Abstract
Neutrophils contain antimicrobial peptides with antituberculous activity, but their contribution to immune resistance to tuberculosis (TB) infection has not been previously investigated to our knowledge. We determined differential white cell counts in peripheral blood of 189 adults who had come into contact with patients diagnosed with active TB in London, United Kingdom, and evaluated them for evidence of TB infection and capacity to restrict mycobacterial growth in whole-blood assays. Risk of TB infection was inversely and independently associated with peripheral blood neutrophil count in contacts of patients diagnosed with pulmonary TB. The ability of whole blood to restrict growth of Mycobacterium bovis bacille Calmette Guérin and Mycobacterium tuberculosis was impaired 7.3- and 3.1-fold, respectively, by neutrophil depletion. In microbiological media, human neutrophil peptides (HNPs) 1–3 killed M. tuberculosis. The neutrophil peptides cathelicidin LL-37 and lipocalin 2 restricted growth of the organism, the latter in an iron-dependent manner. Black African participants had lower neutrophil counts and lower circulating concentrations of HNP1–3 and lipocalin 2 than south Asian and white participants. Neutrophils contribute substantially to innate resistance to TB infection, an activity associated with their antimicrobial peptides. Elucidation of the regulation of neutrophil antimicrobial peptides could facilitate prevention and treatment of TB.
Introduction
Tuberculosis (TB) is a leading global cause of morbidity and death (1). Primary TB infection is acquired by the inhalation of droplets containing Mycobacterium tuberculosis (MTB) bacilli. If innate immunity is insufficient to eliminate infection, the acquired T cell response results in containment of infection in the majority of cases. The immune sensitization that arises can be detected by the delayed-type hypersensitivity reaction to MTB antigens in the form of the tuberculin skin test (TST).
It has long been recognized that some individuals exposed to infectious TB resist developing positive TST for longer periods than their peers despite similar exposure levels (2), raising the possibility that the innate immune response can clear infection without induction of an acquired response. Until recently, investigation of factors associated with innate resistance to MTB infection was hampered by the poor sensitivity and specificity of the TST (3). The development of more sensitive and specific blood-based methods to evaluate the T cell response to TB (known as IFN-γ release assays [IFNGRAs]) is therefore an important advance. One such test, the ELISPOT, has recently been used to determine factors associated with resistance to MTB infection in children (4).
MTB replicates in, and in turn is controlled by, macrophages. The mechanisms by which these cells kill MTB are not fully defined. Recently it has been shown that macrophages may phagocytose apoptotic neutrophils and thereby deploy neutrophil peptides with antimycobacterial activity (5). Two such classes of peptide have been identified to date in humans: the α defensins human neutrophil peptides (HNPs) 1–3 (6) and human cathelicidin LL-37 (7, 8). A third neutrophil peptide, lipocalin 2, binds soluble mycobacterial siderophores with equimolar stoichiometry (9). Siderophores are molecules that are upregulated in iron-limiting conditions and that scavenge iron and transport it into bacteria (10). Lipocalin 2 has previously been shown to restrict growth of Escherichia coli under iron-limiting conditions (in which bacteria rely on siderophores to supply their iron needs) (11), but its potential antituberculous activity has not been investigated.
To assess the potential role of neutrophils in host resistance to mycobacterial infection requires their presence in a high-throughput in vitro model. In this study we employed culture of whole blood with a recombinant M. bovis bacille Calmette Guérin (BCG) expressing luciferase, an enzyme that catalyzes the conversion of aldehyde substrate to produce light detectable in a luminometer. Because this reaction is ATP dependent, light production relates to bacillary metabolic activity and CFU (12). This model (BCG-lux assay) has yielded intuitive correlates of protection in several previous studies (13–15). We combined BCG-lux analysis with a whole-blood IFNGRA that detects response to the MTB antigens early secretory antigenic target–6 (ESAT-6) and culture filtrate protein 10 (CFP-10) and compares well with ELISPOT analysis (16). In this way we were able to evaluate overall immunity of blood cells to mycobacterial infection and sensitively detect the presence of MTB infection in a large group of TB contacts (adults who had come into contact with a patient diagnosed with active TB) recruited in London, United Kingdom; and to relate our findings to potential correlates of resistance to MTB infection.
Results
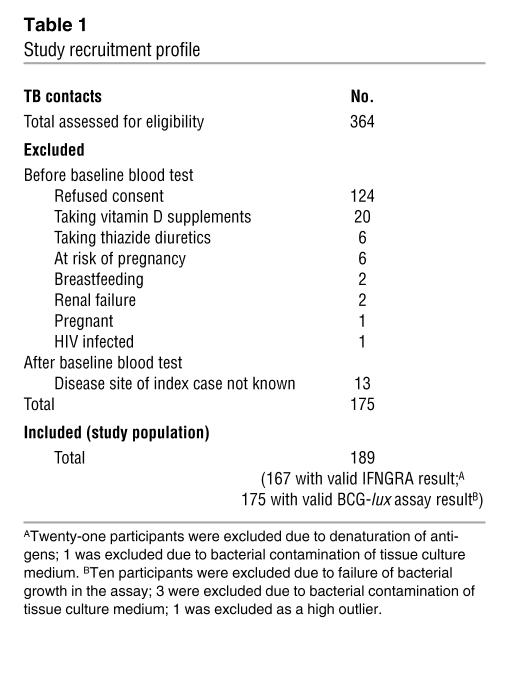
We assessed 364 TB contacts for eligibility between December 16, 2002, and January 31, 2005; 124 declined to participate, 38 were ineligible, and 13 were excluded from the analysis in the absence of information indicating whether the index case had pulmonary or extrapulmonary TB (Table 1). Baseline characteristics and whole-blood assay results for 135 contacts of patients with pulmonary TB (PTB) and 54 contacts of patients with extrapulmonary TB are shown in Table 2. Because extrapulmonary TB is noninfectious, this latter group represents a control group without recent exposure to infectious TB.
