Figure 3.
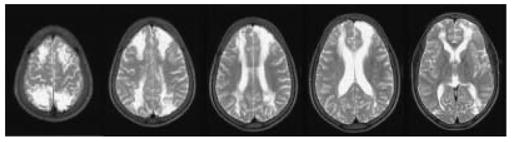
This 8-year-old boy (Patient 1, Tables 2 and 3), one of twins, had uncomplicated sickle cell disease (SCD) but at the age of 6 years, had overnight pulse oximetry classified prospectively as normal (Kirkham et al., 2001) although the mean was less than the 5th percentile for age (Urschitz et al., 2003). His twin developed conditionally high internal carotid/middle cerebral artery velocities on transcranial Doppler (TCD) (maximum 192 cm/sec at the age of 8) but has not had a neurological event over follow-up of 13 years. This patient’s TCD remained normal (maximum 144 cm/sec at the age of 8) but 2 months after this recording, he developed seizures and coma after surgery to drain a painful swelling of his left cheek, associated with fever, after a fall. Preoperative preparation had included hydration and blood transfusion to achieve a haemoglobin of 11.9 g/dl and haemoglobin S of 36% and blood pressure was above 110/50 mmHg (mean arterial blood pressure, MAP 70 mmHg) pre- and post-operatively even after the onset of coma. Intracranial pressure (ICP) was not measured. Initial T2-weighted MRI showed acute infarction with increased signal and swelling in both anterior arterial borderzones and the right posterior arterial borderzone, with mature infarction at follow-up as shown in the figure. TCD, Magnetic Resonance, including arteriography and venography, and four vessel cerebral angiography were normal. Motor function recovered completely. Psychometry showed significant cognitive impairment; compared to premorbid testing full scale IQ was reduced by 30 and performance IQ by 50 points (WISCIII). Covert infarction in the borderzones between the anterior and middle and posterior and middle cerebral arteries are common in SCD, probably because these areas are vulnerable to acute reductions in cerebral blood flow secondary to reduced cerebral perfusion pressure (CPP = MAP − ICP); this patient appears to have had an acute reduction in CPP despite maintenance of blood pressure, perhaps in relation to the cerebral oedema and undiagnosed raised ICP in a child with inadequate preconditioning for the insult experienced and normal cerebral vessels.
