SYNOPSIS
Objective.
Ischemic heart disease (IHD) is one of the most common health threats to the adult population of the U.S. and other countries. The objective of this study was to examine the association between exposure to elevated annual average levels of Particulate matter 2.5 (PM2.5) air quality index (AQI) and IHD in the general population.
Methods.
We combined data from the Behavioral Risk Factor Surveillance System and the U.S Environmental Protection Agency air quality database. We analyzed the data using SUDAAN software to adjust the effects of sampling bias, weights, and design effects.
Results.
The prevalence of IHD was 9.6% among respondents who were exposed to an annual average level of PM2.5 AQI >60 compared with 5.9% among respondents exposed to an annual average PM2.5 AQI ≤60. The respondents with higher levels of PM2.5 AQI exposure were more likely to have IHD (adjusted odds ratio = 1.72, 95% confidence interval 1.11, 2.66) than respondents with lower levels of exposure after adjusting for age, gender, race/ethnicity, education, smoking, body mass index, diabetes, hypertension, and hypercholesterolemia.
Conclusions.
Our study suggested that exposure to relatively higher levels of average annual PM2.5 AQI may increase the likelihood of IHD. In addition to encouraging health-related behavioral changes to reduce IHD, efforts should also focus on implementing appropriate measures to reduce exposure to unhealthy AQI levels.
Ischemic heart disease (IHD) is one of the most common health threats to the adult population of the U.S. and many other countries. It is a condition in which heart muscle is damaged or works inefficiently because of an absence or relative deficiency of its blood supply; most often caused by atherosclerosis, it includes angina pectoris, acute myocardial infarction, chronic IHD, and sudden death. Age, gender, race, education, diabetes, smoking, diet, hypertension, and serum cholesterol level are important IHD risk factors.1–8
Particulate matter 2.5 (PM2.5) are well-known criteria pollutants that pose a risk to public health.9–11 Studies have shown that ambient air pollution is associated with increased risk of respiratory disease and cardiovascular disease (CVD) mortality.12–14 However, research literature does not show a consistency in the association between PM2.5 and IHD.15–17 Most of the previous studies focused on short-term exposure; that is, exposure that lasted only hours or days.15,17,18 In addition, some of the studies did not adjust the confounding effects of other risk factors. Moreover, most of the studies were hospital-based and did not represent the general U.S. population.
The purpose of this study was to examine the association between PM2.5 and IHD in the general U.S. population while adjusting for potential covariates. We used data from a state-based survey, the Behavioral Risk Factor Surveillance System (BRFSS), and from the U.S. Environmental Protection Agency (EPA) 2001 air quality data.
METHODS
Survey data collection
The BRFSS19 is a standardized, state-based telephone survey system designed to collect data on the health behaviors and health conditions of noninstitutionalized adults aged 18 years and older. Data are collected by state health departments with assistance from the U.S. Centers for Disease Control and Prevention (CDC). All BRFSS questions and methods are available at www.cdc.gov/brfss.
In 2001, 20 states participated in the CVD module used in the survey. The question asked was, “Has a doctor, nurse, or other health professional ever told you that you had any of the following? (1) A heart attack, also called myocardial infarction; (2) angina or coronary heart disease.” We defined IHD as a “yes” response to either of the questions.
Environmental data
The PM2.5 air quality index (AQI) data are based on the EPA's Air Quality System (AQS) database. The database contains measurements of six criteria pollutants at sites in all 50 states. Ambient air measurements collected from a network of national, state, and local air monitoring stations were used to calculate the AQI. According to the EPA, the highest individual pollutant AQI for each area was reported as the daily AQI, and the pollutant corresponding to the highest daily AQI was identified. Because our study focused on PM2.5, we used the daily AQI, which reported daily air quality based on the concentration levels of PM2.5. The daily PM2.5 AQI represented the highest concentrations of PM2.5 for that day.
As part of increasing the utility of BRFSS data, we merged data from the AQS with BRFSS data by county. For a county to be included in the analysis, it had to have (1) at least 125 respondents who participated in the CVD module of the survey to ensure a representative sample with a minimum weighting class, and (2) at least 90 days of PM2.5 AQI monitoring to ensure that the annual average PM2.5 AQI was adequately representative. Data from 51 counties in the U.S. were included in our analyses.
