is a complex combination of rolling, gliding and rotation of the femoral condyles relative to the tibial plateau that results in a net posterior movement of tibiofemoral contact in flexion.2,6,13,21,28,39 Normal rollback is dependent on the integrity of the cruciate ligaments, which form a four-bar planar linkage between the femur and tibia that constrains the relative movements of the articular surfaces. 28,39,40 During TKA, the ACL is resected and the complex complementary geometry of the articular surfaces is altered. Therefore, the normal interaction of the four-bar linkage mechanism and the articular surface is lost and rollback cannot occur. However, under these circumstances, if appropriately tensioned, the retained PCL can exert a beneficial checkrein effect to counteract the naturally occurring shear forces which would otherwise result in anterior translation of the femur on the tibia in flexion.56
Insall has stressed the importance of appropriately tensioning the PCL during a cruciate-retaining TKA by restoring the joint line to the pre-arthritic position, restoring the shape and size of the femoral condyles and using nonconforming relatively flat tibial inserts. If too lax postoperatively, the PCL will lose its beneficial effects and, if too tight, it could limit flexion, elevate tibiofemoral contact pressures, cause edge-loading and possibly posterior knee pain.26,38 Recent biomechanical studies have questioned whether the PCL can reliably be tensioned using contemporary techniques and instrumentation. 22,37,38
Advocates of cruciate-sacrificing have argued that the PCL cannot be appropriately tensioned during TKA in the presence of deformities and contractures associated with advanced osteoarthritis.15,33,37 This viewpoint has seemingly been supported by recent studies of PCL strain following TKA. Lotke et al.,37 observed marked variability in the strain of the anteromedial portion of the PCL in vivo in ten knees following cruciate-retaining TKA. In six of the knees the maximum postoperative strain was less than the preoperative values, and in three knees the PCL strain was elevated in early flexion. Only one of the ten knees demonstrated a postoperative pattern similar to the preoperative pattern. However, the strain was measured with unfixed trial components during passive flexion of unloaded knees, and no attempt was made to identify the zero point of strain or balance the ligament prior to testing.
Mahoney et al.,38 have also recently studied PCL strain following TKA in non-arthritic cadaver specimens and observed normal patterns in only three of eight specimens. The knees were tested in stair ascending and descending configurations and average maximum strains of 4.5 0.5% and 4.1 0.4% at 110 to 120 degrees of flexion were observed for the ascending and descending configurations respectively compared to corresponding values of 2.4 0.1% and 2.5 0.1% preoperatively. No mention was made of how the PCLs were tensioned in their study, but all knees were deemed clinically acceptable in terms of range of motion and stability, and the joint line was accurately restored.
The position of the reconstructed joint line is one of several factors that influence the tension of the retained PCL.26 In advanced arthrosis associated with coronal and sagittal plane deformities, restoration of the joint line can be quite difficult.33 For this reason, many surgeons either resect the PCL and utilize cruciate-sacrificing designs which are less sensitive to changes in the joint line position, or recess the ligament in order to achieve appropriate tension in flexion.47 Yoshii et al., have demonstrated that the joint line can accurately be restored in non-arthritic cadaver knees during TKA using standard instrumentation and techniques.58 However, in the presence of a fixed flexion contracture there is often a need to resect more distal femur in order to gain full extension. This results in joint line elevation.
The effect of joint line elevation, which results from resection of too much distal femur, has been studied for cruciate-sacrificing designs.17,33 However, there is little in the literature that documents the effects of joint line elevation using cruciate-retaining designs.9 The purpose of this investigation was to answer the following questions: To what extent does elevation of the reconstructed joint line affect PCL function? Can the retained PCL be appropriately tensioned to cause rollback and improve extensor efficiency using standard instrumentation and techniques?
Materials and Methods
Normal adult fresh-frozen cadaver knees, instrumented with an electrogoniometer, a quadriceps tendon load cell and a PCL force probe and strain gauge, were tested in a materials testing machine (MTS Corp., Eden Prairie, Minnesota). Data was collected during loading at 15, 30, 60, 90 and 105 degrees preoperatively, postoperatively at 0, 2, 4 and 6 mm of joint line elevation, and following resection of the PCL. Joint line elevation was achieved by removing shims from between the distal femoral cut and femoral component and inserting a thicker polyethylene spacer. Pressure sensitive film was utilized to ascertain patellofemoral contact pressures in each knee postoperatively.
One left and three right adult fresh-frozen cadaver limbs (two male, two female, average age 60, range 40-79 years) were thawed overnight in a sealed polyethylene bag prior to testing. Specimens with knee joint contractures, advanced arthrosis and evidence of previous trauma or surgery were excluded from the study. Antero-posterior, lateral and hip-to-ankle alignment radiographs were obtained for templating and preoperative planning. After sectioning the femur at mid shaft, the skin, fat and muscle were resected leaving the knee capsule and periarticular ligaments intact. The rectus femoris and vastus intermedius tendons were sectioned at the level of the myotendinous junction of the rectus, and prepared for application of a serpentine clamp by stripping the attached muscle fibers. Following mid-calf sectioning, the fibula was secured by a threaded Steinman pin to the approximately 24 cm long tibia, which then was potted in a copper tube with polymethylmethacrylate. A 15-mm stainless steel intramedullary rod was inserted into the reamed proximal shaft of the femur resulting in an approximate femoral length of 32 cm.