Table 1 .
Study recruitment profile
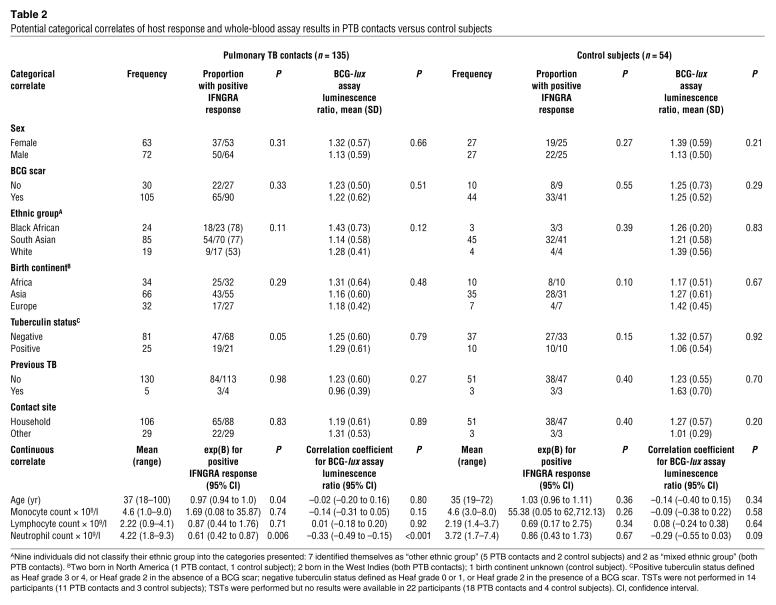
Table 2 .
Potential categorical correlates of host response and whole-blood assay results in PTB contacts versus control subjects
Of the 167 participants with a baseline result for the IFNGRA, 87 of 117 (74%) PTB contacts and 41 of 50 (82%) control subjects had a positive response. Among PTB contacts, positive tuberculin status, young age, and low peripheral blood neutrophil count were associated with positive IFNGRA response on univariate analysis. Binary logistic regression analysis conducted with age and neutrophil count as independent covariates revealed low neutrophil count, but not young age, to be independently associated with positive IFNGRA response [exp(B), 0.60; 95% confidence interval, 0.42–0.86; P = 0.006]. This association held when the analysis was restricted to south Asian PTB contacts [exp(B), 0.68; 95% confidence interval, 0.47–1.0; P < 0.05]. By contrast, no association between neutrophil count and positive IFNGRA response was observed among control subjects [exp(B), 0.86; 95% confidence interval, 0.43–1.73; P = 0.67].
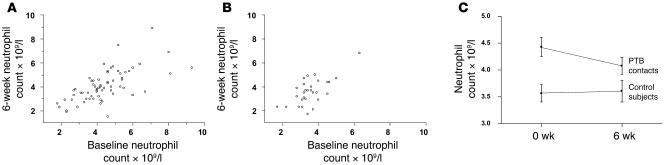
In order to investigate the kinetics of peripheral blood neutrophil count following TB exposure, we determined neutrophil count in 95 participants (66 PTB contacts and 29 control subjects) at baseline and 6 weeks after presentation to the TB contact clinic. At baseline, PTB contacts had a higher mean neutrophil count than control subjects (4.2 × 109/l versus 3.7 × 109/l respectively; P = 0.03). Follow-up counts correlated strongly and positively with baseline counts for both groups (for PTB contacts, Pearson’s r = 0.66; 95% confidence interval, 0.50–0.78; P < 0.001; for control subjects, Pearson’s r = 0.67; 95% confidence interval, 0.40–0.83; P < 0.001) (Figure 1, A and B). A small but statistically significant decrease in mean neutrophil count was observed in PTB contacts over 6 weeks (mean neutrophil count at baseline versus follow-up, 4.4 × 109/l versus 4.1 × 109/l; P = 0.02). By contrast, neutrophil counts of control subjects did not change over 6 weeks (Figure 2C).
Figure 1. Peripheral blood neutrophil counts at baseline and 6-week follow-up in PTB contacts and controls.
