Abstract
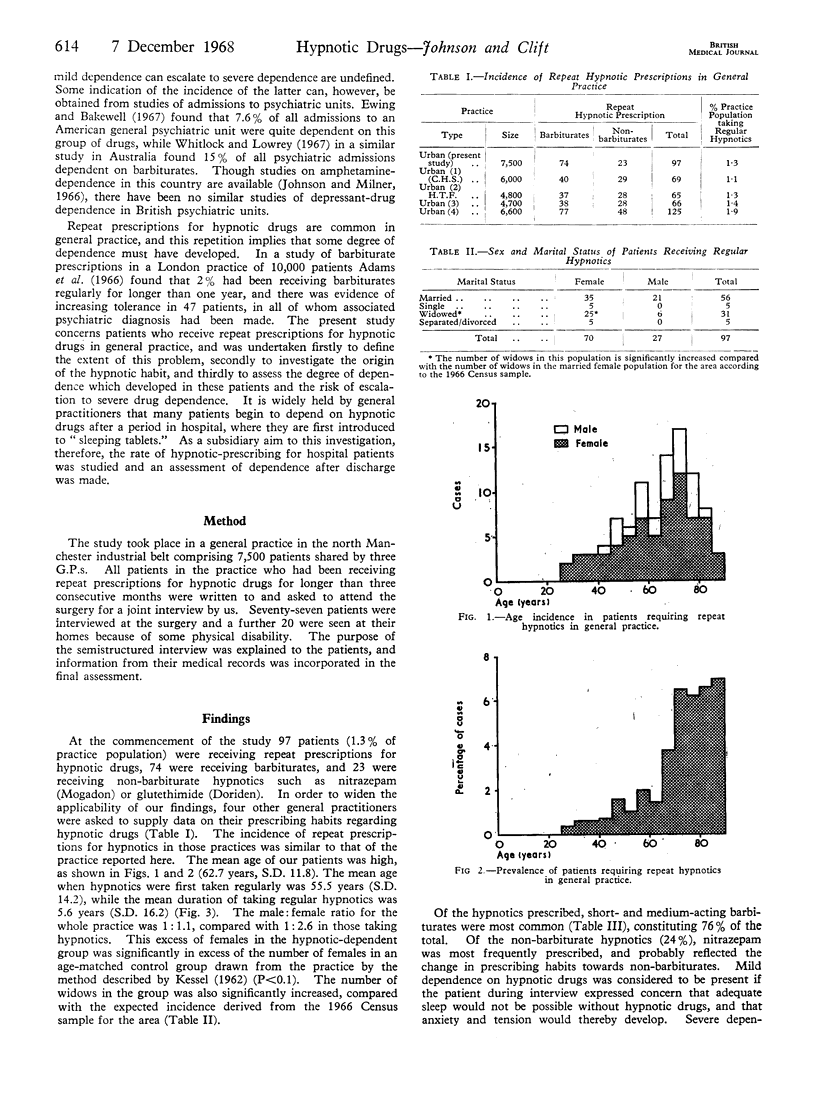
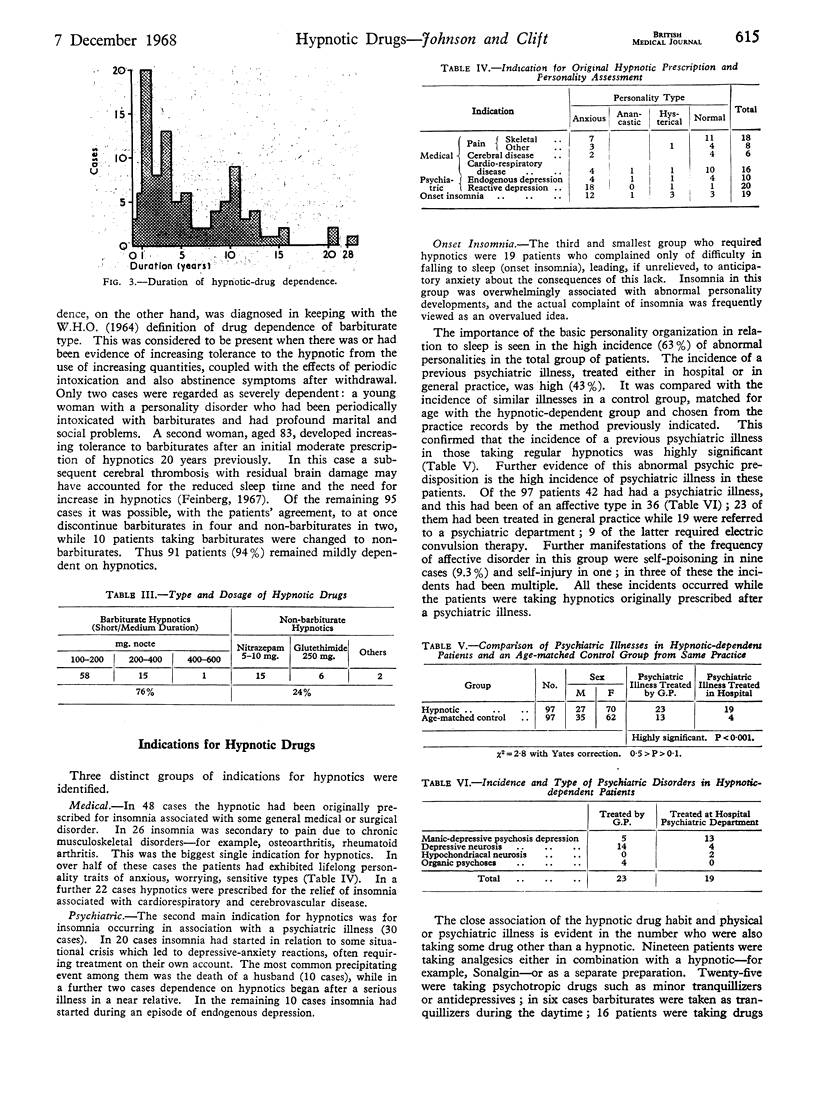
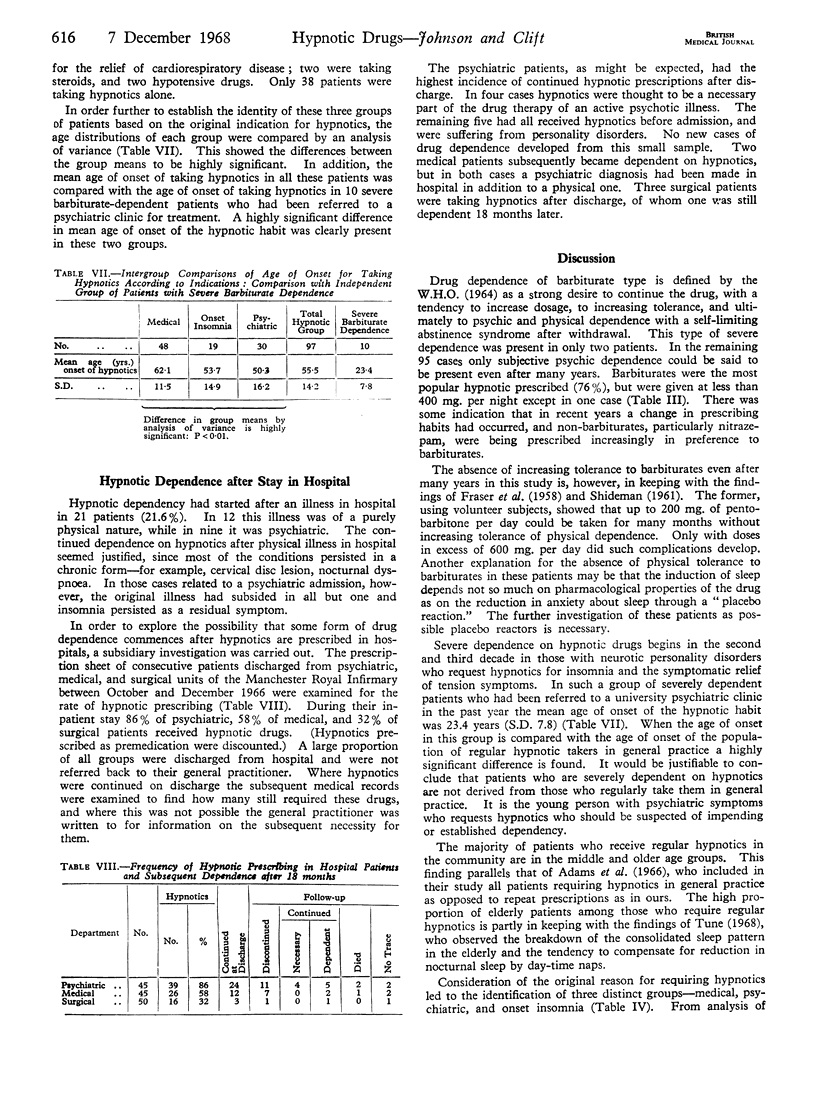
Of the patients in an industrial general practice 1.3% required hypnotic drugs regularly. They were predominantly in the older age groups (mean 62.7 years), with an excess of widows. Only 0.02% were severely dependent; the remainder were mildly so, though they had been taking hypnotics for long periods (mean 5.6 years). There were three main original indications for hypnotics—namely, medical (pain), psychiatric, and onset insomnia in anxious personality disorder. One-fifth of the patients first took hypnotics while in hospital. The group as a whole manifested a high degree of abnormal psychological disposition.
