Abstract
BACKGROUND
While acute illness and hospitalization represent pivotal events for older persons, their contribution to recoverable cognitive dysfunction (RCD) has not been well examined.
OBJECTIVE
Our goals were to estimate the frequency and degree of RCD in an older hospitalized cohort; to examine the relationship of RCD with delirium and dementia; and to determine 1-year cognitive outcomes.
DESIGN
Prospective cohort study.
PARTICIPANTS
Four hundred and sixty patients aged ≥70 years drawn from consecutive admissions to an academic hospital.
MEASUREMENTS
Patients underwent interviews daily during hospitalization and at 1 year. The primary outcome was RCD, defined as an admission Mini-Mental State Examination (MMSE) score that improved by 3 or more points by discharge.
RESULTS
Recoverable cognitive dysfunction occurred in 179 of 460 (39%) patients, with MMSE impairment at baseline ranging from 3 to 13 points (median=5.0 points). The majority of cases were not characteristic of either delirium or dementia, as 144 of 179 (80%) cases did not meet criteria for delirium, and 133 of 164 (81%) cases did not meet criteria for dementia at baseline. In multivariable analysis controlling for baseline MMSE level, 3 factors were predictive of RCD: higher educational level, preadmission functional impairment, and higher illness severity. At 1 year, further improvement in MMSE score occurred in 38 of 92 (41%) patients with RCD. Recoverable cognitive dysfunction was independently predictive of 1-year mortality with an adjusted odds ratio of 1.82 (95% confidence interval [95% CI] 1.03 to 3.20).
CONCLUSIONS
Acute illness is accompanied by a high rate of RCD that is neither characteristic of delirium or dementia. Our observations underscore the reversible nature of this cognitive dysfunction with continued improvement over the ensuing year, and highlight the potential clinical implications of this under-recognized phenomenon.
Keywords: delirium, dementia, cognitive impairment, hospitalization, geriatrics
The onset of acute illness often initiates a cascade of events leading to decline in cognitive functioning, and ultimately culminating in nursing home placement or death.1–3 While delirium has been widely recognized as an important complication of hospitalization for older persons,4–6 more subtle reversible cognitive dysfunction related to acute illness has not been well examined. Fields et al.7 and Hickey et al.8 documented substantial rates of cognitive impairment during hospitalization of 19.8% and 31%, respectively; however, neither study analyzed the reversibility of the impairments or their relationship to delirium or dementia. In a separate study, Fields et al.9 examined a subgroup of the patients and found that 9 of 19 (47%) cognitively impaired medical patients improved their Mini-Mental State Examination (MMSE) scores to their baseline level or by 4 or more points after 3 months. Finally, Treloar and Macdonald10,11 found that 31 of 59 (52%) patients admitted to an acute geriatric unit demonstrated a 5-point or greater increase in MMSE score after 3 months. Both of these latter studies represented small sample sizes, and their methods did not allow estimation of the prevalence rates of recoverable cognitive dysfunction (RCD) in their study populations. Cassell et al.12 demonstrated impairment on 7 Piagetian tasks of judgment in 24 hospitalized patients compared with 28 controls, but these tasks are not validated cognitive measures for adults.
With the aging of the US population, improved understanding of recoverable cognitive dysfunction in hospitalized acutely ill older persons is worthy of attention. There are no previous studies to guide us in how much change in cognitive functioning regularly occurs during hospitalization. Elucidating the prevalence and predictors for recoverable cognitive dysfunction would assist in instituting measures to ameliorate further functional losses. In addition, the presence of cognitive impairment may affect the patient's ability to participate in decision-making and informed consent regarding medical treatment. Cognitive ability would also influence discharge planning and the ability of the patient to live independently. Finally, clarifying the influence of acute illness on cognitive functioning may help to elucidate the pathophysiology of delirium and dementia more broadly.
We conducted a prospective cohort study to examine the prevalence of and predictors for recoverable cognitive dysfunction in an acutely ill older population. The objectives were: (1) to estimate the frequency and degree of RCD—as measured by improvement in MMSE scores by the time of hospital discharge; (2) to evaluate how often cases of RCD meet criteria for delirium or dementia; (3) to determine the predictors for RCD; and (4) to determine the 1-year cognitive outcomes of patients classified by degree of RCD.