(A) Correlation between baseline and follow-up neutrophil count in PTB contacts. Peripheral blood neutrophil count was determined at baseline and 6 weeks later in 66 PTB contacts. Six-week counts correlated strongly and positively with baseline counts (Pearson’s r = 0.66; 95% confidence interval, 0.50 to 0.78; P < 0.001). (B) Correlation between baseline and follow-up neutrophil counts in control subjects. Peripheral blood neutrophil count was determined at baseline and 6 weeks later in 29 contacts of extrapulmonary TB. Six-week counts correlated strongly and positively with baseline counts (Pearson’s r = 0.67; 95% confidence interval, 0.40 to 0.83; P < 0.001). (C) Change in mean neutrophil counts between baseline and follow-up in PTB contacts versus control subjects. At baseline, PTB contacts had a higher mean neutrophil count than control subjects (4.2 × 109/l versus 3.7 × 109/l, respectively; P = 0.03). Mean neutrophil counts decreased in PTB contacts over 6 weeks (mean neutrophil count at baseline versus follow-up, 4.4 × 109/l versus 4.1 × 109/l, respectively; P = 0.02). Error bars represent SEM.
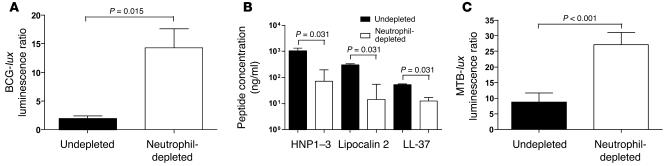
Figure 2. Effect of neutrophil depletion on containment of mycobaterial bioluminescence and secretion of antimicrobial peptides by whole blood.
(A) BCG-lux assay luminescence ratios in the presence and absence of neutrophils. Black bars, undepleted blood; white bars, depleted blood. Error bars represent SEM. Differences in luminescence ratios were compared using a paired Student’s t test. Experiments were conducted in blood of 6 healthy laboratory donors. (B) BCG-stimulated antimicrobial peptide concentration in the presence and absence of neutrophils. Error bars represent SEM. Differences in antimicrobial peptide concentrations in 96-hour supernatants were compared using Wilcoxon matched-pairs tests. Experiments were conducted in whole blood of 6 healthy laboratory donors. LL-37, human cathelicidin LL-37. (C) MTB-lux assay luminescence ratios in the presence and absence of neutrophils. Error bars represent SEM. Differences in luminescence ratios were compared using a paired Student’s t test. Experiments were conducted in blood of 6 healthy laboratory donors.
BCG-lux assay results were available for 126 of 135 (93%) PTB contacts and 49 of 54 (91%) control subjects (Tables 1 and 2). Of the potential correlates of host response investigated in PTB contacts, only neutrophil count correlated with suppression of BCG-lux luminescence (Pearson’s r = –0.33; 95% confidence interval, –0.49 to –0.15; P < 0.001). By contrast, none of the factors investigated correlated with suppression of BCG-lux luminescence among control subjects (Table 2).
To determine the extent to which neutrophils contribute to antimycobacterial response in whole blood, we compared the ability of neutrophil-depleted versus undepleted blood of 6 healthy donors to restrict BCG-lux luminescence. Neutrophil depletion resulted in a 7.3-fold increase in luminescence ratio in depleted versus undepleted blood (mean luminescence ratio, 14.31 versus 1.97; P = 0.02) (Figure 2A). BCG-stimulated antimicrobial peptide concentrations in 96-hour assay supernatants were much lower in neutrophil-depleted versus undepleted blood (median HNP1–3 concentration, 71 ng/ml versus 1,045 ng/ml; median lipocalin 2 concentration, 14 ng/ml versus 307 ng/ml; median LL-37 concentration, 12 ng/ml versus 53 ng/ml; P = 0.03 for all comparisons) (Figure 2B).
In order to determine whether neutrophil depletion also impaired containment of virulent MTB, we next compared the growth of MTB-lux in neutrophil-depleted versus undepleted blood in an additional 6 healthy donors. In keeping with the greater virulence of MTB compared with BCG, luminescence ratios in undepleted blood were higher for MTB-lux versus BCG-lux (mean luminescence ratio, 8.75 versus 1.97; P = 0.04). Neutrophil depletion resulted in a 3.1-fold increase in MTB-lux luminescence ratio in depleted versus undepleted blood (mean luminescence ratio, 27.11 versus 8.75; P < 0.001) (Figure 2C).
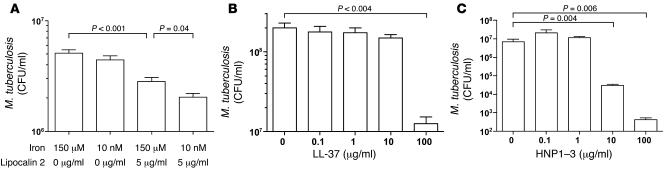
We then assayed the antituberculous activity of lipocalin 2, LL-37, and HNP1–3 in broth. Iron depletion alone had no effect on growth of MTB (Figure 3A); 5 μg/ml lipocalin 2 induced a 45% suppression of MTB CFU in iron-replete broth (150 μM iron) at 192 hours (P < 0.001). Lipocalin 2–induced suppression of MTB CFU was greater in iron-depleted broth (10 nM iron) than in iron-replete broth (60% versus 45%; P = 0.04) (Figure 3A). LL-37 induced a dose-dependent reduction in MTB CFU in iron-depleted broth that was maximal (15.7-fold) at 100 μg/ml (P = 0.004) (Figure 3B). HNP1–3 killed MTB in iron-depleted broth at concentrations greater than or equal to 10 μg/ml (P = 0.006) (Figure 3C). No synergistic effect was observed when peptides were incubated with MTB in combination (data not shown).