It is suggested that many patients who take hypnotics regularly may be placebo reactors, and a more critical attitude to hypnotic prescribing is required both in hospital and in general practice.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROOKE E. M., GLATT M. M. MORE AND MORE BARBITURATES. Med Sci Law. 1964 Oct;4:277–282. doi: 10.1177/002580246400400408. [DOI] [PubMed] [Google Scholar]
- Bewley T. H. Recent changes in the incidence in all types of drug dependence in Great Britain. Proc R Soc Med. 1968 Feb;61(2):175–177. [PMC free article] [PubMed] [Google Scholar]
- ESSIG C. F. ADDICTION TO NONBARBITURATE SEDATIVE AND TRANQUILIZING DRUGS. Clin Pharmacol Ther. 1964 May-Jun;5:334–343. doi: 10.1002/cpt196453334. [DOI] [PubMed] [Google Scholar]
- Ewing J. A., Bakewell W. E. Diagnosis and management of depressant drug dependence. Am J Psychiatry. 1967 Feb;123(8):909–917. doi: 10.1176/ajp.123.8.909. [DOI] [PubMed] [Google Scholar]
- FRASER H. F., WIKLER A., ESSIG C. F., ISBELL H. Degree of physical dependence induced by secobarbital or pentobarbital. J Am Med Assoc. 1958 Jan 11;166(2):126–129. doi: 10.1001/jama.1958.02990020014002. [DOI] [PubMed] [Google Scholar]
- Feinberg I. Sleep electroencephalographic and eye-movement patterns in patients with schizophrenia and with chronic brain syndrome. Res Publ Assoc Res Nerv Ment Dis. 1967;45:211–240. [PubMed] [Google Scholar]
- HINTON J. M. Patterns of insomnia in depressive states. J Neurol Neurosurg Psychiatry. 1963 Apr;26:184–189. doi: 10.1136/jnnp.26.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HINTON J. M. The actions of amylobarbitone sodium, butobarbitone and quinalbarbitone sodium upon insomnia and nocturnal restlessness compared in psychiatric patients. Br J Pharmacol Chemother. 1961 Feb;16:82–89. doi: 10.1111/j.1476-5381.1961.tb00300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JOYCE C. R. Psychological effects of medication. Differences between physicians as revealed by clinical trials. Proc R Soc Med. 1962 Sep;55:776–778. [PMC free article] [PubMed] [Google Scholar]
- Johnson J., Milner G. Psychiatric complications of amphetamine substances. Acta Psychiatr Scand. 1966;42(3):252–263. doi: 10.1111/j.1600-0447.1966.tb01930.x. [DOI] [PubMed] [Google Scholar]
- Kessel N. Self-poisoning. I. Br Med J. 1965 Nov 27;2(5473):1265–1270. doi: 10.1136/bmj.2.5473.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tune G. S. Sleep and wakefulness in normal human adults. Br Med J. 1968 May 4;2(5600):269–271. doi: 10.1136/bmj.2.5600.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock F. A., Lowrey J. M. Drug-dependence in psychiatric patients. Med J Aust. 1967 Jun 10;1(23):1157–1166. doi: 10.5694/j.1326-5377.1967.tb21849.x. [DOI] [PubMed] [Google Scholar]