METHODS
Setting and Patients
The study followed a prospective cohort design, and utilized the control group from the Delirium Prevention Trial,13 which has been described in detail previously. Study participants were drawn from consecutive patients admitted to the general medicine service at Yale New Haven Hospital from March 25, 1995 through March 18, 1998. One-year follow-up interviews were completed by September 1999. Yale New Haven Hospital is an 800-bed urban teaching hospital with 200 medical beds, serving predominantly a large community sample and a smaller referral population. Of 567 eligible patients, 469 agreed to participate and 9 patients were excluded due to the lack of 2 MMSE scores during hospitalization, required for our study outcome. Therefore, the final study cohort included 460 patients.
Procedures
All study procedures were carried out by experienced research interviewers, who were blinded to the research questions and underwent intensive training. Interrater reliability assessments were carried out for key measures at baseline and every 6 months. The baseline interview, completed within 48 hours of admission, included the MMSE,14 Digit Span Test,15 Confusion Assessment Method (CAM) rating,16 Activities of Daily Living17,18 referent to 2 weeks before hospitalization, Jaeger test for vision, Whisper test for hearing,19 demographics, and chart review for the Acute Physiology and Chronic Health Evaluation (APACHE II) score20 and Charlson comorbidity index.21 A family member was interviewed at admission to describe the patient's cognitive functioning before admission and to complete the modified Blessed Dementia Rating Scale (mBDRS).22,23 Subsequently, patients were interviewed daily until discharge with a structured interview including the MMSE, Digit Span Test, and CAM rating.
At 1-year after hospital discharge, patients underwent a follow-up telephone interview to determine vital status and follow-up MMSE scores. This interview used a modified, validated 23-point telephone MMSE.24 If patients could not be interviewed, proxy interviews were obtained, which included reasons why the patient could not be interviewed.
Informed consent for study participation was obtained from the patients or, for those with substantial cognitive impairment, from a proxy, according to procedures approved by the institutional review board of Yale University School of Medicine.
Outcome
The primary outcome was RCD, defined as reduction in the admission MMSE score that improved by at least 3 points by the time of hospital discharge. Hospital discharge was chosen as the reference point, because we believed it was important clinically to identify patients: (1) who had overall cognitive improvement by the time of hospital discharge, and (2) who left the hospital with better cognitive function than upon admission. A 3 or more point change was selected as clinically significant as previous studies have demonstrated test–retest variations (including learning effects) of 1 to 2 points maximum25,26 and longitudinal changes of 2 to 3 points maximum27–29 in cognitively stable patients. Thus, the outcome definition requires that
Multiple alternative definitions for RCD were considered, including improvement in admission MMSE by at least 5 points, improvement by at least 10%, and improvement above the threshold of 28 points. Each of these alternative definitions had serious limitations, and our chosen definition had the greatest clinical sensibility. We present 1-year outcomes for our original definition plus the alternative definition of improvement in admission MMSE by at least 5 points, which yields the greatest contrast with our chosen definition.
To evaluate the degree of RCD, we calculated the difference between the highest daily MMSE score during hospitalization and the admission score for each patient. The highest score during hospitalization was chosen as the best approximation of the patient's full cognitive potential (i.e., reflecting their preadmission “baseline” cognitive function), rather than the discharge value.
At follow-up, improvement in MMSE score was defined as a higher MMSE score at 1 year compared with the in-hospital maximum MMSE score. Similarly, no change or decline at 1 year was defined by comparison with the in-hospital maximum MMSE score.
Definitions of Study Variables
Dementia was defined based on the presence of cognitive symptoms for at least 6 months and a mBDRS score of 4 or more points, a validated cutpoint22,23 used previously.30,31 To evaluate how often cases of RCD met criteria for delirium, both full and partial definitions of delirium based on CAM criteria16 were examined at the time of the baseline assessment. Full delirium was defined as the presence of 3 to 4 CAM features according to the CAM diagnostic algorithm (i.e., presence of (1) acute onset and fluctuating course, (2) inattention, and either (3) disorganized thinking, or (4) altered level of consciousness); partial forms of delirium had at least 1 of the following key CAM features: inattention, disorganized thinking, or altered level of consciousness. Because the intent was to examine the interrelationship of RCD and delirium, delirium was examined at baseline only (i.e., simultaneous with the admission MMSE assessment). To examine predictors associated with degree of RCD, the following baseline factors were evaluated after controlling for the baseline MMSE score: age, gender, nursing home residence, education, mBDRS score, presence of delirium at baseline (based on full CAM criteria), ADL score, APACHE II score, and Charlson comorbidity score.