Figure 3. Effect of antimicrobial peptides on growth of Mycobacterium tuberculosis in microbiological broth media.
(A) Effect of lipocalin 2 on growth of MTB in iron-replete and iron-depleted broth. Effect of lipocalin 2 (5 μg/ml) on growth of an inoculum of 3 × 104 CFU/ml MTB was determined in iron-replete (150 μM Fe) and iron-depleted (10 nM Fe) 7H9 broth medium. The mean of 6 replicates is shown. Error bars represent SEM. (B) Effect of cathelicidin LL-37 on the growth of MTB in broth. Effect of cathelicidin LL-37 (0.1–100 μg/ml) on growth of an inoculum of 6 × 105 CFU/ml MTB was determined in iron-depleted (10 nM Fe) 7H9 broth medium. The mean of 4 replicates is shown. Error bars represent SEM. (C) Effect of HNP1–3 on the growth of MTB in broth. Effect of HNP1–3 (0.1–100 μg/ml) on growth of an inoculum of 6 × 105 CFU/ml MTB was determined in iron-depleted (10 nM Fe) 7H9 broth medium. The mean of 4 replicates is shown. Error bars represent SEM.
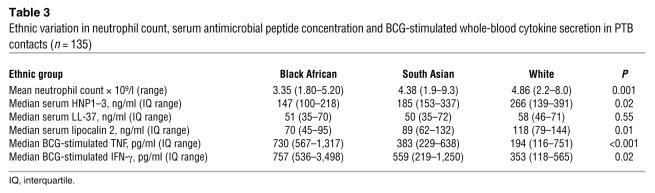
Finally we determined serum antimicrobial peptide concentrations in PTB contacts. Serum lipocalin 2 concentrations correlated with suppression of BCG-lux luminescence in whole blood (Spearman’s r = –0.26; 95% confidence interval, –0.43 to –0.19; P = 0.003), but concentrations of HNP1–3 and LL-37 did not (data not shown). Black African participants had lower neutrophil counts (P = 0.001) and lower serum concentrations of HNP1–3 (P = 0.02) and lipocalin 2 (P = 0.01) than south Asian and white participants. By contrast, BCG-stimutated whole blood of black African participants secreted more TNF (P < 0.001) and IFN-γ (P = 0.02) than that of south Asian and white participants (Table 3).
Table 3 .
Ethnic variation in neutrophil count, serum antimicrobial peptide concentration and BCG-stimulated whole-blood cytokine secretion in PTB contacts (n = 135)
Discussion
We have demonstrated an inverse relationship between peripheral blood neutrophil count and risk of MTB infection in a cohort of PTB contacts and shown that neutrophils make a very significant contribution to host defense in a whole-blood model of mycobacterial infection. Neutrophil antimicrobial peptides possess antituberculous activity in broth: HNP1–3 are potently tuberculocidal, while LL-37 and lipocalin 2 restrict growth of tuberculosis — the latter by a novel, iron-dependent mechanism. PTB contacts’ circulating concentrations of lipocalin 2 also correlated strongly with the ability of their whole blood to restrict luminescence of a reporter mycobacterium in vitro. Black African TB contacts had lower serum levels of HNP1–3 and lipocalin 2 than south Asian and white TB contacts.
Our interpretation of IFNGRA results assumes that a negative assay result indicates an absence of MTB infection. The possibility that a negative result might represent a lack of response to MTB antigens rather than absence of infection cannot be discounted, given the lack of a gold standard diagnostic test for MTB infection. However, the IFNGRA employed in this study has been validated in tuberculin-negative individuals (16, 17), and whole-blood IFNGRAs are reported to have specificity rates as high as 98% in BCG-vaccinated populations with no risk factors for MTB exposure (3).
Our observation that neutrophil count and risk of MTB infection were not associated in a control group of individuals not recently exposed to infectious TB suggests that high peripheral blood neutrophil count may particularly contribute resistance to early infection. This hypothesis presupposes high interindividual variability but low day-to-day intraindividual variability in neutrophil count among contacts of infectious TB. Numerous studies testify that this is the rule in adult populations (18), and our data are in keeping with this literature. Interestingly, we found that PTB contacts had slightly higher neutrophil counts than control subjects at baseline. These counts fell during the following 6 weeks, suggesting that early exposure to MTB infection induces a transient rise in peripheral blood neutrophil count. Active PTB is also associated with increased numbers of neutrophils in peripheral blood (19), although, paradoxically, high neutrophil counts at diagnosis are associated with poor outcome (20). Neutrophils isolated from the peripheral blood of PTB patients also exhibit reduced phagocytic activity and depressed respiratory burst in vitro (21, 22). Clearly, the capacity of neutrophils to induce protective or pathogenic responses relates to their numbers and activity at the site of disease, and peripheral blood neutrophil count may only be a correlate of this. The factors regulating both function and temporal and spatial patterning of neutrophils following exposure to infectious TB are therefore worthy of further investigation.