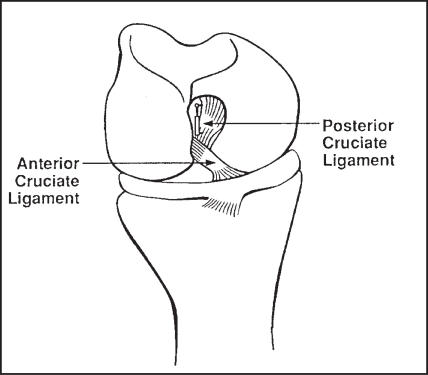
Differential variable reluctance transducers (DVRT) (Microstrain, Burlington, Vermont) were calibrated at 50 m increments through their linear and non-linear ranges using a micrometer. Occasionally, DVRT output fell outside the linear range, which necessitated interpolation of results from the calibration curves. To minimize the size of the bundle of fibers being tested, DVRT anchoring barbs were trimmed to one half of their original lengths and secured with 5-0 prolene sutures. The PCL was exposed through small medial parapatellar and posterior arthrotomies. The overlying synovium and a portion of the ligament of Humphrey were resected to facilitate application of the strain gauge and force probe to the anterior portion of the anterolateral bundle of the PCL19,57 through the medial parapatellar arthrotomy (Figure 1). Once preoperative testing was completed, the attachment sites were marked with ink and the DVRT was removed and subsequently reinserted following TKA.
Figure 1.
The DVRTs were implanted on the anterior portion of the anterolateral bundle of the PCL.
An arthroscopic force probe (Microstrain, Burlington, Vermont) was inserted parallel to the posterior fibers of the anterolateral component of the PCL through the posterior arthrotomy. The point of zero strain was identified by an abrupt change in the output of the probe as the loaded knee was taken through a range of motion. Strain (E) was calculated as:
| Equation 1 |
where; dL is the measured displacement, dL (reference) is the point of zero strain, and L (closed) is the closed length of the DVRT.
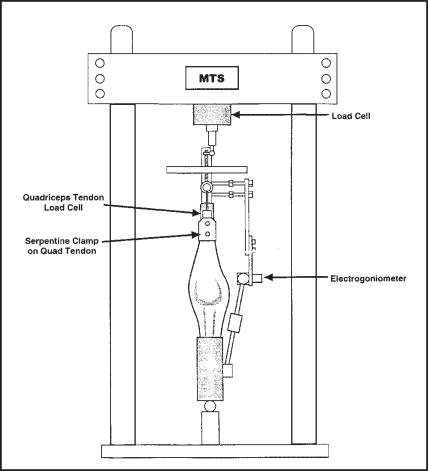
A 250-pound load cell (Sensotec, Columbus, Ohio) was placed in series with the quadriceps tendon via an attachment to the serpentine tendon clamp and eyebolt in order to measure quadriceps force. The loading fixture used was adapted from the design utilized by Huberti and Hayes.24 During loading, the Q-angle was kept physiologic by aligning the quadriceps tendon with the shaft of the femur. Knee joint motions were generated by the application of collinear compressive forces to spherical bearings representing the hip and ankle joints. A three-second-ramp signal was used to apply the desired loads. The tension on the quadriceps tendon was adjusted using an eyebolt so that the desired load was applied at the appropriate flexion angle (Figure 2).
Figure 2.
Diagram of the loading fixture. The desired moments were achieved by applying compressive forces to ball joints representing the hip and ankle. The tension in the quadriceps tendon was adjusted using an eye-bolt so that the load was applied at the appropriate flexion angle.
The target moments for stair descent were estimated to be 35, 105, 115, 80 and 60 N-m for flexion angles of 15, 30, 60, 90 and 105 degrees, respectively, from Andriacchi's study of lower-limb mechanics during stair climbing3. Subsequent to several early specimen failures at these loads, the applied moments were reduced by 75%. The applied axial force necessary to achieve a target moment was calculated as:
| Equation 2 |
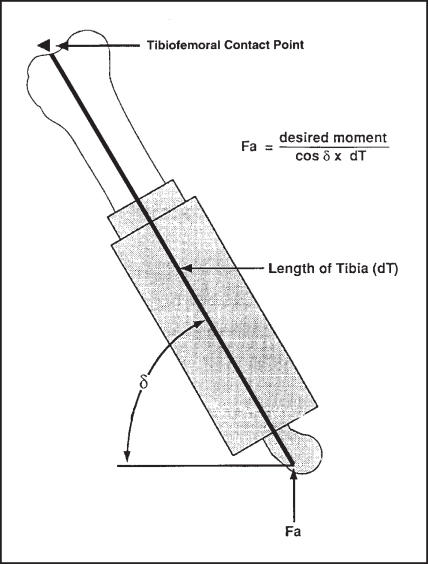
This equation assumes sagittal plane geometry and neglects the weight of the tibia and the effect of the PCL (Figure 3). The angle was measured using an angle finder (Dasco Pro Inc., Rockford, Illinois).
Figure 3.
The applied load necessary to achieve the desired moment for a given flexion angle was calculated using the above equation. The angle was measured using an angle finder and the length of the potted tibia from the ball joint to the estimated point of tibiofemoral contact was measured with a ruler.
Primary cruciate-retaining TKAs were performed using J&J P.F.C. prostheses (Johnson and Johnson Professional, Inc., Raynham, MA) and posterior curved tibial inserts. Preoperative templating with standardized antero-posterior and lateral radiographs determined anatomic axes for use of the intramedullary distal femoral cutting guide. After resection of the fat pad, the anterior cruciate ligament (ACL) and the menisci, the tibia was cut perpendicular to its longitudinal axis using an extramedullary alignment guide, paying special attention to reproduce the normal posterior slope. Approximately 8 mm of bone and cartilage were resected from the medial side leaving the posterior tibial spine and the PCL intact. Next, an 8-mm distal femoral cut was made using the appropriate bushing and an intramedullary femoral guide. A trial reduction was performed, and the tibial cut was revised with the 0 degree cutting block until the 8 mm trial tibial insert did not lift off the tibial tray ( book open) at 120 degrees of flexion. The posterior tibial spine was then carefully resected leaving the PCL fibers intact. A modular tibial tray was positioned as posteriorly as possible and cemented in the appropriate amount of rotation. Ten mm of patellar bone and cartilage were resected to accommodate the maximal thickness of the oval three-post patellar component per J&J protocols.
