Abstract
Objective:
The aim of this study was to compare the long-term objective and subjective outcomes of laparoscopic and open Nissen fundoplication in a randomized clinical trial with an 11-year follow-up.
Summary Background Data:
Laparoscopic Nissen fundoplication has become the method of choice in antireflux surgery, replacing its open counterpart despite the lack of long-term results from controlled clinical studies.
Methods:
Between April 1992 and June 1995, 110 consecutive patients were randomized to either laparoscopic (LAP) or conventional (open) Nissen fundoplication. The objective long-term follow-up consisted of an upper gastrointestinal endoscopy and a clinical assessment; the subjective long-term outcome was investigated by personal interviews using a structured questionnaire.
Results:
Forty-nine patients in the LAP group and 37 patients in the open group were available for evaluation. Late subjective results, including postoperative symptoms and evaluation of the surgical result, were similar in both groups. With the benefit of hindsight, 73.7% of the patients in the open group and 81.8% in the LAP group would again choose surgical treatment (P = 0.3042). In the LAP group, there were 5 (13.2%) partially or totally disrupted plications compared with the 14 (40.0%) disrupted plications in the open group (P = 0.0152). There were 10 incisional hernias in the open group compared with none in the LAP group (P < 0.001).
Conclusions:
At long-term follow-up, the open and LAP approaches for the Nissen fundoplication have similar long-term subjective symptomatic outcome despite the significantly higher incidence of incisional hernias and defective fundic wraps at endoscopy in the open group defining laparoscopic Nissen fundoplication as the procedure of choice in surgical management of gastroesophageal reflux disease.
This randomized study compared the long-term objective and subjective outcomes of laparoscopic and open Nissen fundoplication with an 11-year follow-up. Both approaches for the Nissen fundoplication have similar long-term subjective symptomatic outcome despite the significantly higher incidence of incisional hernias and defective fundic wraps at endoscopy in the open group.
To date, laparoscopic fundoplication is generally accepted as a routine surgical approach in the treatment of moderate or severe gastroesophageal reflux disease. In a review by Catarci et al,1 laparoscopic fundoplication was as effective as its open counterpart with reduced morbidity, shorter hospital stay, and recovery but without any significant differences in early functional results and outcome. However, there are only few randomized studies comparing the laparoscopic and open approach for Nissen fundoplication2–13 and only 2 studies9,14 have published a follow-up of 5 years after surgery. So far, there have been no reports of randomized studies with follow-up exceeding 10 years after this procedure. In this study, we compared the long-term results of laparoscopic (LAP) and open Nissen fundoplication at a mean follow-up of 11 years and 5 months after surgery.
PATIENTS AND METHODS
Patients and Operations
Between April 1992 and June 1995, 110 consecutive patients were randomized to either LAP or conventional (open) Nissen fundoplication, 55 to each procedure. The clinical details of the patients enrolled in the study, the methods, and the operative techniques have previously been described in detail.2 This study was a review of late results after a randomized clinical trial.
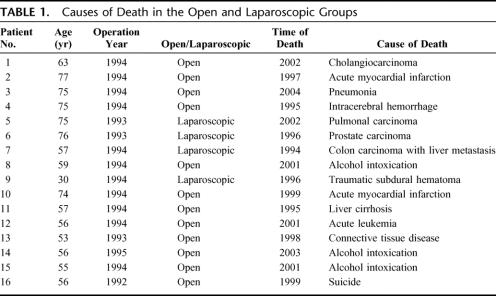
Of the original patient series, 94 patients were available for long-term follow-up. Sixteen patients died of unrelated causes: 12 in the open group and 4 in the LAP group. The causes of death are detailed in Table 1. One patient in the open group underwent refundoplication during the original study period due to a disrupted plication; the late outcome was thus excluded from this study, but the refundoplication was included in the reoperation rate analysis. In addition, 3 patients were excluded from the long-term follow-up based on their current medical condition: 1 for disseminated ovarian cancer, 1 for metastasized renal cancer, and 1 for severe dementia. Of the remaining 90 patients, 86 patients (95.6%) were available for long-term follow-up: 37 open group patients and 49 LAP group patients, including 4 conversions to open surgery. A total of 75 patients (83.3%) underwent both the upper gastrointestinal endoscopy and the symptomatic outcome interview: 35 in the open group and 40 in the LAP group. Informed consent was obtained from all the patients. The additional 11 patients underwent a personal phone interview by the same researcher using the same structured questionnaire; the response rate was thus 95.6% at a median follow-up of 11 years and 5 months. The researcher (P.T.P.S.) collecting and analyzing the results was independent of the surgical team and she (P.T.P.S.) also performed 93.3% (n = 70) of all clinical examinations and endoscopies. Five endoscopies were performed by 4 other surgeons; 2 due to local arrangements concerning endoscopies needing sedation, 2 due to a patient's choice and one due to a recent endoscopy just before initiation of this study. The mean age of the patients at follow-up was 60 years (range, 38–87 years), 50 men (58.1%) and 36 women (41.9%). Both these patient characteristics and the mean follow-up were comparable in both groups.