Individuals of black African, Afro-Caribbean, and Middle Eastern ethnic origin are recognized to have lower levels of neutrophils than white individuals, possibly due to differences in release of mature neutrophils from the bone marrow storage pool (23). Rates of MTB infection were higher among black African PTB contacts than among whites in this study, and ethnicity-related factors therefore have the potential to confound the relationship observed between low neutrophil count and positive IFNGRA response. Our demonstration that this association was preserved even when analysis was restricted to south Asian participants indicates that confounding by ethnicity-related factors does not explain the association we describe.
Neutrophil depletion of whole blood resulted in at least as great an impairment in suppression of BCG-lux luminescence as T cell depletion (14). This striking observation suggests that neutrophils make a large contribution to antimycobacterial activity in this assay. The finding that some antimicrobial peptides were detectable in the supernatants of neutrophil-depleted blood (Figure 2B) can be explained by our observation that 1%–7% of neutrophils were not removed by depletion. Moreover, cathelicidin LL-37 is expressed by mononuclear phagocytes as well as neutrophils (24): this cell population may therefore also contribute to secretion of this peptide in neutrophil-depleted samples.
Of the neutrophil antimicrobial peptides investigated, HNP1–3 were the only peptides to kill MTB in iron-depleted broth, at concentrations of at least 10 μg/ml — 1,000 times lower than those found in neutrophil granules (25). By contrast, LL-37 and lipocalin 2 restricted growth of MTB rather than inducing killing. The antibacterial effects of antimicrobial peptides are recognized to depend on ionic environment (26), and the fact that we demonstrate more potent antituberculous activity of HNP1–3 and LL-37 in broth than other investigators (7, 27) may be attributable to the iron-depleted culture conditions we employed. Our demonstration that lipocalin 2–induced antituberculous activity in broth is more marked under iron-depleted conditions is consistent with the hypothesis that it acts by sequestrating mycobacterial siderophores, thereby depriving MTB of iron. It may be that lipocalin 2 exerts more potent antimycobacterial activity in the phagolysosome, where the molar ratio of lipocalin 2 to siderophore is likely to be higher and where lipocalin 2 might act in concert with other molecules that restrict availability of free iron (28): our demonstration of a strong and highly statistically significant correlation between serum lipocalin 2 level and suppression of luminescence in the BCG-lux assay (not observed for HNP1–3 or LL-37) is consistent with this hypothesis.
It has previously been reported that African American individuals are more susceptible to TB infection than white individuals (29), and given our findings, it is possible that ethnic neutropenia might contribute to this phenomenon. Interestingly, we did not observe statistically significant ethnic variation in BCG-lux assay luminescence ratios in this study. The antigen-stimulated whole blood of black Africans living in Malawi has previously been shown to secrete higher levels of TNF and IFN-γ than that of white individuals living in the United Kingdom (30, 31), and we also found that BCG-stimulated TNF and IFN-γ secretion was higher for black African participants than for south Asian and white participants. These are 2 of the best-characterized cytokines necessary for protection against TB (32), and it may be that the more pronounced BCG-stimulated TNF and IFN-γ responses we observed in whole blood of black Africans represent compensatory mechanisms to restrict mycobacterial luminescence when neutrophil numbers are low.
In summary, we have demonstrated that neutrophils make a very significant contribution to innate immunity to TB, an activity associated with their antimicrobial peptides. Elucidation of the regulation of these peptides could lead to the development of novel strategies to prevent and treat TB.
Methods
Participants.
The study was approved by the Research Ethics Committees of North East London and Harrow (REC P/02/146 and EC 2759, respectively), and written informed consent to participate was obtained from all subjects. Study participants were recruited from TB contact clinics at Newham University Hospital and Northwick Park Hospital. All people over 17 years of age who had been exposed to a patient with active TB were assessed. Exclusions were symptoms, clinical signs, or radiographic evidence of active TB; HIV infection, renal failure, sarcoidosis, or hyperparathyroidism; corticosteroid, thiazide, or vitamin D therapy; breastfeeding; and pregnancy. The TST was performed and read according to UK national guidelines (33). Participants self-classified ethnicity into 1 of the following 5 categories (34): black/black British (black African), Asian/British Asian (south Asian), white, mixed, or other. Blood for neutrophil depletion assays was taken from healthy laboratory donors.
Preparation and culture of recombinant mycobacteria.
BCG and MTB H37Rv transformed with a replicating vector containing the luciferase (lux) gene of Vibrio harveyi were prepared as previously described (12). Frozen aliquots of BCG-lux bacilli were grown to mid–log phase in Middlebrook 7H9 broth supplemented with 10% albumin dextrose catalase enrichment (BD Biosciences) and 15 μg/ml hygromycin (Roche Diagnostics). Whole blood was infected with equal numbers of log-phase bacilli corresponding to a multiplicity of infection (mononuclear phagocyte/bacillus) of approximately 1:1. RLU/CFU enumerations were performed periodically to confirm plasmid stability.