Statistical Analyses
The demographic and clinical characteristics of the study population at baseline were presented as means and proportions. The association between RCD and delirium was examined among patients with full, partial, or no delirium. In addition, the association of RCD with dementia was examined. We used a multiple linear regression model to examine the potential predictors of RCD. All models controlled for admission MMSE score (continuous, with lower scores indicating more impairment). We modeled the degree of RCD, defined as the difference between the maximum MMSE score during hospitalization and admission. A selection procedure using backward selection with an inclusion criterion of P≤.10 was applied to the 10 candidate predictors including age (continuous), male gender (vs female), nursing home residence (vs not nursing home), education (continuous), modified Blessed Dementia Rating Scale score (continuous, with higher score indicating more impairment), presence of delirium at baseline (vs no delirium), Activities of Daily Living score (continuous, 0 to 7, with higher score indicating more impairment), APACHE II score (continuous, with higher scores indicating higher illness severity), and Charlson comorbidity score (continuous, with higher scores indicating more comorbidity). The strength of the linear relationship between the selected predictors and degree of RCD was assessed using the model R2. Model fit was assessed using residual analyses and collinearity diagnostics. Notably, the same variables were selected by backward, forward, and stepwise selection procedures.
To assess the impact of RCD on 1-year mortality, we created an ordinal cognitive predictor variable reflecting our a priori hypothesis of mortality risk, with the group who have cognitive decline having the highest mortality, followed by the RCD group, followed by the group with baseline cognitive impairment or dementia who remain stable, followed by the nonimpaired group (referent category). We tested the ordinal outcome in a multivariable logistic regression model for prediction of 1-year mortality, controlling for age, ADL score, and APACHE II score.
Because the telephone follow-up interview used a shortened MMSE with a total score of 23, these scores were prorated by a factor of 1.3 to yield a total score of 30. This adjustment facilitated comparison with the highest MMSE score during hospitalization, which was based on the 30-point MMSE. The 23-point telephone MMSE24 has been validated against the full 30-point MMSE.
All statistical tests were 2-tailed, and P<.05 was considered statistically significant. All analyses were performed using the SAS statistical program (Version 9.1, SAS Institute Inc., Cary, NC) and Stata version 9.0 (StataCorp, College Station, TX).
RESULTS
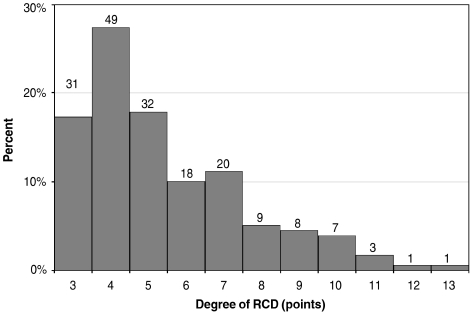
Baseline characteristics of the study sample are shown in Table 1. Overall, these 460 patients represent an elderly, frail population with a mean age of 80 years, 13% with dementia, 35% with impairment in at least 1 ADL, and who had at least moderate degrees of illness severity and comorbidity. Of the 460 patients, 179 (39%) demonstrated RCD, that is, an admission MMSE score that improved by 3 or more points by hospital discharge. Among those with RCD, the degree of RCD ranged from 3 to 13 points (Fig. 1), with a median of 5.0 points, and mean±SD of 5.4±2.2 points. Overall MMSE scores (mean±SD) at baseline were 23.2±4.9 (N=460), at discharge 25.0±5.0 (N=460), and at 1-year follow-up 27.4±3.3 (N=263).
Table 1.
Baseline Characteristics of the Study Population
| Characteristic | Patients (N = 460) |
|---|---|
| Age (y), mean ± SD | 80.0 ± 6.5 |
| Male, n (%) | 183 (39.8) |
| Nonwhite, n (%) | 69 (15.0) |
| Nursing home residence, n (%) | 30 (6.5) |
| Education (y), mean ± SD* | 11.0 ± 3.6 |
| Modified Blessed DRS score, mean ± SD* | 1.5 ± 2.0 |
| Dementia, n (%)—define as mBDRS≥4* | 56 (13.2) |
| Any ADL impairment, n (%) | 162 (35.2) |
| APACHE II score, mean ± SD | 15.6 ± 4.1 |
| Charlson score, mean ± SD | 2.7 ± 2.2 |
| Principal diagnosis, n (%) | |
| Chronic lung disease | 55 (12.0) |
| Congestive heart failure | 54 (11.7) |
| Pneumonia | 49 (10.7) |
| Gastrointestinal disease | 47 (10.2) |
| Ischemic heart disease | 42 (9.1) |
| Diabetes mellitus or metabolic disorder | 17 (3.7) |
| Cerebrovascular disease | 13 (2.8) |
| Cancer | 12 (2.6) |
| Renal failure | 9 (2.0) |
| Anemia | 5 (1.1) |
| Other | 157 (34.1) |
Missing values present for some variables. Education, missing = 3; mBDRS score, missing = 35.