Once all of the standard cuts were made, an additional 6 mm of distal femur was resected leaving the PCL femoral attachment intact. Aluminum shims placed between the surface of the distal cut and the femoral component restored femoral length. The joint line was elevated by removing shims, revising the chamfer cuts and inserting the next thicker tibial insert. The femoral component was cemented at each joint line position to prevent rocking. The thickness of the shims corresponded to the minimum polyethylene thickness of the posterior curved tibial inserts (Table 1). After each successive joint line elevation, the knee was taken through a range of motion and assessed clinically for tightness in flexion by noting whether or not the tibial trial insert lifted off anteriorly.
Table 1.
The minimum thickness of the articular surface of each polyethylene tibial spacer was measured using a micrometer. The thickness of the shims used between the femoral component and the distal femoral cut to vary the position of the joint line corresponded to the differences in the minimum polyethylene thickness between spacers. For example, to elevate the joint line from 0 mm to 2 mm for the size 3 tibial tray, a 2. 1mm shim was removed from between the femoral component and the distal femoral cut and the tibial insert was changed from the 8. 0 mm size to the 10. 0 mm size.
| Minimum Polyethylene Thickness (mm) |
|||
|---|---|---|---|
| Insert Thickness | Size 3 | Size 4 | Size 5 |
| 8. 0 mm | 6. 0 | 6. 1 | 6. 1 |
| 10. 9 mm | 8. 1 | 8. 0 | 8. 1 |
| 12. 5 mm | 10. 1 | 10. 1 | 10. 2 |
| 15. 0 mm | 12. 4 | 12. 3 | 12. 3 |
Each specimen was tested preoperatively, postoperatively at 0, 2, 4 and 6 mm of joint line elevation, and following PCL resection at 0 mm of joint line elevation. A test sequence included three trials each at flexion angles of 15, 30, 60, 90 and 105 degrees. The simultaneous voltage outputs for the MTS load cell, the quadriceps load cell, the PCL DVRT, the force probe and the electrogoniometer were sampled by MTS Test Ware SX software every tenth of a second for a ten second interval that included the three second ramp load.
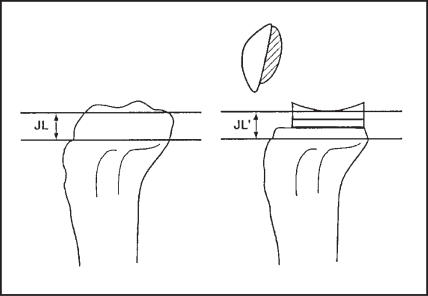
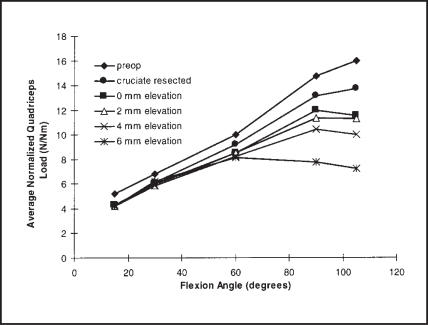
Standardized lateral radiographs centered at the joint line were obtained for each loaded specimen, pre- and postoperatively, at each flexion angle and successive joint line position, and after PCL resection. The anatomic axis, joint line position and posterior slope from the pre- and postoperative AP and lateral radiographs were measured using the method of Figgie et al.16 (Figure 4) Femoral rollback was estimated using a technique similar to that described by Stiehl et al.56 The estimated center of tibiofemoral contact was identified and its perpendicular distance from the mid-lateral tibial line was measured (Figure 5). Each radiographic measurement was repeated three times on separate occasions.
Figure 4.
The joint line was measured using the method of Figgie et al.15
Figure 5.
The location of the estimated center of tibiofemoral contact was quantified from standardized lateral radiographs relative to the mid-lateral tibial line.
Patellofemoral contact pressures were ascertained with medium range Pressensor pressure sensitive film (Inteque Resources Corp., Fort Lee, New Jersey). Two-inch square pieces of monolayer film were packaged between two sealed layers of Saran Wrap (Dow Brands L.P., Indianapolis, Indiana). The film was placed between the femoral component and the patellar component prior to loading. Reference marks were made on the film using two Kirschner wires passed through two small drill holes in the superior rim of the patellar component. Three trials were performed and the most representative stain with the least artifact was optically scanned at a resolution of 210 pixels/inch. The digital 256-gray-level images were processed to calculate the contact pressure.53 Total contact pressures were not calculated because this would have required integrating patterns from low, medium and high films. Rather, the films demonstrated differences in patellofemoral pressures at given flexion angles for the various knee testing protocols.
Normalized loads were calculated by dividing the measured forces by the applied moment. The data analysis was a repeated measures analysis of variance. The mean results for normalized quadriceps load, normalized patellofemoral contact pressure, PCL strain, and rollback between the six trials (preoperative, 4 postoperative, and cruciate resected) were compared at each angle using Bonferroni's t-test at the 0.05 significance level.