Based on EPA air quality standards, the daily AQI scale runs from 0 to 500 and is categorized into six groups based on the pollutant health effects: (1) 0 to 50 = good, (2) 51 to 100 = moderate, (3) 101 to 150 = unhealthy for sensitive groups, (4) 151 to 200 = unhealthy, (5) 201 to 300 = very unhealthy, and (6) 301 to 500 = hazardous. We calculated the mean annual level of PM2.5 AQI by converting the daily concentrations of PM2.5 into AQI scores and then to an annual average AQI level. The formula used for the conversion from daily concentration to AQI is discussed in detail on the EPA's website.20
We categorized the annual mean PM2.5 AQI where we used an annual mean of PM2.5 AQI >50 to examine the association between the prevalence of IHD and the annual mean PM2.5 AQI. In addition, to examine whether the prevalence of IHD increased with the increased level of the annual mean PM2.5 AQI, we repeated the analysis using annual mean levels of >55 and >60. We did not consider using higher annual mean levels because at an annual mean PM2.5 AQI level >60, we had one county with 412 respondents.
We classified respondents into two groups: (1) respondents who lived in counties with an annual mean level of PM2.5 AQI >50 and (2) all respondents who lived in counties with an annual mean level of PM2.5 AQI ≤50. Because at an annual mean PM2.5 AQI >60 the sample size was small and the conversion we did may have introduced bias, we repeated the analysis by calculating the prevalence of IHD and annual mean PM2.5 at county level. We categorized the annual mean PM2.5 AQI into 10th percentile to assess the association between the prevalence of IHD and annual mean PM2.5 by county. In our analysis, we used an annual mean PM2.5 as a categorical variable because EPA air quality data were collected daily, while BRFSS data reflect events that happened in the last 30 days or more. Therefore, using the annual mean can be more reasonable and may possibly reduce bias.
In addition, we examined the seasonal variations of the quarterly PM2.5 AQI and the association between quarterly variation and IHD prevalence. The quarterly data included quarter 1 (January to March), quarter 2 (April to June), quarter 3 (July to September), and quarter 4 (October to December). We used logistic regression analyses to assess the association between the annual mean PM2.5 AQI and IHD while adjusting for covariates including age, gender, race/ethnicity, education, diabetes, body mass index, hypertension, hypercholesterolemia, and smoking. We used statistical analysis package SAS21 and SUDAAN22 for data analysis to account for the complex sampling design.
RESULTS
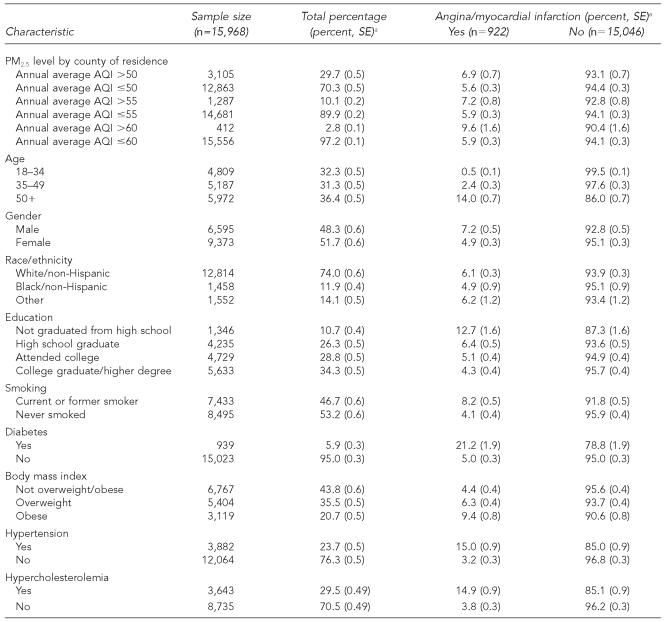
A total of 15,968 respondents participated in the survey in 51 selected U.S. counties during 2001. The age of the respondents ranged from 18–99 (Table 1). The respondents included 48.3% male and 51.7% female; 74.0% white/non-Hispanic; 11.9% black/non-Hispanic; and 14.1% other races/ethnicities, including Asian, Hispanic, other race, and multirace. Of the 15,968 respondents, 922—a prevalence of 6.0%—reported being told by health professionals that they had IHD. The prevalence of IHD was higher among respondents who were aged 50 years or older, male, smokers, and with no high school education. In addition, IHD was higher among respondents with diabetes, hypertension, obesity, and hypercholesterolemia (Table 1).
Table 1.