SD, standard deviation; mBDRS, modified Blessed Dementia Rating Scale; ADL, activities of daily living; APACHE II, Acute Physiology and Chronic Health Evaluation II.
FIGURE 1.
Degree of recoverable cognitive dysfunction (RCD) at hospital admission (N = 179). This figure demonstrates the number and percent of patients with reduction in MMSE scores at hospital admission, compared with their highest MMSE score at any time during hospitalization, among RCD patients only. For this study, recoverable cognitive dysfunction was defined as an admission MMSE score that improved 3 or more points by the time of hospital discharge. The amount of reduction in MMSE scores ranged from 3 to 13 points, with a median of 5.0 points. The number of patients is indicated above each bar. MMSE, Mini-Mental State Examination.
Table 2 demonstrates the relationship of RCD with the presence of delirium at baseline. These results indicate that RCD occurred in patients who were not delirious at baseline in the majority of cases; in fact, 144 of 179 (80%) patients with RCD had no delirium at baseline. However, patients with full or partial delirium were significantly more likely to develop RCD (35 of 60, 58%) than those without delirium (144 of 400, 36%, P<.001). The relationship of RCD and dementia is examined in Table 3. Patients with dementia demonstrated a high rate of development of RCD, in 31 of 56 (55%) cases, and were significantly more likely to demonstrate RCD than patients without dementia (133 of 369, 36%, P=.006).
Table 2.
Relationship of Recoverable Cognitive Dysfunction with Delirium at Baseline
| Recoverable Cognitive Dysfunction | |||
|---|---|---|---|
| Delirium status at baseline assessment (N = 360) | Total Sample N (%) | Present (n) | Absent (n) |
| Full or partial CAM criteria | 60 (13.0) | 35 | 25 |
| Full criteria | 8 (1.7) | 5 | 3 |
| Partial criteria | 52 (11.3) | 30 | 22 |
| No delirium | 400 (87.0) | 144 | 256 |
| Totals | 460 (100) | 179 | 281 |
CAM, Confusion Assessment Method; see text for definitions.
Table 3.
Relationship of Recoverable Cognitive Dysfunction with Baseline Dementia*
| Recoverable Cognitive Dysfunction | |||
|---|---|---|---|
| Baseline Dementia Status (N = 333) | Total Sample N (%) | Present (n) | Absent (n) |
| Dementia (mBDRS ≥ 4) | 56 (13.2) | 31 | 25 |
| No dementia | 369 (86.8) | 133 | 236 |
| Totals | 425 (100) | 164 | 261 |
35 patients with missing mBDRS scores at baseline were excluded from these analyses.
Factors associated with the degree of RCD are presented in Table 4. After controlling for baseline MMSE score, the final independent factors identified by multivariable analysis were educational level, baseline ADL score, and APACHE II score. Each year of education was associated with 0.12 point more RCD (i.e., more impairment in admission MMSE); thus, persons with higher educational level had higher degrees of RCD. Each 1-point increase in ADL score (with higher scores indicating more impairment) was associated with 0.18 points more RCD; thus, persons with more ADL impairments at baseline demonstrated higher degrees of RCD. Finally, each 1-point increase in APACHE II score was associated with a 0.05 point more RCD at admission; thus, more severely ill persons demonstrated higher degrees of RCD.
Table 4.
Baseline Factors Associated with Degree of Recoverable Cognitive Dysfunction*
| Full Model† | Final Model† | |||
|---|---|---|---|---|
| β | P Value | β | P Value | |
| Age‡ | −0.01 | .738 | ||
| Male gender (vs female) | −0.24 | .267 | ||
| Nursing home residence (vs N) | 0.17 | .719 | ||
| Education‡ | 0.14 | <.001 | 0.12 | <.001 |
| mBDRS score‡ | −0.10 | .134 | ||
| Delirium at baseline (vs N) | −1.02 | .190 | ||
| ADL score‡ | 0.20 | .007 | 0.18 | .002 |
| APACHE II score‡ | 0.05 | .075 | 0.05 | .056 |
| Charlson comorbidity score‡ | 0.03 | .558 | ||
All factors are taken from baseline (admission), and all analyses control for baseline level of MMSE. mBDRS, modified Blessed Dementia Rating Scale; MMSE, Mini-Mental State Examination; ADL, activities of daily living; APACHE, Acute Physiology and Chronic Health Evaluation; N, none or not present.