RESULTS
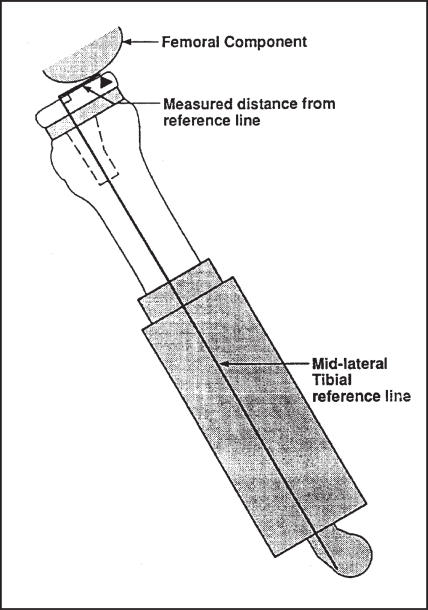
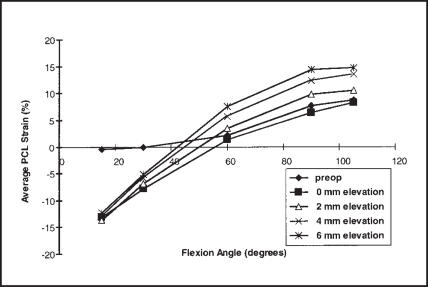
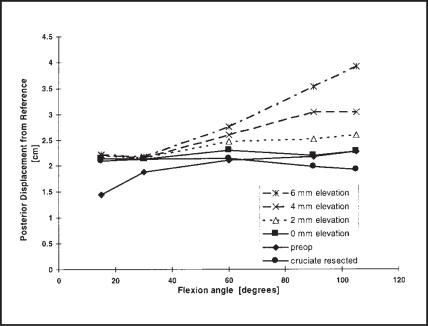
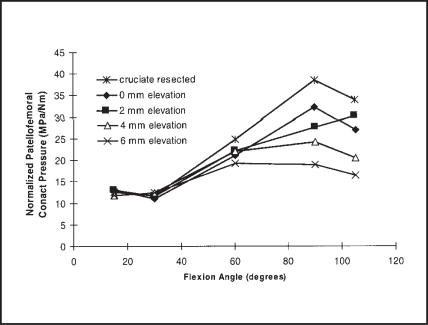
The joint line was restored within 2 mm, axial alignment within 2 degrees, and posterior slope within 3 degrees for all specimens. All knees demonstrated marked tightness in flexion at elevations of 4 and 6 mm and all but one "booked open" before 120 degrees of flexion at 2 mm of joint line elevation. The average strain recorded in the anterolateral band of the PCL is reported as a function of flexion angle for the preoperative condition and the four PCL-intact TKAs (Figure 6). Average femoral rollback is plotted as posterior displacement from the reference point through the range of flexion angles tested (Figure 7). The average normalized quadriceps tendon load and selected normalized patellofemoral contact pressures are also displayed as functions of the knee flexion angle (Figures 8 and 9, respectively). Representative digitized patellofemoral contact pressure recordings at 15, 30, 60, 90 and 105 degrees demonstrate the change of loading patterns during flexion (Figure 10).
Figure 6. AVERAGE PCL STRAIN.
Average strain of the anterolateral band of the PCL as a function of flexion angle.
Figure 7. Average Femoral Rollback.
Average femoral rollback as a function of flexion angle.
Figure 8. AVERAGE NORMALIZED QUADRICEPS TENDON LOAD.
Average normalized quadriceps tendon load as a function of flexion angle.
Figure 9. NORMALIZED PATELLOFEMORAL CONTACT PRESSURE.
Average normalized patellofemoral contact pressure as a function of flexion angle.
Figure 10.
Representative digitized patellofemoral contact pressure patterns at 15, 30, 60, 90 and 105 degrees. 1 and 2 represent the location of the reference marks which were made by indenting the film with small Kirschner wires passed through drill holes at the superior edge of the patellar button. "+" represents the center of patellofemoral contact.
DISCUSSION
Monotonic increases in strain in the anterior portion of the anterolateral component of the PCL were observed in all specimens preoperatively and postoperatively as they were flexed from 15 to 105 degrees (Figure 6). Maximum strain occurred at 105 degrees in all specimens, averaging 8.7 1.7% preoperatively and 8.3 1.5% postoperatively. The average difference between the observed strains preoperatively versus postoperatively was 26 10% at 90 degrees (range 18 - 40%) and 14 5% at 105 degrees (range 7 - 20 %). The point of zero strain occurred at an average flexion angle of 36 10 degrees preoperatively and 56 6 degrees in the postoperative specimens. As the joint line was elevated, PCL strain increased at all measured flexion angles above 30 degrees. These increases were statistically significant at 4 mm for flexion angles of 90 and 105 degrees (p=.007, p=.04) and at 6 mm for angles 60, 90 and 105 degrees (p=.007, p=.0004, p=.0007). At 2 mm of joint line elevation, the average increases in strain of 2.1, 3.4 and 2.1% at flexion angles of 60, 90 and 105 degrees, respectively, were not statistically significant. The average maximum strain of 14.7 2.2% at 6 mm of elevation and 105 degrees of flexion represents a 77% increase in PCL strain over the initial average postoperative strain. All specimens eventually failed during testing at this level of strain. (three PCLs avulsed from their tibial insertions and the fourth knee dislocated posteriorly).