Distribution of ischemic heart disease by risk factors in 51 counties in the U.S., 2001
Percentage and SE are calculated based on weighted sample using SUDAAN software. [Research Triangle Institute. SUDAAN User's Manual: Release 9.0. Research Triangle Park (NC): Research Triangle Institute; 2005.]
PM2.5 = Particulate matter 2.5
AQI = air quality index
SE = standard error
The prevalence of IHD among respondents exposed to an annual mean PM2.5 AQI >50 was 6.9%. As we increased the cutoff value to >55 and >60, the prevalence of IHD increased to 7.2% and 9.6%, respectively. The prevalence of IHD among respondents exposed to an annual average PM2.5 AQI ≤50, ≤55, and ≤60 remained almost the same at 5.6% to 5.9% (Table 1).
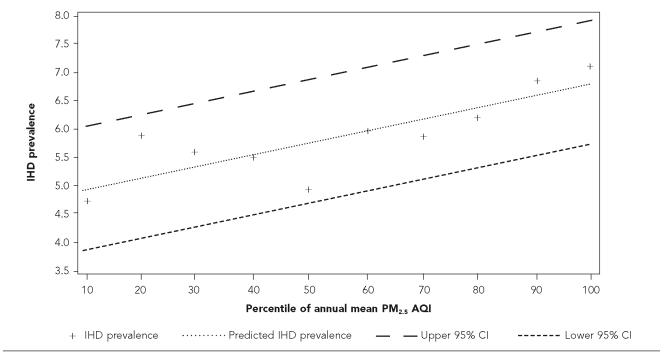
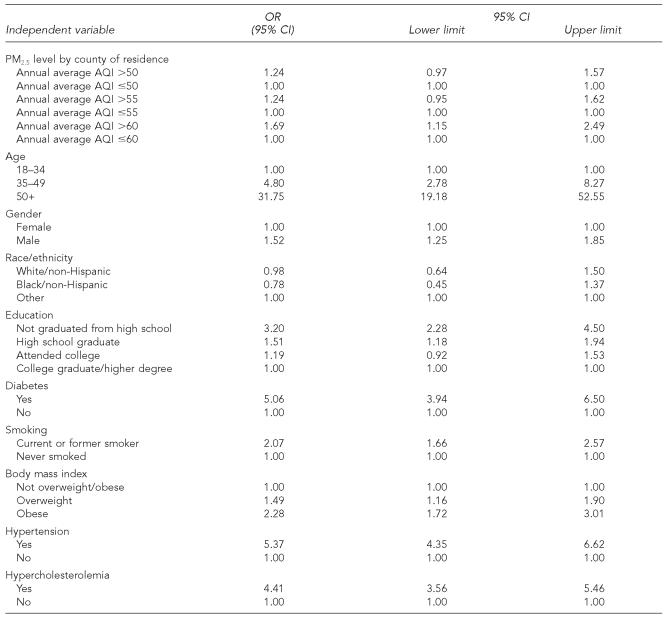
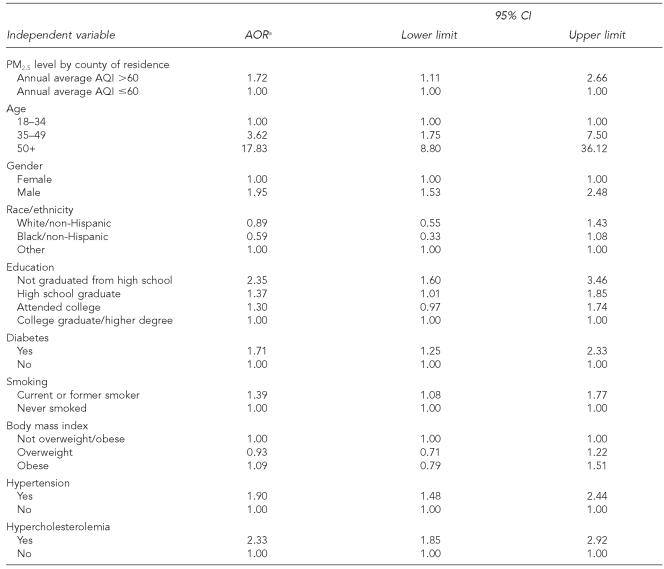
No statistical association was found between the prevalence of IHD and an annual mean level of PM2.5 AQI >50 (odds ratio [OR] =1.24; 95% confidence interval [CI] 0.97, 1.57) or >55 (OR=1.24; 95% CI 0.95, 1.64) before adjusting for covariates (Table 2). However, a statistical association was found between the prevalence of IHD and an annual mean level of PM2.5 AQI >60 both before (OR=1.69; 95% CI 1.15, 2.49) (Table 2) and after adjusting for covariates (adjusted odds ratio [AOR] =1.72, 95% CI 1.11, 2.66) (Table 3). This association persisted when we repeated the analysis using annual mean PM2.5 AQI and prevalence of IHD to build a regression model at county level (p=0.0019). As the annual mean of PM2.5 AQI by county increased, the prevalence of IHD increased (Figure).