TABLE 1. Causes of Death in the Open and Laparoscopic Groups
In this study, we primarily compared the patients in a per-protocol analysis to better detect and elucidate possible differences between laparoscopic and open approach for a Nissen fundoplication; the 4 conversions were excluded from this analysis, leaving a total of 82 patients: 38 in the open group and 44 in the LAP group. Of these 82 patients, 3 open group patients and 6 LAP group patients underwent only the phone interview. A total of 73 upper gastrointestinal endoscopies were included in the per-protocol analysis. Of these 73 patients, 38 were LAP group and 35 were open group patients. Patients and results were also compared in a separate intention-to-treat analysis, including the 4 conversions to laparotomy in the LAP group; the results of the intention-to-treat analysis did not differ from the per-protocol analysis results.
Senior surgeons performed both the laparoscopic and open operations. In the initial patient series, all of the laparoscopic procedures were performed by the same senior surgeon (J.T.O.) with a personal laparoscopic fundoplication experience of 20 procedures before the initiation of this randomized study. This surgeon (J.T.O.) also operated 11 of the patients in the open group of this follow-up patient series. Of the remaining 26 open group patients, 13 patients were operated on by another senior surgeon (A.P.T.R.) and the other 13 open procedures were performed by 6 senior surgeons (5, 1, 2, 1, 3, and 1 operations per surgeon).
Follow-up
The objective long-term follow-up consisted of an upper gastrointestinal endoscopy, a clinical examination of possible incisional hernias, and an evaluation of the need for further examinations. The presence of esophagitis, Barrett esophagus, hiatal hernia, and the endoscopic appearance of the plication and lower esophageal sphincter (LES) was noted. Esophagitis was evaluated by the Los Angeles classification.15 The diagnosis of Barrett esophagus was confirmed by histology in all cases. The state of the fundic wrap was evaluated at retroflexed endoscopy and was assessed normal when a 270° elevated fold resembling an inverted cone was present (Fig. 1). The plication was evaluated disrupted when no folds or only loose distorted loose folds were visible (Fig. 2). In addition to the researcher's evaluation of the plication, all of the plications were documented by print photography during endoscopy. These photos were then used to achieve a second opinion on the plication appearances by another experienced surgeon. This second evaluation was done independent of the researcher with similar plication assessment results; all of the disrupted plications were also rated disrupted in this second analysis.
