Figure 2.
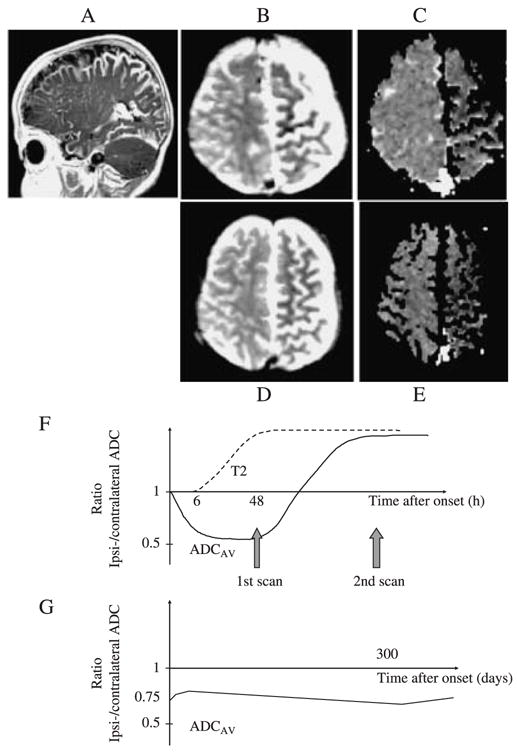
This patient was born with a left capillary haemangioma in the V1–2 distribution and demonstration of a pial angioma confirmed the diagnosis of Sturge-Weber syndrome. She presented at age 4 months with 6 days of frequent treatment-resistant seizures lasting up to 2 hours. T2-weighted imaging (B) and diffusion imaging (C) were performed 6, 12 and 25 days after initial presentation. The apparent diffusion coefficient (ADC) maps obtained at 6 days after initial onset of the seizures showed evidence of ongoing restricted diffusion throughout a substantial part of the abnormal left hemisphere (C). Representative regions showed an ipsi/contralateral ADC ratio of 0.79 (shown graphically in G, compared with values of the order of 0.5 in the first 48 hours in a child with a stroke and 1.0 in controls, shown graphically in F). The ADC remained low in the affected areas at 12 and 25 days after presentation (shown graphically in G, ipsi/contralateral ADC ratio 0.81 and 0.84 respectively). Throughout this period, the T2-weighted images showed hypointensity in corresponding regions. The patient developed a right hemiparesis and chronic epilepsy. A sleep study showed mean and minimum oxyhaemoglobin saturation (SpO2) of 95.8% and 91% respectively (97% is the 5th percentile in normal children; Urschitz et al., 2003). A follow-up scan was performed at the age of 14 months (D, E); the ADC remained low with an ipsi/contralateral ADC ratio of 0.79 (shown graphically in G). At the age of 15 months, her development was delayed to the 10-month level. Persistently low ADC, suggesting ongoing ischaemia, was again demonstrated on MR scans at 16 (G) and 30 months. The patient underwent a hemispherectomy for intractable epilepsy at the age of 33 months and has remained seizure-free post-operatively. It is possible that chronic exposure to mild overnight hypoxaemia had a deleterious effect on brain tissue compromised by chronic venous hypertension and ischaemia.