Multiple linear regression models. N = 422 for models due to missing values (35 missing mBDRS, 3 missing education). For final model, N = 457 (3 missing education), adjusted R2 = 0.3576, F = 64.45, P<.0001
Handled as continuous variables in model. ADL scored 0 to 7, with 7 indicating independence in all ADLs. See text for details.
Table 5 indicates the 1-year outcomes in the RCD group according to degree of RCD. At 1-year follow-up, 92 of 179 patients with RCD were alive and had completed MMSE scores. Continued improvement in 1-year MMSE scores, compared with best in-hospital score, occurred in 38 (41%) patients with RCD. Stratified by degree of RCD at admission, improvement in cognitive function at 1 year occurred in 8 (47%) of patients with 3 points of RCD on admission; 18 (40%) with 4 to 5 points of RCD, and 12 (40%) with 6 or more points of RCD. Thus, each group demonstrates substantial continued improvements in MMSE score over the 1-year follow-up period. Similar trends were demonstrated with the alternative RCD definition of improvement in admission MMSE score by 5 or more points, with continued improvements in MMSE by 1 year in 45% overall.
Table 5.
One-Year Outcomes by Degree of RCD During Hospitalization*
| One-Year Outcome (N = 179) | |||||||
|---|---|---|---|---|---|---|---|
| Degree of RCD by original definition (points) | Improved MMSE n (%) | Unchanged MMSE n (%) | Declined MMSE n (%) | Subtotal n (%) | Missing n | Dead n | Total n |
| 3 | 8 (47) | 5 (29) | 4 (24) | 17 (100) | 8 | 6 | 31 |
| 4 to 5 | 18 (40) | 12 (27) | 15 (33) | 45 (100) | 21 | 15 | 81 |
| ≥6 | 12 (40) | 4 (13) | 14 (47) | 30 (100) | 18 | 19 | 67 |
| Total | 38 | 21 | 33 | 92 | 47 | 40 | 179 |
| One-Year Outcome (N = 79) | |||||||
|---|---|---|---|---|---|---|---|
| Degree of RCD, alternative definition (points) | Improved MMSE n (%) | Unchanged MMSE n (%) | Declined MMSE n (%) | Subtotal n (%) | Missing n | Dead n | Total n |
| 5 | 4 (57) | 0 | 3 (43) | 7 (100) | 8 | 6 | 21 |
| ≥6 | 11 (42) | 4 (15) | 11 (42) | 26 (100) | 16 | 16 | 58 |
| Total | 15 | 4 | 14 | 33 | 24 | 22 | 79 |
RCD=recoverable cognitive dysfunction (Original definition = 3 or more points improvement in admission MMSE; Alternative definition = 5 or more points improvement in admission MMSE. See text for details.); MMSE, Mini-Mental State Examination; n = number of patients.
The 1-year mortality rates for RCD patients are considerable. Overall 40 of 179 (22%) patients with RCD at baseline died by 1 year, with mortality rates ranging from 6 (19%) in the group with 3 points of RCD at admission, 15 (19%) in the group with 4 to 5 points of RCD, to 19 (28%) with 6 or more points of RCD. Recoverable cognitive dysfunction did predict 1-year mortality, and the ordinal relationship specified (see “Methods”) did demonstrate a significant mortality trend (ptrend=0.0032) as hypothesized. In multivariable analyses, controlling for age, ADL score, and APACHE II score, the adjusted odds ratio associated with 1-year mortality for the RCD group (compared with the nonimpaired group) was 1.82 (95% confidence interval [95% CI] 1.03, 3.20). Similar results were demonstrated with the alternative RCD definition (5 or more point change), with an adjusted odds ratio associated with 1-year mortality for the RCD group (compared with the nonimpaired group) of 2.05 (95% CI 1.15, 3.65). Thus, findings for 1-year outcomes were robust across varying definitions of RCD.
Notably, 47 of 179 (26%) patients were missing MMSE scores at 1 year. The reasons for the missing MMSE scores were: incomplete MMSE (n=8); refusal of follow-up interview (n=13), illness-related factors (n=10), communication difficulties precluding telephone interview (n=13, e.g., severe deafness in 7, severe cognitive impairment in 5, or language barrier in 1), and nursing home placement (n=3). As a sensitivity analysis, if all the patients with missing values were added to the “Declined MMSE” category, then the overall rate of improvement would decrease to 38 of 139 (27%) and the rate of decline would increase to 80 of 139 (58%).