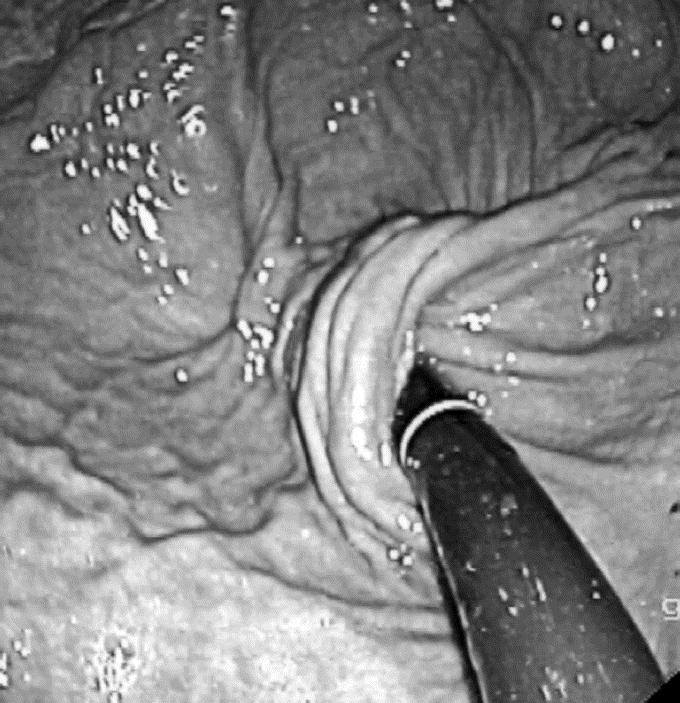
FIGURE 1. Normal plication at endoscopy.
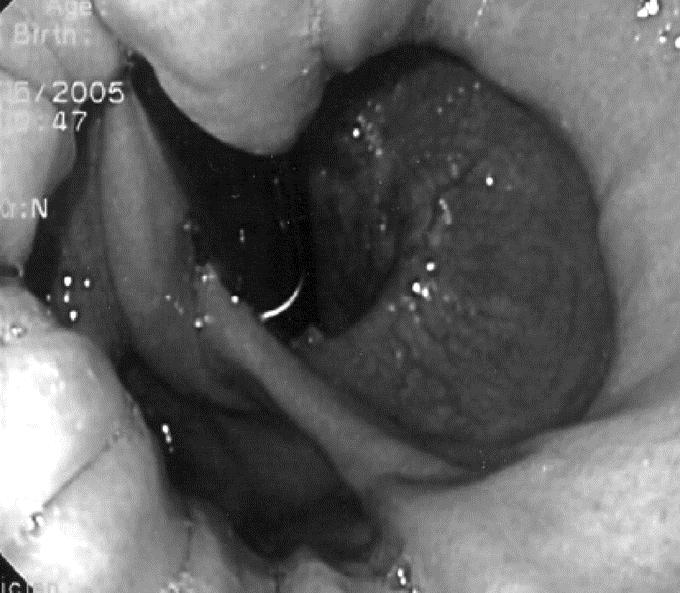
FIGURE 2. A partially disrupted plication and a hiatal hernia.
The long-term subjective symptomatic outcome was investigated by personal interviews using a structured questionnaire. Patients were asked to grade their postoperative symptoms on a scale ranging from 1 (being absent) to 5 (having severe symptoms). In the questionnaire, even the slightest symptoms were taken into account; but it was only the difficult and severe symptoms that had an impact on the patients' everyday life. The following symptoms were asked: heartburn, regurgitation and upper abdominal pain, dysphagia, and bloating or increased flatulence. The patients were also asked to rate the result of their surgery and to state whether they would still prefer surgery to medication as the optimal treatment of their gastroesophageal reflux disease. Information on the use of acid suppression medications after antireflux surgery was acquired. The possible operative procedures (dilatations and reoperations) were registered from the hospital records.
When comparing categorical variables between surgical approaches, χ2 was used. In case of low frequencies, Fisher exact test was applied. T test was used to compare age and follow-up time between open and LAP groups. P values less than 0.05 were considered significant. The statistical analyses were carried out using SAS/STAT software, version 9.1.3 SP3 of the SAS System for Windows.
RESULTS
Upper Gastrointestinal Endoscopy
The group-specific endoscopic findings are shown in detail in Table 2. In the whole study group, 4 patients (5.5%) had esophagitis at endoscopy; all of them were grade A esophagitis and none of these patients used proton pump inhibitors (PPIs) at the time of endoscopy. Barrett esophagus was noted in 8 patients; in 3 patients, the condition was already previously noted and the only long-segment Barrett esophagus was one of these patients. New-onset Barrett esophagus was discovered in 5 patients: 4 in the LAP group and one in the open group. All of these LAP group patients had a very-short-segment Barrett esophagus with an intact plication without esophagitis at endoscopy. The one open group patient with a 4-cm-long Barrett esophagus had a disrupted wrap and grade A esophagitis. The appearance of LES was evaluated normal in 61 patients (83.6%) and loose in 11 patients (15.1%); all of the patients in the latter category had a disrupted plication. In addition, one patient (1.3%) had a relative esophageal stricture at the LES level due to recurrent reflux resulting from a disrupted plication. Hiatal hernia was noted in 23 patients (31.5%). In the whole study group, there were 3 ventricular ulcers and one duodenal ulcer; all but one of these patients were asymptomatic. Helicobacter pylori was detected in 14 patients; 2 of the ventricular ulcer patients were Helicobacter pylori-positive.