To produce iron-depleted broth media, 7H9 was prepared in acid-washed bottles from its constituent ingredients, omitting ferric ammonium citrate. These media were subsequently adjusted with ferric ammonium citrate to attain specified iron concentrations. Iron-depleted stocks of MTB-lux were grown to log phase in broth containing 2 μM iron (a concentration of iron low enough to induce bacillary siderophore production) (35) and frozen in 15% glycerol. For assays of HNP1–3 and LL-37 activity, inocula of 6 × 105 CFU/ml were cultured for 168 hours in medium containing HNP1–3 isolated from human blood (PANATecs) or synthetic LL-37 (PANATecs) at a 10-nM final iron concentration (the concentration of free iron estimated to exist in the phagolysosome) (10). For assays of lipocalin 2 activity, inocula of 3 × 104 CFU/ml were cultured for 192 hours at final iron concentrations of both 10 nM and 150 μM (the concentration of iron in undepleted 7H9 broth) in the presence or absence of 5 μg/ml recombinant lipocalin 2 (R&D Systems). This concentration of lipocalin 2 is sufficient to saturate estimated siderophore production of this inoculum of MTB (36).
Whole-blood assays.
The IFNGRA used in this study has been described elsewhere (16). Triplicate samples of venous blood diluted 1:10 with RPMI-1640 (Invitrogen) were cultured with 2.5 μg/ml recombinant ESAT-6 (37), 5 μg/ml CFP-10 (Lionex), 5 μg/ml phytohemagglutinin (ICN Biomedicals), or no stimulus at 37°C in 5% CO2. Supernatants were aspirated at 96 hours for determination of IFN-γ concentration by ELISA. An antigen-stimulated increment in supernatant IFN-γ concentration greater than or equal to 10 pg/ml in response to either ESAT-6 or CFP-10 was taken to indicate the presence of MTB infection. The BCG-lux assay has also previously been described (13). Triplicate samples of 0.5 ml venous blood diluted with an equal volume of RPMI-1640/2 mM glutamine/25 mM HEPES buffer (Life Technologies) were infected with 3 × 105 CFU BCG-lux and incubated for 96 hours. Mycobacterial luminescence was measured at baseline and 96 hours in a luminometer, and a luminescence ratio calculated by division of the 96-hour RLU value by the baseline value. To deplete neutrophils, blood from healthy donors diluted as described above was incubated for 20 minutes at 4°C with magnetic beads conjugated to anti-CD15 antibodies (Miltenyi Biotec) at a ratio of 50 μl beads per 2 ml diluted blood. MS depletion columns (Miltenyi Biotec) were attached to a separation magnet and primed with 500 μl magnetic affinity cell sorting buffer (PBS/0.5% BSA/2 mmol EDTA) followed by 500 μl RPMI/glutamine/HEPES buffer. Two columns were used to deplete 6 ml diluted whole blood. Control samples without antibody-coated beads were prepared and treated under identical conditions. Fluorescence-activated cell sorting showed depletion of 93%–99% neutrophils in depleted fractions without significant loss of mononuclear phagocytes. Coulter counter (Beckman Coulter) analysis of undepleted versus depleted samples from 6 donors confirmed that the depletion procedure affected neither lymphocyte nor monocyte counts (mean lymphocyte count, undepleted versus depleted blood, 7.67 × 108/l versus 8.00 × 108/l, respectively; P = 0.17; mean monocyte count, undepleted versus depleted blood, 1.67 × 108/l versus 1.83 × 108/l, respectively; P = 0.61).
ELISA.
ELISAs were performed using antibody pairs from R&D Systems for TNF and from BD for IFN-γ. The sensitivity of these assays was less than 10 pg/ml. Serum and supernatant concentrations of antimicrobial peptides were assayed using kits from Hycult Biotechnology for LL-37 and HNP1–3 and Antibody Shop for lipocalin 2.
Statistics.
Analysis of potential correlates of risk of MTB infection was conducted using χ2 tests for categorical determinants and binary logistic regression analysis for continuous determinants. Pearson’s r and Spearman’s ρ were calculated to test for correlation between continuous variables with Gaussian and non-Gaussian distribution, respectively. Median values of variables with non-Gaussian distribution were compared between groups using Wilcoxon matched-pairs tests, Mann-Whitney U tests, and Kruskal-Wallis tests. Mean values of variables with Gaussian distribution were compared between groups using paired Student’s t tests, unpaired Student’s t tests, and 1-way ANOVA. Reported P values are 2-sided. A P value of less than 0.05 was considered significant.
Acknowledgments
This work was supported by the Wellcome Trust (grants 064261, 066321, 072070, and 077273), the Department of Environmental Health, London Borough of Newham, Newham University Hospital NHS Trust Research Fund, and Northwick Park Hospital Tropical Research Fund. We thank staff of the Department of Hematology, St. Mary’s Hospital, London, United Kingdom, for Coulter counter analysis of neutrophil-depleted blood samples. Bradley February of the Institute for Infectious Diseases and Molecular Medicine, University of Cape Town, South Africa, for assistance in CFU enumeration; Adam Whelan of the Veterinary Laboratories Agency, Surrey, United Kingdom, for the gift of recombinant ESAT-6; and John White of the Department of Physiology, McGill University, Montreal, Quebec, Canada, for helpful discussion and review of the manuscript.