Figure.
Association of IHD with PM2.5 air pollution at county level
IHD = ischemic heart disease
PM2.5 = Particulate matter 2.5
AQI = air quality index
CI = confidence interval
The mean quarterly level of PM2.5 AQI was 48.04, 39.33, 42.27, and 39.47 for quarters 1, 2, 3, and 4, respectively. The difference of the quarterly mean was statistically significant (p<0.001); however, no association was found between quarterly variations of the mean levels of PM2.5 AQI and quarterly variations of the prevalence of IHD (data not shown).
An elevated annual mean of PM2.5 AQI >60 was still a significant predictor for IHD even after adjusting for potential covariates. Our findings also demonstrated that the prevalence of IHD was independently associated with known risk factors such as age, gender, level of education, diabetes, hypertension, hypercholesterolemia, and smoking (Table 3).
DISCUSSION
To our knowledge, this study was the first to combine data from BRFSS and the EPA AQI database to examine the association of IHD with PM2.5 among the general U.S. population. Our findings showed that respondents exposed to a higher level of annual mean PM2.5 AQI at individual levels and at county levels were more likely to report IHD than respondents exposed to a lower level of annual mean PM2.5 AQI.
IHD is one of the main manifestations of atherosclerotic coronary artery disease. Numerous clinical and epidemiological studies have shown that age, gender, race, diabetes, smoking, diet, hypertension, and serum cholesterol level are important risk factors.1–7 Studies have also shown that air pollution increases the risk of death from CVD.12–14 The association of IHD with long-term exposure to PM2.5 was robust by an annual mean in our models. This finding was consistent with other studies. Studies by Pope et al.23 demonstrated that long-term PM2.5 exposure was most strongly associated with mortality attributable to IHD, dysrhythmias, heart failure, and cardiac arrest. A study by Schwartz et al.24 found an association of PM2.5 with increased mortality caused by IHD and chronic obstructive pulmonary disease. Pekkanen et al.25 suggested that PM2.5 pollution was associated with cardiovascular morbidity, at least through increased susceptibility to IHD.
The mechanism of induced IHD, including myocardial infarctions, from PM2.5 pollution is not yet clear. However, one short-term study15 suggested that elevated PM2.5 may trigger myocardial infarction possibly because of the association between hemodynamic and hemostatic alterations with particulate matter air pollution. According to Peters et al.26–28 this theory appears to be supported by observations from at least several other studies14,29–32 that found associations of ambient particle pollutions with: (1) increased plasma viscosity,26 (2) acceleration of heart rates and diminished heart rate variability,14,26,31,32 and (3) ventricular fibrillation and increased number of therapeutic interventions in patients with implanted cardioverter-defibrillators.28
Similar to other studies, our findings demonstrate that in addition to an elevated annual mean of PM2.5 AQI being a significant predictor of IHD, age, gender, diabetes, smoking, hypertension, and hypercholesterolemia are important predictors as well.1–6 In addition, a low level of education was a risk factor of IHD, a finding also reported in other studies,4,8 and was strongly associated with overweight/obesity, smoking, diabetes, hypercholesterolemia, and hypertension (data not shown). A plausible explanation for this association could be a lack of access to information on modifying health behaviors or lack of knowledge on how to prevent CVD.
Limitations
Our study had some limitations. Because BRFSS is a telephone survey, people who do not have telephones are excluded, which may result in sampling bias. All data on IHD and risk factors were self-reported and may have been subject to recall bias. We did not have meteorological data or county level measurements of the social ecological data, which could be very important confounders of IHD. Our study was cross-sectional; therefore, we were unable to determine a cause-and-effect relationship. In addition, we could not measure true exposure because data related to factors that could influence true exposure were lacking. Data on number of PM2.5 monitors, location in each county, distance of individual residence and workplace, and indoor exposure were unavailable. Therefore, individuals may have higher or lower exposure. Because our study included only 51 counties, the findings of this study cannot be generalized to all U.S counties. The prevalence of IHD could be underestimated in our study because our survey focused on noninstitutionalized adults.