TABLE 2. Group-Specific Endoscopic Findings
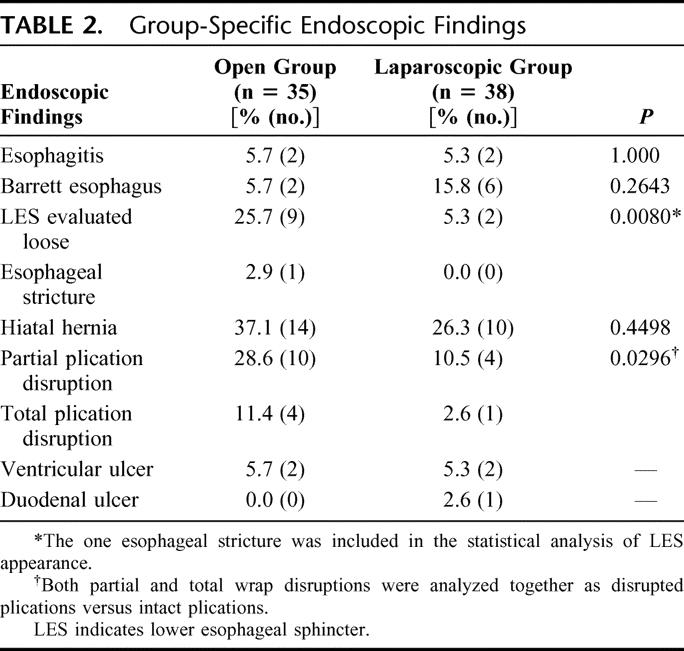
At follow-up endoscopy, 14 of 35 (40.0%) fundic wraps were defective in the open group. Of these 14 plications, 10 were evaluated partially disrupted and in the remaining 4 patients there were no plication folds visible. Correspondingly in the LAP group 5 of 38 (13.2%) plications were defective: one totally disrupted wrap and 4 partially disrupted plications (P = 0.0152). Four of these patients (5.5%) had esophagitis at follow-up endoscopy: 2 patients in both groups. The remaining 15 of 19 patients with disrupted plications presented no esophagitis, but 10 of these 15 patients used PPI at the time of follow-up endoscopy. Compared with patients with an intact plication, the incidence of esophagitis was significantly higher with a defective plication (P = 0.0032). There was no correlation between the use of antireflux medication and fundoplication failure; 52.6% of the patients with a disrupted wrap had reinstated the medication compared with 35.7% of the patients with an intact plication (P = 0.2785); 26.3% (n = 5) of the patients with a defective wrap complained of difficult or severe upper abdominal symptoms, 21.1% (n = 4) had moderate symptoms and 52.6% (n = 10) presented no or only mild symptoms. In patients with an intact fundoplication wrap, these percentages were 16.7% (n = 9), 7.4% (n = 4), and 76.8% (n = 41), respectively.
Incisional Hernias
A careful clinical examination of incisional hernias was conducted during the outpatient visit; none of the patients had undergone hernia repair prior to this study period. None of the patients in the LAP group had incisional hernias. Ten patients (28.6%) in the open group had an incisional hernia (P < 0.001), but all of them were yet small and asymptomatic and thus none of them were referred to surgery at this point.
Reoperations and Dilatations
Three patients in the open group needed a refundoplication: 2 due to a disrupted plication and one due the dysphagia based on a distorted plication. There was one reoperation in the LAP group due to a problematic ventricle retention suspected to result from a vagus nerve lesion; this patient underwent a successful gastrojejunostomy. In addition, there were 2 LAP group patients that needed one to 2 dilatations due to dysphagia.