DISCUSSION
Acute illness can represent a life-altering event for an older person, yet the impact of acute illness on cognitive functioning has not been systematically examined. This prospective cohort study documents the striking degree of a novel clinical phenomenon, RCD, occurring in 39% of the older hospitalized persons in our study, a rate substantially higher than in previous studies. Importantly, our study documents the high prevalence of depressed cognitive functioning on hospital admission with continued improvements in a considerable proportion of patients over time. The vast majority of cases of RCD (80%) occurred in patients who did not meet criteria for either full or partial delirium at baseline. Although dementia represents a risk factor, 81% of cases of RCD occurred in patients without evidence of dementia. Thus, RCD in the face of acute illness in older persons represents a frequent occurrence which has not been well-described previously, and which extends beyond our current conceptualization of delirium and dementia. In addition, RCD is a strong independent predictor of 1-year mortality, with an adjusted odds ratio of 1.82 (95% CI 1.03 to 3.20) compared with the group with no cognitive impairment.
We identified 3 independent predictors for RCD in multivariable analysis after controlling for baseline MMSE score: higher educational level, increased preadmission functional (ADL) impairment, and higher illness severity (APACHE II). The latter 2 factors are supported by previous studies; that is, sicker patients with functional impairment would be most likely to demonstrate RCD during hospitalization. The relationship with educational level is worthy of note. Although patients with higher educational level tended to have higher MMSE scores at baseline, they also demonstrated higher rates of RCD during hospitalization. This finding may be due to having “more to lose,” but may also reflect the resiliency and improved cognitive reserve capacity associated with higher educational level.32,33
Strengths of this study include the daily assessment of cognitive function with standardized-validated instruments, which allowed us to discover the reversible nature of cognitive impairment and to correlate the findings with the presence of delirium and dementia. The prospective design with longitudinal follow-up represents another strength. The blinding of the interviewers to the study hypotheses minimized bias in data collection. Detailed assessment of patient characteristics facilitated elucidation of cogent predictors. Proxy interviews allowed us to determine baseline dementia status on all patients, as well as to determine the status of patients lost to 1-year follow-up. Finally, validating the 1-year outcomes with an alternative definition of RCD demonstrated the robustness of the results.
Several caveats about this study deserve comment. First, a learning effect on the MMSE might have contributed to the results. However, we do not believe that learning effect played a major role in our findings for several reasons. We failed to demonstrate a substantial learning effect in our previous studies of acutely ill hospitalized persons with daily MMSE testing,13,34 and the medical literature documents that the effect is generally modest, usually 1 to 2 points at maximum14,26—rather than up to 13 points as demonstrated in our study. Moreover, the learning effects would be short-term, and would not be expected to persist or increase over 1-year follow-up as demonstrated in our study. Second, we were not able to obtain Diagnostic and Statistical Manual-based psychiatric diagnoses for delirium and dementia in this large-scale epidemiologic study. While this would have been ideal, we did use instruments which are well validated and widely used for identification of delirium and dementia. Third, we found considerable losses to follow-up at 1 year, as expected in a study involving a frail older population. However, these losses do not invalidate our findings of a substantial proportion of patients with improvements in MMSE at 1 year. Sensitivity analysis which included all of the losses to follow-up in the worsened MMSE group (see “Results”) still demonstrated a substantial degree of improvement at 1 year. Our definition of RCD is based on the admission MMSE score; it is possible that additional cases of RCD develop after hospital admission and would not be captured by the current definition. Thus, our results may represent conservative estimates of this phenomenon. Finally, this study was based on a sample which was representative of all older persons hospitalized at the institution, including 15% nonwhite and 14% with low socioeconomic status. Given that the findings are from a single site, they will need to be validated in other populations. The potential lack of generalizability, however, does not compromise the internal validity of the findings or the description of this new phenomenon.