In this investigation the tibial cut was revised until the 8-mm trial tibial insert did not book open at 120 degrees. This resulted in joint lines that were 0.5 to 2.0 mm below the preoperative joint line level. The observed postoperative strain patterns were similar to the preoperative patterns in that the ligament was lax in extension and became taut in flexion. However, there were consistently observed differences. Preoperatively the point of zero strain occurred at an average flexion angle of 36 10 degrees and strain increased thereafter to an average maximum of 8.7 1.7 % at 105 degrees of flexion. These values fall well within the range of previous reports.7,10,32,38 Postoperatively the point of zero strain occurred at an average flexion angle of 56 6 degrees reflecting relative laxity of the ligament in extension. This is presumably the result of resecting the ACL and the posterior tibial spine. From the point of zero strain, steady increases in PCL strain were observed as the knee was flexed to 105 degrees. The maximum average postoperative strain of 8.3 1.5% was similar to the corresponding preoperative value. This maximum average was associated with percent differences ranging from 18-40% at 90 degrees of flexion and 7-20% at 105 degrees. These differences are smaller than the previously reported values.37,38
Despite the similarities of the pre- and postoperative strain patterns, normal rollback was not observed. Rather, the average estimated tibiofemoral contact postoperatively occurred well posterior to the corresponding location preoperatively at 15 degrees and remained relatively stationary as the knee was flexed to 105 degrees. This observation corresponds well with previous reports.14,31,38,56 Following PCL resection the tibiofemoral contact did not change at lower flexion angles, but moved anteriorly an average of 1.7 0.7, 2.2 0.7 and 3.4 0.4 mm at flexion angles of 60, 90 and 105 degrees respectively compared to the corresponding values in the knees tested with the PCL intact. These differences were not statistically significant but a similar trend was observed in all specimens. These results differ from those reported by Horwood who observed no difference in the extensor mechanism moment arms in postoperative cadaver knees tested before and after PCL resection.22
The average value of 8.3 2.5 mm of preoperative femoral rollback observed in this experiment during flexion from 15 to 105 degrees is similar to reported average values of 13.5 1.5 mm from 0 to 90 degrees of flexion by Draganich12 and 8 mm from 0 to 115 degrees reported by Stiehl.56 Smooth continuous patterns were observed for all specimens (Figure 7). Postoperatively, the center of tibiofemoral contact at 15 degrees occurred an average of 6.9 3.5 mm posterior to the corresponding position preoperatively. From this relatively posterior starting point, the center of tibiofemoral contact movement was erratic and averaged a net 1.4 0.8 mm posterior as the knee was flexed to 105 degrees. The average position of the tibiofemoral center of contact at 105 degrees postoperatively was equal to the preoperative value. As the joint line was elevated the center of tibiofemoral contact did not change at the flexion angles of 15 and 30 degrees. However, at 60, 90 and 105 degrees the tibiofemoral contact center moved posteriorly with each successive elevation of the joint line. The changes in the position of the contact center were statistically significant for 60, 90 and 105 degrees at 6 mm of elevation (p=.02, p=<.0001, p=<.0001), and for 90 and 105 degrees at 4 mm of elevation (p=.0007, p=.008). This resulted in the tibiofemoral contact occurring on the posterior lip of the tibial tray in 50% of specimens at 4 mm of elevation and in all of the specimens at 6 mm of elevation and 105 degrees of flexion. The changes were not statistically different at 2 mm of elevation for any of the angles. Following resection of the PCL there was no significant statistical difference in the tibiofemoral contact center position for any angle. However, the average center moved anteriorly 1.7 0.7, 2.2 0.7 and 3.5 0.4 mm at flexion angles of 60, 90 and 105 degrees and did not change at lower flexion angles. The net average movement of the tibiofemoral center of contact following resection of the PCL from 15 to 105 degrees was 1.7 1.0 mm anterior to the starting point.
Following TKA the normalized quadriceps load decreased in all specimens at all flexion angles (Figure 8). This was most notable at flexion angles of 60, 90 and 105 degrees where average decreases of 13.2 8, 17.6 7 and 27.7 7% were observed. These decreases were not statistically significant except at the flexion angle of 105 degrees (p=.0028). Following resection of the PCL the average normalized quadriceps load increased at higher flexion angles but did not change at 15 and 30 degrees. The normalized quadriceps load increased an average of 7.4 4.1, 10.1 2.5 and 22.2 17.1% at 60, 90 and 105 degrees of flexion. These differences were not statistically significant (p>.75). Elevation of the joint line 2 mm resulted in an average decrease in quadriceps load of 5.0 and 2.5 % at 90 and 105 degrees respectively (statistically insignificant). However, elevations of 4 and 6 mm decreased the normalized quadriceps load by an average of 35 20 and 40 20% at flexion angles of 90 and 105 degrees (p=.0038, p=.0038) with no change at flexion angles of 15, 30 and 60 degrees. . Rueben et al., have also reported no statistical difference in quadriceps load postoperatively vs. preoperatively using the optimal patellar cut in ten cadaver knees from flexion of 0 to 90 degrees.46
Similar trends were observed for the average normalized patellofemoral contact pressures (Figure 9). Following resection of the PCL, the average patellofemoral contact pressure did not change at flexion angles of 15 and 30 degrees but increased by an average of 10 12, 17 8 and 26 10% for angles 60, 90 and 105 degrees. Again, these differences did not reach statistical significance but a similar trend was observed in each specimen. Elevation of the joint line decreased patellofemoral contact at flexion angles of 60, 90 and 105 degrees but these changes were not statistically significant except at 105 degrees and 6 mm of elevation (p=.06). Mahoney observed a similar decrease in extensor efficiency in cruciate-sacrificing designs in which there was no built-in mechanism for cruciate substitution. However, the patellofemoral joint was not replaced in their specimens.38
The patellofemoral contact patterns for each specimen were similar. Contact occurred on the central portion of the component at 15 and 30 degrees (Figure 10). The contact at 90 and 105 degrees was bifocal and occurred more toward the periphery of the patellar button. The pattern observed at 60 degrees represented a transition between the patterns observed at lower and higher flexion angles.