CONCLUSION
Our findings suggest that exposure to a relatively higher level of annual mean PM2.5 AQI may increase the likelihood of IHD. Although age, gender, hypercholesterolemia, hypertension, diabetes, and education were major covariates, PM2.5 was still a significant predictor. The likelihood of IHD was 1.72 times higher for populations with elevated levels of exposure to PM2.5.
The health effect of PM2.5 air pollution cannot be ignored in the prevention of CVD. Efforts to prevent or reduce IHD should not only focus on encouraging behavioral modification but should also target the implementation of appropriate measures to reduce PM2.5 exposure, especially for susceptible individuals living in areas with a frequent unhealthy level of PM2.5 AQI. Government agencies should continue to implement measures to reduce the PM2.5 air pollution effectively and enforce air quality standards. In addition communities should develop innovative and affordable approaches to improve air quality.
Table 2.
Non-adjusted odds ratio of ischemic heart disease by risk factor in 2001
OR = odds ratio
CI = confidence interval
PM2.5 = Particulate matter 2.5
AQI = air quality index
Table 3.
Adjusted odds ratio of ischemic heart disease (IHD) by risk factor, 2001
AOR of IHD by annual average PM2.5 AQI level, adjusted by age, gender, race, education, diabetes, smoking, body mass index, hypertension, and hypercholesterolemia
AOR = adjusted odds ratio
CI = confidence interval
PM2.5 = Particulate matter 2.5
AQI = air quality index
Acknowledgments
The authors thank the U.S. Environmental Protection Agency for providing air quality data, with special thanks to David Mintz and the Behavioral Risk Factor Surveillance System coordinators for their help in collecting the data used in the analysis.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Yusuf HR, Giles WH, Croft JB, Anda RF, Casper ML. Impact of multiple risk factor profiles on determining cardiovascular disease risk. Prev Med. 1998;27:1–9. doi: 10.1006/pmed.1997.0268. [DOI] [PubMed] [Google Scholar]
- 2.The Pooling Project Research Group. Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. J Chronic Dis. 1978;31:201–306. doi: 10.1016/0021-9681(78)90073-5. [DOI] [PubMed] [Google Scholar]
- 3.Multiple Risk Factor Intervention Trial Research Group. Relationship between baseline risk factors and coronary heart disease and total mortality in the Multiple Risk Factor Intervention Trial. Prev Med. 1986;15:254–73. doi: 10.1016/0091-7435(86)90045-9. [DOI] [PubMed] [Google Scholar]
- 4.Chang M, Hahn RA, Teutsch SM, Hutwagner LC. Multiple risk factors and population attributable risk for ischemic heart disease mortality in the United States, 1971-1992. J Clin Epidemiol. 2001;54:634–44. doi: 10.1016/s0895-4356(00)00343-7. [DOI] [PubMed] [Google Scholar]
- 5.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 6.Wilson PW, D'Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162:1867–72. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- 7.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121:293–8. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- 8.Jacobsen BK, Thelle DS. Risk factors for coronary heart disease and level of education. The Tromso Heart Study. Am J Epidemiol. 1988;127:923–32. doi: 10.1093/oxfordjournals.aje.a114895. [DOI] [PubMed] [Google Scholar]
- 9.Environmental Protection Agency (US) Research Triangle Park (NC): Office of Air Quality Planning and Standards; 1996. Review of the national ambient air quality standards for particular matter; policy assessment of scientific and technical information. [Google Scholar]
- 10.Environmental Protection Agency (US) Research Triangle Park (NC): Office of Air Quality Planning and Standards; 1996. Review of the National Ambient Air Quality Standards for ozone; assessment of scientific and technical information. [Google Scholar]
- 11.Aunan K. Exposure-response functions for health effects of air pollutants based on epidemiological findings. Risk Anal. 1996;16:693–709. doi: 10.1111/j.1539-6924.1996.tb00818.x. [DOI] [PubMed] [Google Scholar]