Footnotes
Nonstandard abbreviations used: BCG, Mycobacterium bovis bacille Calmette Guérin; CFP-10, culture filtrate protein 10; ESAT-6, early secretory antigenic target–6; HNP, human neutrophil peptide; IFNGRA, IFN-γ release assay; MTB, Mycobacterium tuberculosis; PTB, pulmonary TB; TB, tuberculosis; TST, tuberculin skin test.
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 117:1988–1994 (2007). doi:10.1172/JCI31097
References
- 1.Dye C. Global epidemiology of tuberculosis. Lancet. 2006;367:938–940. doi: 10.1016/S0140-6736(06)68384-0. [DOI] [PubMed] [Google Scholar]
- 2.Israel H.L., Hetherington H.W., Ord J.G. A study of tuberculosis among students of nursing. JAMA. 1941;117:839–844. [Google Scholar]
- 3.Connell T.G., Rangaka M.X., Curtis N., Wilkinson R.J. QuantiFERON-TB Gold: state of the art for the diagnosis of tuberculosis infection? Expert Rev. Mol. Diagn. 2006;6:663–677. doi: 10.1586/14737159.6.5.663. [DOI] [PubMed] [Google Scholar]
- 4.Soysal A., et al. Effect of BCG vaccination on risk of Mycobacterium tuberculosis infection in children with household tuberculosis contact: a prospective community-based study. Lancet. 2005;366:1443–1451. doi: 10.1016/S0140-6736(05)67534-4. [DOI] [PubMed] [Google Scholar]
- 5.Tan B.H., et al. Macrophages acquire neutrophil granules for antimicrobial activity against intracellular pathogens. J. Immunol. 2006;177:1864–1871. doi: 10.4049/jimmunol.177.3.1864. [DOI] [PubMed] [Google Scholar]
- 6.Fu L.M. The potential of human neutrophil peptides in tuberculosis therapy. Int. J. Tuberc. Lung Dis. 2003;7:1027–1032. [PubMed] [Google Scholar]
- 7.Liu P.T., et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311:1770–1773. doi: 10.1126/science.1123933. [DOI] [PubMed] [Google Scholar]
- 8.Martineau A.R., et al. IFN-gamma- and TNF-independent vitamin D-inducible human suppression of mycobacteria: the role of cathelicidin LL-37. J. Immunol. 2007;178:7190–7198. doi: 10.4049/jimmunol.178.11.7190. [DOI] [PubMed] [Google Scholar]
- 9.Holmes M.A., Paulsene W., Jide X., Ratledge C., Strong R.K. Siderocalin (Lcn 2) also binds carboxymycobactins, potentially defending against mycobacterial infections through iron sequestration. Structure. 2005;13:29–41. doi: 10.1016/j.str.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Ratledge C. Iron, mycobacteria and tuberculosis. Tuberculosis. 2004;84:110–130. doi: 10.1016/j.tube.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Goetz D.H., et al. The neutrophil lipocalin NGAL is a bacteriostatic agent that interferes with siderophore-mediated iron acquisition. Mol. Cell. 2002;10:1033–1043. doi: 10.1016/s1097-2765(02)00708-6. [DOI] [PubMed] [Google Scholar]
- 12.Snewin V.A., et al. Assessment of immunity to mycobacterial infection with luciferase reporter constructs. Infect. Immun. 1999;67:4586–4593. doi: 10.1128/iai.67.9.4586-4593.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kampmann B., et al. Evaluation of human antimycobacterial immunity using recombinant reporter mycobacteria. J. Infect. Dis. 2000;182:895–901. doi: 10.1086/315766. [DOI] [PubMed] [Google Scholar]
- 14.Tena G.N., et al. Failure to control growth of mycobacteria in blood from children infected with human immunodeficiency virus and its relationship to T cell function. J. Infect. Dis. 2003;187:1544–1551. doi: 10.1086/374799. [DOI] [PubMed] [Google Scholar]
- 15.Kampmann B., Tena-Coki G.N., Nicol M.P., Eley B. Reconstitution of antimycobacterial immune responses in HIV-infected children receiving HAART. AIDS. 2006;20:1011–1018. doi: 10.1097/01.aids.0000222073.45372.ce. [DOI] [PubMed] [Google Scholar]
- 16.Scholvinck E., et al. Gamma interferon-based immunodiagnosis of tuberculosis: comparison between whole-blood and immunospot methods. J. Clin. Microbiol. 2004;42:829–831. doi: 10.1128/JCM.42.2.829-831.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson S.T., et al. Transmission of Mycobacterium tuberculosis undetected by tuberculin skin testing. Am. J. Respir. Crit. Care Med. 2006;173:1038–1042. doi: 10.1164/rccm.200509-1526OC. [DOI] [PubMed] [Google Scholar]
- 18.Garrey W.E., Bryan W.R. Variations in white blood cell counts. Phys. Rev. 1935;15:597–638. [Google Scholar]
- 19.Veenstra H., et al. Changes in leucocyte and lymphocyte subsets during tuberculosis treatment; prominence of CD3dimCD56+ natural killer T cells in fast treatment responders. Clin. Exp. Immunol. 2006;145:252–260. doi: 10.1111/j.1365-2249.2006.03144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnes P.F., et al. Predictors of short-term prognosis in patients with pulmonary tuberculosis. J. Infect. Dis. 1988;158:366–371. doi: 10.1093/infdis/158.2.366. [DOI] [PubMed] [Google Scholar]