One of the functions of the retained, appropriately tensioned PCL is to counteract the natural anteriorly directed shear forces which occur in flexion and result in movement of the tibiofemoral contact center anteriorly. Based on the findings of this investigation, this effect occurs only at flexion angles greater than 60 degrees due to the laxity in the PCL at lesser flexion angles. Interestingly, this angle is similar to the angle of 69.2 2.4 degrees at which the cam mechanism for a cruciate-substituting device has been observed to engage. 38 Thus, the advantages of retaining the PCL from the improved extensor efficiency standpoint must be weighed against the associated increases in tibiofemoral contact pressures described by Soudry.55 The magnitude of these increased pressures was not addressed in this study. However, they may play a significant role in the posterior tibial wear recently reported by Feng16 and Lewis36, especially if the postoperative PCL strains are excessively high.
The effect of joint line elevation on knee range of motion following cruciate-retaining TKA has been studied by Carpenter et al.9 Significant decreases in flexion were observed with as little as 2 mm of elevation. Flexion was limited further as the joint line was elevated 4 and 6 mm, and was partially restored following cruciate excision. Similar trends were observed in this investigation. Elevating the joint line 2 mm resulted in statistically insignificant increases in the measured PCL strain averaging 2.1, 3.4 and 2.1% at flexion angles of 60, 90 and 105 degrees. Statistically significant differences were observed at these angles for joint lines 4 and 6 mm higher than the initial level. The maximum average strain observed was 14.7 2.2% at 6 mm of elevation and 105 degrees of flexion. This value is lower than reported maximum strains for intrasubstance failure; 22,42,43 however, three PCLs failed by avulsion of the tibial insertion, which represents the weak link following the proximal tibial cut.41
The tibiofemoral contact center was noted to move posteriorly at flexion angles of 60, 90 and 105 degrees as the joint line was elevated. The differences were small at 2 mm of elevation but were very significant at elevations of 4 and 6 mm where tibiofemoral contact occurred on the posterior curve and posterior lip of the tibial insert at 90 and 105 degrees.
The effect of joint line elevation on normalized quadriceps load and patellofemoral contact pressures was observed only at higher flexion angles. Statistically significant decreases were observed at 4 and 6 mm of elevation with average reductions of 35-45%. These marked decreases are not due entirely to the improved extensor mechanism moment arm. Rather they reflect a combination of the increased resistance to flexion by the excessively tight PCL, changes in the patellar ligament angle and differences in the quadriceps-to-patellar ligament force transfer ratio that accompany the abnormal knee kinematics at these joint line positions.
The results of this study must be considered in light of several limitations in addition to the small sample size. For one, no attempt was made to account for the function of the hamstrings, which have been demonstrated to influence PCL strain.7 Secondly, the model does not account for soft tissue remodeling that may occur postoperatively. Finally, the specimens used in this study had no significant underlying arthrosis and the TKAs were performed under optimal conditions. Therefore, the results observed must be interpreted as the "best case scenario" and may not be routinely achievable intraoperatively in the face of severe arthrosis.
SUMMARY
In this investigation, the maximum postoperative strain in the anterolateral portion of the PCL was similar to preoperative values in all specimens. However, the ligament consistently remained lax at flexion angles smaller than 60 degrees. Despite these similar strains at higher flexion angles, normal rollback was not observed. The anterior movement of tibiofemoral contact following PCL resection at flexion angles 60 degrees demonstrated the beneficial effect of the PCL on extensor function. This anterior translation and the concomitant increases in quadriceps tendon load and patellofemoral contact pressures were consistently observed. This study demonstrated that small changes of the joint line position significantly influenced PCL strain and knee kinematics. In order to preserve the desired functions that would be lost with an overly lax PCL and to avoid the potential adverse effects of an overly tight PCL (posterior edge loading and increased tibiofemoral contact), the surgeon should make every effort to restore the preoperative joint line. If this is not possible, consideration should be given to posterior cruciate recession or use of a posterior cruciate substituting design.
ACKNOWLEDGMENT
Financial assistance was provided by a grant from Johnson and Johnson Orthopaedics. Technical assistance was provided by Dr. M. James Rudert.
References
- 1.Aglietti P, Rinonapoli E. Total condylar knee arthroplasty: a five year follow-up study of 33 knees. Clin Orthop. 1984;186:104. [PubMed] [Google Scholar]
- 2.Andriacchi TP. Biomechanics and gait analysis in total knee replacement. Orthopaedic Review. 1988;17(5):470–473. [PubMed] [Google Scholar]
- 3.Andriacchi TP, Andersson GBJ, Fermier RW, Stern D, Galante JO. A study of lower-limb mechanics during stair climbing. J Bone and Joint Surg. 1980;62-A(5):749–757. [PubMed] [Google Scholar]
- 4.Andriacci TP, Galante JO. Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty. 1988;35:13–19. doi: 10.1016/s0883-5403(88)80003-2. [DOI] [PubMed] [Google Scholar]
- 5.Andriacci TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair climbing. J Bone and Joint Surg. 1982;64-A(9):1328–1335. [PubMed] [Google Scholar]
- 6.Andriacci TP, Tarnowski LE, Berger RA, Galante JO. New insights into femoral rollback during stairclimbing and posterior cruciate ligament function. Proceedings of the 45th Annual Meeting of the Orthopaedic Research Society. 1999. p. 20.
- 7.Arms SW, Johnson RJ, Pope MH. Strain measurement of the human posterior cruciate ligament. Proceedings of the 30th Annual Meeting of the Orthopaedic Research Society. 1984. p. 335.