Subjective Symptomatic Outcome
Figures 3 to 5 show the group-specific results on a 5-point scale; the occurrence percentages are quite similar in both groups. In the whole study group, 73.2% (n = 60) of the patients had no or only mild upper abdominal symptoms, including heartburn or regurgitation; 9.8% of the patients (n = 8) had moderate symptoms and 17.0% of the patients (n = 14) suffered from difficult upper abdominal symptoms; 83.0% (n = 68) of the patients had no significant dysphagia postoperatively, 13.4% (n = 11) had occasional difficulties with swallowing and 3.6% (n = 3) had difficult or severe dysphagia. Bloating and the presence of increased passage of flatus were the most common postoperative complaint; 45.1% (n = 37) of the patients reported the severity of this symptom to be clearly disturbing, 19.5% (n = 16) had moderate symptoms, and 35.4% (n = 29) reported of absent or only mild symptoms.
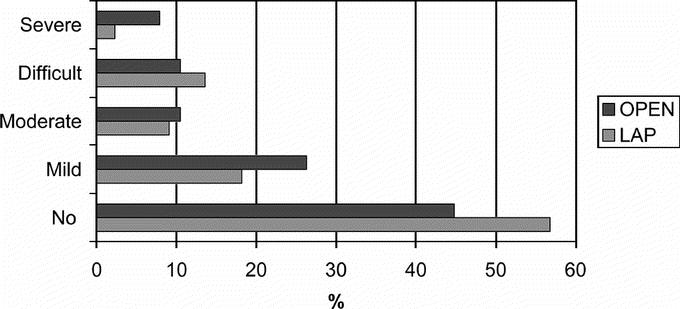
FIGURE 3. Late subjective results of heartburn and regurgitation. P = 0.6241.
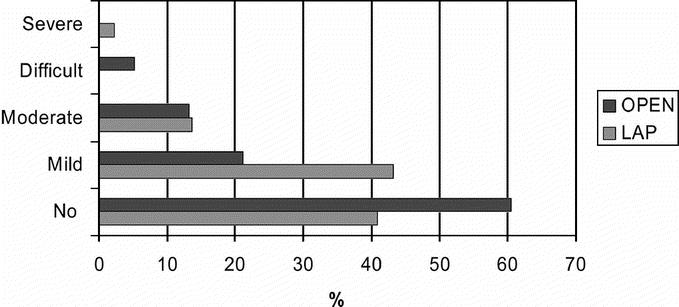
FIGURE 4. Late subjective results of dysphagia. P = 0.0682.
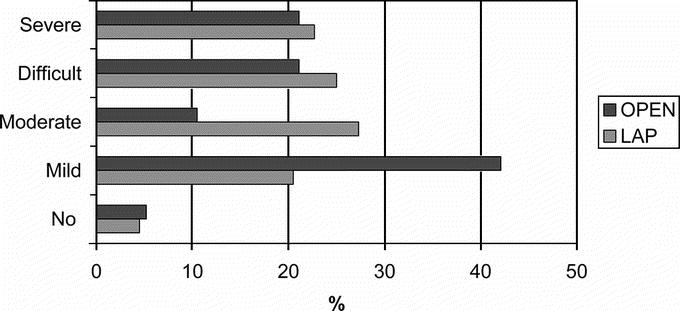
FIGURE 5. Late subjective results of bloating and flatulence. P = 0.1734.
The patients were also given a 5-point scale to evaluate the result of their surgery, ranging from the result being excellent to a poor result; and the group-specific evaluations are shown in Figure 6. In the whole study group, 85.4% (n = 70) of the patients rated their surgical result to be excellent, good, or satisfactory; 14.6% (n = 12) of the patients felt that their surgical result was only fair or poor; 73.7% (n = 28) of the patients in the open group and 81.8% (n = 36) in the LAP group would still choose surgery; 7.9% (n = 3) of the patients in the open group would abstain from surgery and 18.4% (n = 7) of the patients in this group were hesitant of their choice; these percentages were 11.4% (n = 5) and 6.8% (n = 3) in the LAP group.
