Figure 5.
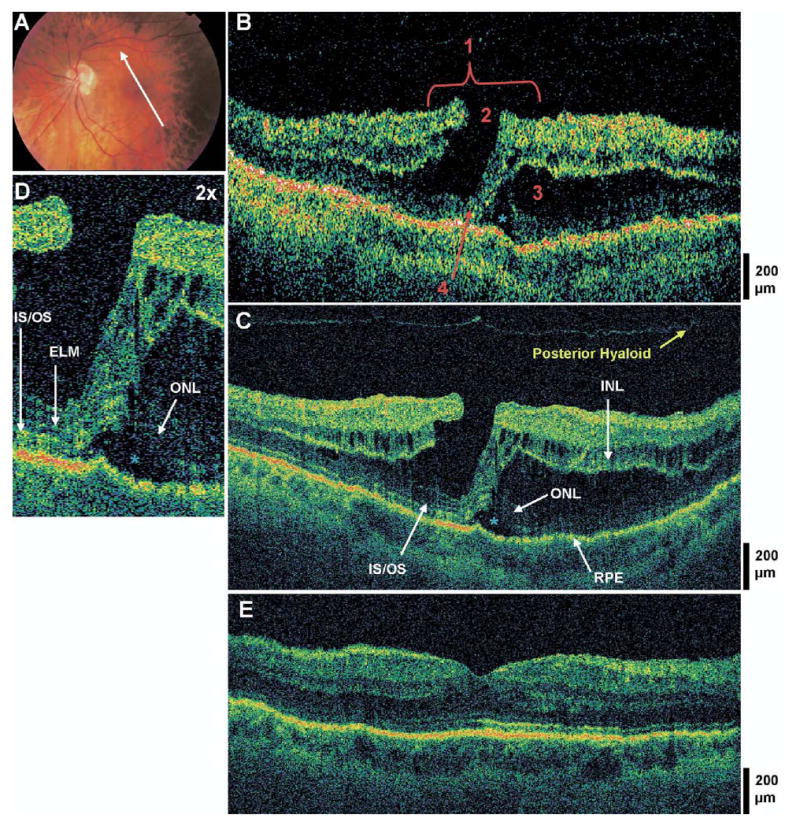
Lamellar hole with photoreceptor disruption and subfoveal fluid. The patient is a 57-year-old myopic woman (−4.75 diopters) who presented with a best-corrected visual acuity (BCVA) of 20/100 in the left eye. Dilated fundus examination revealed a sharply-circumscribed red lesion in the left macula, believed to be a pseudohole. A, Fundus photograph depicting lamellar hole and the direction of optical coherence tomographic (OCT) scans. B, Stratus OCT image meeting all 4 criteria for the diagnosis of lamellar hole, which are labeled as follows: 1, an irregular foveal contour; 2, break in the inner fovea; 3, separation of the inner from the outer foveal retinal layers; and 4, absence of a full thickness foveal defect with intact foveal photoreceptors. A large strand of tissue connects the inner to the outer retina at the fovea. C, The corresponding UHR OCT image, which also shows disruption of the inner/outer segment junction (IS/OS) junction and the external limiting membrane (ELM) at the fovea, but the outer nuclear layer (ONL) remains intact underneath the area of foveal dehiscence. A small pocket of subfoveal fluid is present (blue asterisk). Small cystic spaces are present within the inner nuclear layer (INL). D, Magnification (×2) of UHR OCT image, showing a subretinal fluid pocket and photoreceptor disruption. E, Postoperative UHR OCT image. The patient underwent a pars plana vitrectomy with peeling of the internal limiting membrane (ILM), air/fluid exchange, and sulfur hexafluoride 20% injection. Six months later, the hole was flat and closed on fundus examination and OCT, and BCVA had improved to 20/30 in the left eye.