- 8.Becker MW, Insall JN, Faris PM. Bilateral total knee arthroplasty. one cruciate retaining and one cruciate substituting. Clin Orthop. 1991;271:122–125. [PubMed] [Google Scholar]
- 9.Carpenter CW, Cummings JF, Grood ES, Leach DU, Paganelli JV, Manley MT. The influence of joint line elevation in total knee arthroplasty. Am J Knee Surg. 1994;7(4):164–176. [Google Scholar]
- 10.Covey DC, Sopega AA, Sherman GM, Torg JS. Testing for "isometry" during posterior cruciate ligament reconstruction. Proceedings of the 38th Annual Meeting of the Orthopaedic Research Society. 1992. p. 665.
- 11.Dorr LD, Ochsner JL, Gronley J, Perry J. Functional comparison of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. Clin Orthop. 1988;236:36–43. [PubMed] [Google Scholar]
- 12.Draganich LF, Andriacci TP, Andersson GBT. Interaction between intrinsic knee mechanics and the knee extensor mechanism. J Orthopaedic Research. 1987;5:539–547. doi: 10.1002/jor.1100050409. [DOI] [PubMed] [Google Scholar]
- 13.Dyrby CO, Andriacci TP. Three-dimensional measurement of the dynamic envelope of knee motion. Proceedings of the 45th Annual Meeting of the Orthopaedic Research Society. 1999. p. 934.
- 14.El Nahass GG, Walker PS. Does the knee joint rotate normally after total knee replacement. Proceedings of 35th Annual Meeting of the Orthopaedic Research Society. 1989. p. 372.
- 15.Faris PM, Herbst SA, Ritter MA, Keating EM. The effect of preoperative knee deformity on the initial results of cruciate-retaining total knee arthroplasty. J Arthroplasty. 1992;7(4):527–530. doi: 10.1016/s0883-5403(06)80074-4. [DOI] [PubMed] [Google Scholar]
- 16.Feng EL, Stulberg SD, Wixson RL. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop. 1994;299:60–71. [PubMed] [Google Scholar]
- 17.Figgie HE, III, Goldberg VM, Heiple KG, Moller HS, Gordon NH. The influence of tibial patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone and Joint Surg. 1986;68A(7):1035–1040. [PubMed] [Google Scholar]
- 18.Freeman MAR, Railton GT. Should the posterior cruciate ligament be retained in condylar nonmeniscal knee arthroplasty?: The case for resection. J Arthroplasty. 1988;35:3–12. doi: 10.1016/s0883-5403(88)80002-0. [DOI] [PubMed] [Google Scholar]
- 19.Harner CD. The posterior cruciate ligament relevant anatomy and biomechanics. Instructional Course 104 The PCL Injured Knee: Current Concepts; the 62nd Annual Meeting of the American Academy of Orthopaedic Surgeons; February, 1995. [Google Scholar]
- 20.Hirsch HS, Lotke PA, Morrison LD. The posterior cruciate ligament total knee surgery: save, sacrifice or substitute? Clin Orthop. 1994;309:64–88. [PubMed] [Google Scholar]
- 21.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop. 1993;290:259–268. [PubMed] [Google Scholar]
- 22.Horwood RL, Beden EN, Focht LM, Colwell CW. The role of the posterior cruciate ligament in the kinematics of total knee arthroplasty. Proceedings of the 34th Annual Meeting of the Orthopaedic Research Society. 1988. p. 360.
- 23.Horwood RL, Beden EN, Wyatt MP, Colwell CW. Gait analysis of total condylar knee arthroplasty during stair ascent. Proceedings of the 34th Annual Meeting of the Orthopaedic Research Society. 1988. p. 543.
- 24.Huberti HH, Hayes WC. Patellofemoral contact pressures: the influence of q-angle and tendofemoral contact. J Bone and Joint Surg. 1984;66-A(5):715–724. [PubMed] [Google Scholar]
- 25.Insall JN. Presidential address to the Knee Society: Choices and compromises in total knee arthroplasty. Clin Orthop. 1988;226:43–48. [PubMed] [Google Scholar]
- 26.Insall JN. Surgery of the Knee. 2nd edition. Churchill Livingstone; 1993. Surgical techniques and instrumentation in total knee arthroplasty; pp. 750–753. [Google Scholar]
- 27.Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop. 1991;268:161–178. [PubMed] [Google Scholar]
- 28.Kapandji IA. The Physiology of the Joints. II. Churchill Livingstone; 1970. [Google Scholar]
- 29.Kelman GJ, Biden EN, Wyatt, Ritter MA, Colwell CW. Gait laboratory analysis of a posterior cruciate-sparing total knee arthroplasty in stair ascent and descent. Clin Orthop. 1989;248:21–26. doi: 10.1097/00003086-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Kennedy JC, Hawkins RJ, Willis RB, Danylchuk KD. Tension studies of human knee ligament: yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone and Joint Surgery. 1976;58-A(3):350–355. [PubMed] [Google Scholar]
- 31.Kurosawa H, Walker PS, Abe S, et al. Geometry and motion of the knee for implant and orthotic design. J Biomech. 1985;18:487. doi: 10.1016/0021-9290(85)90663-3. [DOI] [PubMed] [Google Scholar]
- 32.Kurosawa H, Yamakoshi KI, Yasuda K, Saski T. Simultaneous measurement of changes in length of the cruciate ligaments during knee motion. Clin Orthop. 1991;265:233–240. [PubMed] [Google Scholar]
- 33.Laskin RS. RMC total knee replacement. J Arthroplasty. 1986;1:11. doi: 10.1016/s0883-5403(86)80005-5. [DOI] [PubMed] [Google Scholar]