- 12.Bascom R. Health effects of outdoor air pollution. Am J Respir Crit Care Med. 1996;153:3–50. doi: 10.1164/ajrccm.153.1.8542133. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz J. Particulate air pollution and daily mortality: a synthesis. Public Health Rev. 1991;19:39–60. [PubMed] [Google Scholar]
- 14.Pope CA, III, Dockery DW. Epidemiology of particle effects. In: Holgate ST, Samet JM, Koren HS, Maynard RL, editors. Air pollution and health. San Diego: Academic Press; 1999. pp. 673–705. [Google Scholar]
- 15.Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103:2810–5. doi: 10.1161/01.cir.103.23.2810. [DOI] [PubMed] [Google Scholar]
- 16.Levy D, Sheppard L, Checkoway H, Kaufman J, Lumley T, Koenig J, et al. A case-crossover analysis of particulate matter air pollution and out-of-hospital primary cardiac arrest. Epidemiol. 2001;12:193–9. [PubMed] [Google Scholar]
- 17.Sullivan J, Sheppard L, Schreuder A, Ishikawa N, Siscovick D, Kaufman J. Relation between short-term fine-particulate matter exposure and onset of myocardial infarction. Epidemiology. 2005;16:41–8. doi: 10.1097/01.ede.0000147116.34813.56. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan J, Ishikawa N, Sheppard L, Siscovick D, Checkoway H, Kaufman J. Exposure to ambient fine particulate matter and primary cardiac arrest among persons with and without clinically recognized heart disease. Am J Epidemiol. 2003;157:501–9. doi: 10.1093/aje/kwg015. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (US) National Center for Chronic Disease Prevention and Health Promotion, Behavioral Risk Factor Surveillance System. [cited 2007 Jan 22]. Available from: URL: http://www.cdc.gov/brfss.
- 20.Environmental Protection Agency (US) Guidelines for the reporting of daily air quality—the air quality index (AQI) [cited 2007 Jan 22]. Available from: URL: http://www.epa.gov/ttn/oarpg/t1/memoranda/rg701.pdf.
- 21.SAS Institute. SAS: Version 8.2 for Windows. Cary (NC): SAS Institute; 2005. [Google Scholar]
- 22.Research Triangle Institute. SUDAAN User's Manual: Release 9.0. Research Triangle Park (NC): Research Triangle Institute; 2005. [Google Scholar]
- 23.Pope CA, III, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109:71–7. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specifically with fine particles? J Air Waste Manag Assoc. 1996;46:927–39. [PubMed] [Google Scholar]
- 25.Pekkanen J, Peters A, Hoek G, Tiittanen P, Brunekreef B, de Hartog J, et al. Particulate air pollution and risk of st-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: the exposure and risk assessment for fine and ultrafine particles in ambient air (ULTRA) study. Circulation. 2002;106:933–8. doi: 10.1161/01.cir.0000027561.41736.3c. [DOI] [PubMed] [Google Scholar]
- 26.Peters A, Doring A, Wichmann HE, Koenig W. Increased plasma viscosity during the 1985 air pollution episode: a link to mortality? Lancet. 1997;349:1582–7. doi: 10.1016/S0140-6736(97)01211-7. [DOI] [PubMed] [Google Scholar]
- 27.Peters A, Perz S, Doring A, Stieber J, Koenig W, Wichman HE. Increases in heart rate during an air pollution episode. Am J Epidemiol. 1999;150:1094–8. doi: 10.1093/oxfordjournals.aje.a009934. [DOI] [PubMed] [Google Scholar]
- 28.Peters A, Liu E, Verrier RL, Schwartz J, Gold DR, Mittleman M, et al. Air pollution and incidences of cardiac arrhythmia. Epidemiol. 2000;11:11–7. doi: 10.1097/00001648-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Pope CA, III, Dockery DW, Kanner RE, Villegas GM, Schwartz J. Oxygen saturation, pulse rate, and particulate air pollution: a daily time-series panel study. Am J Respir Crit Care Med. 1999;159:365–72. doi: 10.1164/ajrccm.159.2.9702103. [DOI] [PubMed] [Google Scholar]
- 30.Pope CA, III, Verrier RL, Lovett EG, Larson AC, Raizenne ME, Kanner RE, et al. Heart rate variability associated with particulate air pollution. Am Heart J. 1999;138:890–9. doi: 10.1016/s0002-8703(99)70014-1. [DOI] [PubMed] [Google Scholar]
- 31.Liao D, Creason J, Shy C, Williams R, Watts R, Zweidinger R. Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Environ Health Perspect. 1999;107:521–5. doi: 10.1289/ehp.99107521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gold DR, Litonjua A, Schwartz J, Lovett E, Larson A, Nearing B, et al. Ambient pollution and heart rate variability. Circulation. 2000;101:1267–73. doi: 10.1161/01.cir.101.11.1267. [DOI] [PubMed] [Google Scholar]