- 21.Shalekoff S., Tiemessen C.T., Gray C.M., Martin D.J. Depressed phagocytosis and oxidative burst in polymorphonuclear leukocytes from individuals with pulmonary tuberculosis with or without human immunodeficiency virus type 1 infection. Clin. Diagn. Lab. Immunol. 1998;5:41–44. doi: 10.1128/cdli.5.1.41-44.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fiorenza G., Bottasso O.A., Rateni L., Farroni M.A., Dlugovitzky D. Impaired neutrophil function in patients with pulmonary tuberculosis and its normalization in those undergoing specific treatment, except the HIV-coinfected cases. FEMS Immunol. Med. Microbiol. 2003;35:159–164. doi: 10.1016/S0928-8244(03)00004-X. [DOI] [PubMed] [Google Scholar]
- 23.Haddy T.B., Rana S.H., Castro O. Benign ethnic neutropenia: what is a normal absolute neutrophil count? J. Lab. Clin. Med. 1999;133:15–22. doi: 10.1053/lc.1999.v133.a94931. [DOI] [PubMed] [Google Scholar]
- 24.Wang T.T., et al. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J. Immunol. 2004;173:2909–2912. doi: 10.4049/jimmunol.173.5.2909. [DOI] [PubMed] [Google Scholar]
- 25.Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat. Rev. Immunol. 2003;3:710–720. doi: 10.1038/nri1180. [DOI] [PubMed] [Google Scholar]
- 26.Dorschner R.A., et al. The mammalian ionic environment dictates microbial susceptibility to antimicrobial defense peptides. FASEB J. 2006;20:35–42. doi: 10.1096/fj.05-4406com. [DOI] [PubMed] [Google Scholar]
- 27.Kisich K.O., Higgins M., Diamond G., Heifets L. Tumor necrosis factor alpha stimulates killing of Mycobacterium tuberculosis by human neutrophils. Infect. Immun. 2002;70:4591–4599. doi: 10.1128/IAI.70.8.4591-4599.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barry C.E., Boshoff H. Getting the iron out. Nat. Chem. Biol. 2005;1:149–153. doi: 10.1038/nchembio0805-127. [DOI] [PubMed] [Google Scholar]
- 29.Stead W.W., Senner J.W., Reddick W.T., Lofgren J.P. Racial differences in susceptibility to infection by Mycobacterium tuberculosis. N. Engl. J. Med. 1990;322:422–427. doi: 10.1056/NEJM199002153220702. [DOI] [PubMed] [Google Scholar]
- 30.Weir R.E., et al. Mycobacterial purified protein derivatives stimulate innate immunity: Malawians show enhanced tumor necrosis factor alpha, interleukin-1beta (IL-1beta), and IL-10 responses compared to those of adolescents in the United Kingdom. Infect. Immun. 2004;72:1807–1811. doi: 10.1128/IAI.72.3.1807-1811.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Black G.F., et al. BCG-induced increase in interferon-gamma response to mycobacterial antigens and efficacy of BCG vaccination in Malawi and the UK: two randomised controlled studies. Lancet. 2002;359:1393–1401. doi: 10.1016/S0140-6736(02)08353-8. [DOI] [PubMed] [Google Scholar]
- 32. Wilkinson, R.J., and Young, D.B. 2004. Novel vaccines against tuberculosis. In New generation vaccines. M. Levine, J. Kaper, R. Rappuoli, M. Liu, and M. Good, editors. Marcel Dekker. New York, New York, USA. 519–535. [Google Scholar]
- 33.Joint Tuberculosis Committee of the British Thoracic Society. . Control and prevention of tuberculosis in the United Kingdom: code of practice 2000. Thorax. 2000;55:887–901. doi: 10.1136/thorax.55.11.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Office for National Statistics. 2003. Ethnic group statistics: a guide for the collection and classification of ethnicity data. Her Majesty’s Stationery Office. London, United Kingdom. 63 pp. [Google Scholar]
- 35.Rodriguez G.M., Voskuil M.I., Gold B., Schoolnik G.K., Smith I. ideR, an essential gene in mycobacterium tuberculosis: role of IdeR in iron-dependent gene expression, iron metabolism, and oxidative stress response. Infect. Immun. 2002;70:3371–3381. doi: 10.1128/IAI.70.7.3371-3381.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ratledge C., Hall M.J. Influence of metal ions on the formation of mycobactin and salicylic acid in Mycobacterium smegmatis grown in static culture. J. Bacteriol. 1971;108:314–319. doi: 10.1128/jb.108.1.314-319.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rhodes S.G., et al. Antigen specificity in experimental bovine tuberculosis. Infect. Immun. 2000;68:2573–2578. doi: 10.1128/iai.68.5.2573-2578.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]