- 34.Lee JG, Keating EM, Ritter MA, Garis PM. Review of all polyethylene component in total knee arthroplasty. Clin Orthop. 1990;260:87–92. [PubMed] [Google Scholar]
- 35.Lew WD, Lewis JL. The effect of knee-prosthesis geometry of cruciate ligament mechanics during flexion. J Bone and Joint Surg. 1982;64-A(5):734–739. [PubMed] [Google Scholar]
- 36.Lewis P, Rorabech CH, Bourne RB, Devane P. Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop. 1994;299:11–17. [PubMed] [Google Scholar]
- 37.Lotke PA, Corces A, Williams JL, Hirsh HS. Strain characteristics of the posterior cruciate ligament after total knee arthroplasty. Am J Knee Surg. 1993;6(3):104–107. [Google Scholar]
- 38.Mahoney O, Noble PC, Rhoads DD, Alexander JW, Tullos HS. Posterior cruciate function following total knee arthroplasty: a biomechanical study. J Arthroplasty. 1994;9(6):569–578. doi: 10.1016/0883-5403(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 39.Mow VC, Ratcliffe A, Woo SL-Y. Biomechanics of Diarthrodial Joints. II. Spinger-Verlag New York, Inc; 1990. Chapter 25; pp. 197–199. [Google Scholar]
- 40.Müller W. Kinematics of the cruciate ligaments. In: Feagin JA, editor. The Cruciate Ligaments. Churchill Livingstone; 1988. pp. 217–220. [Google Scholar]
- 41.Oschner LA, McFarland G, Boffes GC, Cook SD. Posterior cruciate ligament avulsion in total knee arthroplasty. Orthopaedic Review. 1993. Oct, [PubMed]
- 42.Prietto MP, Bain JR, Stonebrook SN, Settlage RA. Tensile strength of the human posterior cruciate ligament (PCL) Proceedings of the 34th Annual Meeting of the Orthopaedic Research Society. 1988. p. 195.
- 43.Race A, Amis AA. The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomechanics. 1994;27(1):13–24. doi: 10.1016/0021-9290(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 44.Ranawat CS, Boachie-Adjei O. Survivorship analysis and results of total condylar knee arthroplasty. Clin Orthop. 1988;226:6–13. [PubMed] [Google Scholar]
- 45.Ranawat CS, Hansraj KK. Effect of posterior cruciate sacrifice on durability of the cement-bone interface: a nine-year survivorship study of 100 total condylar knee arthroplasties. Orthop Clin North Am. 1989;20:63–69. [PubMed] [Google Scholar]
- 46.Reuben JD, McDonald CL, Woodard PC, Hennington LS. Factors affecting patella strain before and after total knee replacement. Proceedings of the 36th Annual Meeting of the Orthopaedic Research Society. 1990. p. 281.
- 47.Ritter MA, Faris PM, Keating M. Posterior cruciate ligament balancing during total knee arthroplasty. J Arthroplasty. 1988;3(4):323–326. doi: 10.1016/s0883-5403(88)80032-9. [DOI] [PubMed] [Google Scholar]
- 48.Ritter MA, Silisk J, Werland R, Faris PM, Keating EM, Meding JB, Helphenstine JV. Flat on flat, non constrained, compression molded polyethylene total knee replacement: a ten year survival analysis. Proceedings of the 1995 Knee/AAHKS Combined Specialty Day Meeting. 1995. p. 19.
- 49.Scott RD, Volatile TB. Twelve years' experience with posterior cruciate-retaining total knee arthroplasty. Clin Orthop. 1986;205:100–107. [PubMed] [Google Scholar]
- 50.Scott WN, Rubinstien M, Suuderi G. Results after knee replacement with a posterior cruciate-substituting prosthesis. J Bone and Joint Surg. 1988;70A:1163. [PubMed] [Google Scholar]
- 51.Scuderi GR, Insall JN, Windsor RE, Moran MC. Survivorship of cemented knee replacements. J Bone and Joint Surg. 1989;71B:798–803. doi: 10.1302/0301-620X.71B5.2584250. [DOI] [PubMed] [Google Scholar]
- 52.Shoji H, Wolf A, Packard S, Yoshino S. Cruciate retained and excised total knee arthroplasty: a comparative study in patients with bilateral total knee arthroplasty. Clin Orthop. 1994;305:218–222. [PubMed] [Google Scholar]
- 53.Singerman RJ, Pedersen DR, Brown TD. Quantitation of pressure-sensitive film using digital image scanning. Exp Mech. 1987;27:99. [Google Scholar]
- 54.Skyhar MJ, Warren RF, Oritz GT, Schwartz E, Otis TC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone and Joint Surg. 1993;75-A(5):694–699. doi: 10.2106/00004623-199305000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Soudry M, Walker PS, Reilly DT, Kurosawa H, Sledge CB. Effects of total knee replacement designs on femoral-tibial contact conditions. J Arthroplasty. 1986;1(1):35–43. doi: 10.1016/s0883-5403(86)80008-0. [DOI] [PubMed] [Google Scholar]
- 56.Stiehl JB, Komistek RD, Dennis DA, Paxson RD. Kinematic analysis of the knee following posterior cruciate retaining total knee arthroplasty using fluoroscopy. the 62nd Annual Meeting of the American Academy of Orthopaedic Surgeons; February, 1995. [Google Scholar]
- 57.VonDommelin BA, Fowler PJ. Anatomy of the posterior cruciate ligament: a review. Am J Sports Med. 1989;17(1):24–29. doi: 10.1177/036354658901700104. [DOI] [PubMed] [Google Scholar]
- 58.Yoshii I, Whiteside LA, White SE, Milliano MT. Influence of prosthetic joint line position on knee kinematics and patellar position. J Arthroplasty. 1991;6(2):169–179. doi: 10.1016/s0883-5403(11)80013-6. [DOI] [PubMed] [Google Scholar]