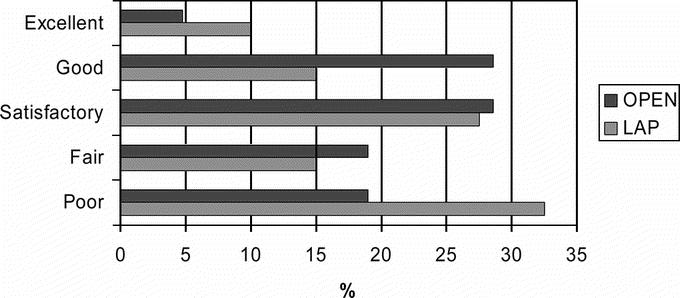
FIGURE 6. Subjective results of the evaluation of the surgical result. P = 0.7361.
A total of 39.5% (n = 15) of the patients in the open group and 40.9% (n = 18) of the patients in the LAP group had started taking acid suppression medications postoperatively (P = 1.0000). In both groups, the majority of these patients used PPIs; 33.3% (n = 5) of these patients in the open group and 26.3% (n = 5) in the LAP group needed medication on a daily basis (P = 0.4027); for the rest of the patients, the need for acid suppression medication was only occasional.
DISCUSSION
Laparoscopic fundoplication is shown to be as effective as its open counterpart with reduced morbidity, shorter hospital stay, and recovery but without any significant differences in early functional results and short-term outcome.1 However, so far, there are only 2 randomized studies comparing the laparoscopic and open approach for Nissen fundoplication with a 5-year-follow-up9,14 and long-term follow-up of randomized trials exceeding this has not yet been published. In this study, we compared the long-term results of laparoscopic and open Nissen fundoplication at a mean follow-up of 11 years and 5 months after surgery.
In this study, we tried to minimize the risk of bias associated with the researcher being part of the surgical team by having an independent surgeon performing the follow-up. The additional strong elements of this present study include the long mean follow-up and the high attendance rate regarding endoscopies and personal interviews. The potential subjectivity of postoperative upper gastrointestinal endoscopy was minimized both by using a single independent researcher performing most of the endoscopies and by photographing all of the endoscopic findings for an additional blinded evaluation of the plication by another surgeon experienced in the field.
A distinct disadvantage of this present study is the lack of preoperative symptom scores because in recent years both dysphagia and bloating have increasingly been considered to be related to gastroesophageal reflux disease itself, instead of occurring as postoperative side effects.16,17 This study was initiated in the early 1990s, and at that time the more objective validated scoring systems for measuring health-related quality of life had not yet become a standard.
In this study, no statistically significant differences were found between the LAP and open group patients in long-term subjective outcomes such as heartburn and regurgitation, dysphagia, bloating and increased flatulence, patient satisfaction, and preference to surgical treatment. Some randomized studies comparing laparoscopic and open fundoplication have shown somewhat higher incidence of dysphagia in laparoscopically operated patients.3,4,7,10,12 Bais et al5 reported a significantly higher incidence of dysphagia in the laparoscopic arm in a multicenter trial, which was stopped at interterm analysis due to this dysphagia incidence. However, in their recently published long-term follow-up evaluation of this prematurely terminated randomized trial, Draaisma et al14 found no differences between the subjective and objective results of laparoscopic and conventional Nissen fundoplication. Other randomized studies also reported similar postoperative dysphagia incidences in both laparoscopic and open approaches.11,13 In the long-term follow-up results of Nilsson et al,9 there were also no differences in postoperative dysphagia between the 2 groups in comparison to the somewhat higher incidence of mild dysphagia in their laparoscopic group at 6 months after surgery.7 As previously reported in our initial study,2 there was no difference in the amount of dysphagia between the LAP and open groups at 3 or 12 months after surgery; and correspondingly in this study, the postoperative dysphagia rate was similar in both groups.