Given its high prevalence, all acutely ill older adults should be considered at risk for RCD, and thus, formal cognitive screening procedures (such as the MMSE and CAM) should be routinely implemented and preventive interventions initiated in all older patients upon hospital admission. The high overall 1-year mortality rate observed with RCD and its independent association with 1-year mortality suggest that, like delirium, this condition may be a marker for poor cognitive reserve capacity and holds substantive prognostic implications. While the cases of RCD in our study may represent subsyndromal delirium,35,36 as defined by criteria distinct from those used for full and partial delirium in our study, the high prevalence of this condition in older hospitalized persons suggests that reevaluation of our conceptualization of reversible cognitive disorders may be required with extension to include this new phenomenon. Cognitive impairment is a costly problem; a previous study has estimated an annual cost of $2,000 US (1995 dollars)37 per patient for each 1-point decrease in MMSE score. Strategies to prevent and ameliorate RCD (such as avoidance of psychoactive medications, reorientation procedures, and therapeutic activities) are clinically indicated. In addition, assurance of independence in basic and instrumental activities of daily living is indicated before discharge to ensure safe discharge to the home environment. Future research will be imperative to test effective intervention strategies for RCD. Moreover, this study raises concerns about the validity of diagnosing dementia in the face of acute illness or hospitalization in older persons. Consideration should be given to raising this issue as a stronger precaution in the current diagnostic criteria for dementia.38–40 Thus, our findings hold substantial implications from both clinical and health policy perspectives.
Acknowledgments
The authors thank the patients and family members at Yale New Haven Hospital who participated in the study and Project Recovery research staff at the Yale Program on Aging who carried out the interviews and medical record abstractions. We also thank Ms. Patty Fugal and Ms. Sarah Dowal for assistance with manuscript preparation. This work is dedicated to Benjamin and Jordan Helfand.
Data integrity: Drs. Inouye and Zhang have had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Grant support: In part by grants #R21AG025193 and #K24AG00949 (Dr. Inouye) from the National Institute on Aging and by in-kind support from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG21342). The funders played no role in the design or conduct of this study, or in the collection, management, analysis, and interpretation of the data, or in preparation, review, or approval of this manuscript.
REFERENCES
- 1.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–8. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 2.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–23. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 3.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK. Current concepts: delirium in older persons. N Engl J Med. 2006;354:1157–65. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 5.Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12:7–21. [PubMed] [Google Scholar]
- 6.Meagher DJ. Delirium: optimising management. BMJ. 2001;322:144–9. doi: 10.1136/bmj.322.7279.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fields SD, MacKenzie CR, Charlson ME, Sax FL. Cognitive impairment: can it predict the course of hospitalized patients? J Am Geriatr Soc. 1986;34:579–85. doi: 10.1111/j.1532-5415.1986.tb05763.x. [DOI] [PubMed] [Google Scholar]
- 8.Hickey A, Clinch D, Groarke EP. Prevalence of cognitive impairment in the hospitalized elderly. Int J Geriatr Psychiatry. 1997;12:27–33. doi: 10.1002/(sici)1099-1166(199701)12:1<27::aid-gps446>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 9.Fields SD, MacKenzie CR, Charlson ME, Perry SW. Reversibility of cognitive impairment in medical inpatients. Arch Intern Med. 1986;146:1593–6. [PubMed] [Google Scholar]
- 10.Treloar AJ, Macdonald AJD. Outcome of delirium, Part I: outcome of delirium diagnosed by DSM-III-R, ICD-10 and CAMDEX and derivation of the reversible cognitive dysfunction scale among acute geriatric inpatients. Int J Geriatr Psychiatry. 1997;12:609–13. doi: 10.1002/(sici)1099-1166(199706)12:6<609::aid-gps553>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 11.Treloar AJ, Macdonald AJF. Outcome of delirium, Part II: clinical features of reversible cognitive dysfunction. Are they the same as accepted definitions of delirium? Int J Geriatr Psychiatry. 1997;12:614–8. doi: 10.1002/(sici)1099-1166(199706)12:6<614::aid-gps1553>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 12.Cassel EJ, Leon AC, Kaufman SG. Preliminary evidence of impaired thinking in sick patients. Ann Intern Med. 2001;134:1120–3. doi: 10.7326/0003-4819-134-12-200106190-00012. [DOI] [PubMed] [Google Scholar]