The number of partially or totally disrupted plications was significantly higher (P = 0.0152) in the open group; 14 of 35 plications (40.0%) were defective compared with 5 of 38 plications (13.2%) in the LAP group. Franzén et al18 reported the durability of open partial fundoplication exceeding 90% using patient satisfaction as a definition for durability of the surgical procedure with a follow-up of 10 years. Rantanen et al19 reported 37% endoscopically documented defective plications at 6.5 years after open fundoplication in a community hospital. In a study by Luostarinen,20 109 patients treated with open Nissen fundoplication underwent endoscopy at 6 years after surgery; endoscopy showed 24 defective wraps (22.9%). One of the weaknesses in our study is the number of surgeons in the open group compared with one surgeon performing all of the operations in the LAP group; and this might have an effect on the higher incidence of defective wraps in the open group. On the other hand, of the 14 patients with defective plications in the open group, 2 patients were asymptomatic, 5 had occasional symptoms, 3 had moderate symptoms, and only 4 suffered from difficult or severe heartburn and regurgitation affecting daily life. Despite the objective plication failure rate of 40% in the open group, only 18.4% of the open group patients regarded their surgical result only fair or poor and 73.7% would again choose surgery. This constitutes discrepancies between subjective symptomatic outcome and objective endoscopic findings in the present study as previously found by other studies.20
In this study, approximately 40% of the patients had reinstated acid suppression medication postoperatively; 39.5% (n = 15) in the open group and 40.9% (n = 18) in the LAP group. However, it has to be taken into account that the use of antireflux medication following antireflux surgery does not necessarily correspond to a failure of the surgical procedure. A significant proportion of these patients are treated for undifferentiated and vague abdominal or chest symptoms.21 Despite the symptomatic failure of surgical therapy in these patients using antireflux medications postoperatively, only a small proportion of the patients have abnormal distal esophageal acid exposure on 24-hour pH monitoring.14,22 Nevertheless, this suggests that patients considering antireflux surgery should not be guaranteed a postoperative life without the need for antisecretory medications.
At long-term follow-up, the open and laparoscopic approaches for the Nissen fundoplication have similar long-term subjective symptomatic outcome; there was virtually no difference in terms of clinical outcome between the groups despite the significantly higher incidence of incisional hernias and defective fundic wraps at endoscopy in the open group. The most important long-term quality measurement is indeed the patients' subjective symptomatic outcome due to gastroesophageal reflux disease being a benign functional disorder. However, the objective endoscopic findings of defective plication rates of 40.0% (open) and 13.1% (LAP) somewhat question the durability of the procedure at long-term follow-up, and this suggests that patients considering antireflux surgery should not be guaranteed a permanent relief of reflux symptoms or a postoperative life without the need for antisecretory medications. This emphasizes the importance of adequate preoperative information and appropriate patient selection in securing good outcomes and long-term patient satisfaction.
CONCLUSION
At long-term follow-up, laparoscopic Nissen fundoplication is as safe and effective as its open counterpart and is associated with significantly fewer defective plications and incisional hernias. It should thus be considered as the procedure of choice in surgical management of gastroesophageal reflux disease.
Footnotes
Supported by a research grant from the Department of Surgery, Turku University Central Hospital.
Reprints will not be available from the author.
Correspondence: Paulina Salminen, MD, Kiinamyllynkatu 4-8, 20520 Turku, Finland. E-mail: paulina.salminen@tyks.fi.