- 13.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–76. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. The Folstein Mini-Mental State Examination: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 15.Cummings JL. Clinical Neuropsychiatry. Orlando: Grune and Stratton; 1985. p. 9. [Google Scholar]
- 16.Inouye SK, Van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 17.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL, a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 18.Cornoni-Huntley J, Brock DB, Ostfeld AM, Taylor JO, Wallace RB. Bethesda: NIH publication no. 86-2443. National Institute on Aging; 1986. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. [Google Scholar]
- 19.MacPhee GJ, Crowther JA, McAlpine CH. A simple screening test for hearing impairment in elderly patients. Age Ageing. 1988;17:347–51. doi: 10.1093/ageing/17.5.347. [DOI] [PubMed] [Google Scholar]
- 20.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 23.Uhlmann RF, Larson EB, Buchner DM. Correlations of Mini-Mental State and Modified Dementia Rating Scale to measures of transitional health status in dementia. J Gerontol. 1987;42:33–6. doi: 10.1093/geronj/42.1.33. [DOI] [PubMed] [Google Scholar]
- 24.Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Validation of a telephone version of the Mini-Mental State Examination. J Am Geriatr Soc. 1992;40:697–702. doi: 10.1111/j.1532-5415.1992.tb01962.x. [DOI] [PubMed] [Google Scholar]
- 25.Anthony JC, LeResche L, Niaz U, Von Korff MR, Folstein MF. Limits of the ‘Mini-Mental State’ as a screening test for dementia and delirium among hospital patients. Psychol Med. 1982;12:397–408. doi: 10.1017/s0033291700046730. [DOI] [PubMed] [Google Scholar]
- 26.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–35. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 27.Van Belle G, Uhlmann RF, Hughes JP, Larson EB. Reliability of estimates of changes in mental status test performance in senile dementia of the Alzheimer type. J Clin Epidemiol. 1990;43:589–95. doi: 10.1016/0895-4356(90)90163-j. [DOI] [PubMed] [Google Scholar]
- 28.Salmon DP, Thal LJ, Butters N, Heindel WC. Longitudinal evaluation of dementia of the Alzheimer type: a comparison of 3 standardized mental status examinations. Neurology. 1990;40:1225–30. doi: 10.1212/wnl.40.8.1225. [DOI] [PubMed] [Google Scholar]
- 29.Stockton P, Cohen-Mansfield J, Billig N. Mental status change in older surgical patients. Am J Geriatr Psychiatry. 2000;8:40–6. doi: 10.1097/00019442-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Inouye SK, Robison JT, Froehlich TE, Richardson ED. The Time and Change Test: a simple screening test for dementia. J Gerontol A Biol Sci Med Sci. 1998;53A:M281–M286. doi: 10.1093/gerona/53a.4.m281. [DOI] [PubMed] [Google Scholar]
- 31.Froehlich TE, Robison JT, Inouye SK. Screening for dementia in the outpatient setting: the time and change test. J Am Geriatr Soc. 1998;46:1506–11. doi: 10.1111/j.1532-5415.1998.tb01534.x. [DOI] [PubMed] [Google Scholar]
- 32.Le Carret N, Lafont S, Letenneur L, Dartigues JF, Mayo W, Fabrigoule C. The effect of education on cognitive performances and its implication for the constitution of the cognitive reserve. Dev Neuropsychol. 2003;23:317–37. doi: 10.1207/S15326942DN2303_1. [DOI] [PubMed] [Google Scholar]
- 33.Liao YC, Liu RS, Teng EL, et al. Cognitive reserve: a SPECT study of 132 Alzheimer's disease patients with an education range of 0–19 years. Dement Geriatr Cogn Disord. 2005;20:8–14. doi: 10.1159/000085068. [DOI] [PubMed] [Google Scholar]
- 34.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons: predictive model and inter-relationship with baseline vulnerability. JAMA. 1996;275:852–7. [PubMed] [Google Scholar]
- 35.Cole M, McCusker J, Dendukuri N, Han L. The prognostic significance of subsyndromal delirium in elderly medical inpatients. J Am Geriatr Soc. 2003;51:754–60. doi: 10.1046/j.1365-2389.2003.51255.x. [DOI] [PubMed] [Google Scholar]
- 36.Levkoff SE, Liptzin B, Cleary P, et al. Subsyndromal delirium. Am J Geriatr Psychiatry. 1996;4:320–9. doi: 10.1097/00019442-199622440-00006. [DOI] [PubMed] [Google Scholar]
- 37.Jönsson L, Lindgren P, Wimo A, Jönsson B, Winblad B. Costs of Mini-Mental State Examination-related cognitive impairment. Pharmacoeconomics. 1999;16:409–16. doi: 10.2165/00019053-199916040-00008. [DOI] [PubMed] [Google Scholar]
- 38.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–44. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. Geneva: World Health Organization; 1992. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research; pp. F00–F09. [Google Scholar]
- 40.American Psychiatric Association. four. Washington, DC: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders; pp. 133–55. [Google Scholar]