REFERENCES
- 1.Catarci M, Gentileschi P, Papi C, et al. Evidence-based appraisal of antireflux fundoplication. Ann Surg. 2004;239:325–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laine S, Rantala A, Gullichsen R, et al. Laparoscopic vs conventional Nissen fundoplication: a prospective randomized study. Surg Endosc. 1997;11:441–444. [DOI] [PubMed] [Google Scholar]
- 3.Heikkinen TJ, Haukipuro K, Koivukangas P, et al. Comparison of costs between laparoscopic and open Nissen fundoplication: a prospective randomized study with a 3-month followup. J Am Coll Surg. 1999;188:368–376. [DOI] [PubMed] [Google Scholar]
- 4.Heikkinen TJ, Haukipuro K, Bringman S, et al. Comparison of laparoscopic and open Nissen fundoplication 2 years after operation: a prospective randomized trial. Surg Endosc. 2000;14:1019–1023. [DOI] [PubMed] [Google Scholar]
- 5.Bais JE, Bartelsman JF, Bonjer HJ, et al. Laparoscopic or conventional Nissen fundoplication for gastro-oesophageal reflux disease: randomised clinical trial. The Netherlands Antireflux Surgery Study Group. Lancet. 2000;355:170–174. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson G, Larsson S, Johnsson F. Randomized clinical trial of laparoscopic versus open fundoplication: blind evaluation of recovery and discharge period. Br J Surg. 2000;87:873–878. [DOI] [PubMed] [Google Scholar]
- 7.Wenner J, Nilsson G, Oberg S, et al. Short-term outcome after laparoscopic and open 360 degrees fundoplication: a prospective randomized trial. Surg Endosc. 2001;15:1124–1128. [DOI] [PubMed] [Google Scholar]
- 8.Nilsson G, Larsson S, Johnsson F. Randomized clinical trial of laparoscopic versus open fundoplication: evaluation of psychological well-being and changes in everyday life from a patient perspective. Scand J Gastroenterol. 2002;37:385–391. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson G, Wenner J, Larsson S, et al. Randomized clinical trial of laparoscopic versus open fundoplication for gastro-oesophageal reflux. Br J Surg. 2004;91:552–559. [DOI] [PubMed] [Google Scholar]
- 10.Luostarinen M, Virtanen J, Koskinen M, et al. Dysphagia and oesophageal clearance after laparoscopic versus open Nissen fundoplication: a randomized, prospective trial. Scand J Gastroenterol. 2001;36:565–571. [DOI] [PubMed] [Google Scholar]
- 11.Chrysos E, Tsiaoussis J, Athanasakis E, et al. Laparoscopic vs open approach for Nissen fundoplication: a comparative study. Surg Endosc. 2002;16:1679–1684. [DOI] [PubMed] [Google Scholar]
- 12.Franzen T, Anderberg B, Wiren M, et al. Long-term outcome is worse after laparoscopic than after conventional Nissen fundoplication. Scand J Gastroenterol. 2005;40:1261–1268. [DOI] [PubMed] [Google Scholar]
- 13.Ackroyd R, Watson DI, Majeed AW, et al. Randomized clinical trial of laparoscopic versus open fundoplication for gastro-oesophageal reflux disease. Br J Surg. 2004;91:975–982. [DOI] [PubMed] [Google Scholar]
- 14.Draaisma WA, Rijnhart-de Jong HG, Broeders IA, et al. Five-year subjective and objective results of laparoscopic and conventional Nissen fundoplication: a randomized trial. Ann Surg. 2006;244:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong D, Bennett JR, Blum AL, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85–92. [DOI] [PubMed] [Google Scholar]
- 16.Wetscher GJ, Glaser K, Gadenstaetter M, et al. The effect of medical therapy and antireflux surgery on dysphagia in patients with gastroesophageal reflux disease without esophageal stricture. Am J Surg. 1999;177:189–192. [DOI] [PubMed] [Google Scholar]
- 17.Anvari M, Allen C. Postprandial bloating after laparoscopic Nissen fundoplication. Can J Surg. 2001;44:440–444. [PMC free article] [PubMed] [Google Scholar]
- 18.Franzen T, Bostrom J, Tibbling Grahn L, et al. Prospective study of symptoms and gastro-oesophageal reflux 10 years after posterior partial fundoplication. Br J Surg. 1999;86:956–960. [DOI] [PubMed] [Google Scholar]
- 19.Rantanen TK, Halme TV, Luostarinen ME, et al. The long term results of open antireflux surgery in a community-based health care center. Am J Gastroenterol. 1999;94:1777–1781. [DOI] [PubMed] [Google Scholar]
- 20.Luostarinen M. Nissen fundoplication for reflux esophagitis: long-term clinical and endoscopic results in 109 of 127 consecutive patients. Ann Surg. 1993;217:329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bammer T, Hinder RA, Klaus A, et al. Five- to eight-year outcome of the first laparoscopic Nissen fundoplications. J Gastrointest Surg. 2001;5:42–48. [DOI] [PubMed] [Google Scholar]
- 22.Lord RV, Kaminski A, Oberg S, et al. Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg. 2002;6:3–9; discussion 10. [DOI] [PubMed]