Abstract
OBJECTIVE
To understand the flow of family physicians from region to region across Canada. To discover how many leave a region after residency, how many stay, and how many flow into a region from other regions.
DESIGN
Cross-sectional study using descriptive statistics.
SETTING
Various regions across Canada.
PARTICIPANTS
A weighted sample (N = 14 332) of all family physicians who completed the College of Family Physicians of Canada’s 2001 National Family Physician Workforce Survey. This survey asked where physicians had done their family medicine residency.
MAIN OUTCOME MEASURES
The proportion of family physicians whose current region of practice was the same as their place of residency (“staying”), the proportion of family physicians who trained in one region and who now practise in a different region (“outflow”), the proportion of family physicians who practise in a region but were trained in another region (“inflow”), and the number of family physicians flowing in and out of regions.
RESULTS
Half of Canadian family physicians were practising in regions different from the regions where they did their residency programs. This percentage varied by region, however, with only Ontario’s percentage resembling the Canadian figure. In the Atlantic and Prairie regions, few stayed (13.8% and 24.7%, respectively), but many flowed in. In Quebec, a high proportion stayed after residency training (81.6%). In British Columbia, only 23.7% stayed, but many flowed in.
CONCLUSION
This study provides information about the relationship between where family physicians did their residency programs and where they subsequently practised. Our results add important information to the health human resource literature.
RÉSUMÉ
OBJECTIF
Comprendre les déplacements des médecins de famille d’une région du Canada à une autre. Déterminer combien quittent une région après y avoir fait leur résidence, combien y restent et combien migrent dans une région à partir d’une autre région.
TYPE D’ÉTUDE
Étude transversale à l’aide de statistiques descriptives
CONTEXTE
Diverses régions du Canada.
PARTICIPANTS
Échantillon pondéré (n = 14 332) de tous les médecins qui ont répondu au Sondage national auprès des médecins de famille 2001 du Collège des médecins de famille du Canada. On y demandait l’endroit où le médecin avait fait sa résidence enmédecine familiale.
PRINCIPAUX PARAMÈTRES À L'ÉTUDE
Proportion des médecins exerçant maintenant dans la même région que celle de leur résidence («non migrants»), proportion deceux exerçant maintenant dans une région autre que celle de leur résidence («émigrants»), proportion de ceux exerçant maintenant dans une région, mais ayant été formés dans une autre région («immigrants») et nombre de ceux qui passent d'une région à une autre.
RÉSULTATS
La moitié des médecins de famille canadiens pratiquaient dans des régions autres que celle où ils avaient fait leur résidence. Toutefois, ce pourcentage variait d'une région à l'autre, l'Ontario étant la seule province à avoir un pourcentage voisin du pourcentage canadien. Dans les provinces de l'Atlantique et dans les Prairies, les non-migrants étaient peu nombreux (13,8 et 24,7%, respectivement), mais plusieurs avaient immigré dans ces régions. Au Québec, une forte proportion étaient demeurés dans la région de leur résidence (81,6%). En Colombie-Britannique, seulement 23,7% étaient restés, mais plusieurs avaient immigré.
CONCLUSION
Cette étude nous renseigne sur la relation entre l'endroit où un médecin de famille fait sa résidence et celui où il pratique par la suite. Ces résultats constituent un complément d'information majeur à la littérature sur les ressources humaines en santé.
Health human resources is the number 1 issue in Canadian health care today.1 Concerns regarding the shortage of physicians in general and the shortage of family physicians in particular are being raised with increasing frequency. The Romanow Report2 indicated that in Canada, between 1980 and 1993, the number of general practitioners for every 100 000 persons increased from 76.4 to a peak of 101.5. The number decreased in 1999 to 94.0 and has steadily increased since.
These averages tell only part of the story, however. There are substantial differences among the provinces and territories, and some communities lack the requisite number of health professionals to ensure access to even basic health services. As well, the averages do not indicate the age distribution of populations or the demographic and practice characteristics of the physicians. Provincial governments have prepared and commissioned reports and expert panels3–8 and have increased medical school and residency training spaces. In concert with policy initiatives, relevant and timely research helps to set the stage for the future.
Much of the literature on the relationship between location of family medicine residency and location of practice focuses on the role of rural training in increasing the chances that physicians will practise in rural locations.9–12 Two studies in the United States13,14 examining the influence of graduate medical education on region of future practice found that about half the physicians remained in the state where they were trained. The purpose of this secondary analysis of data from the 2001 National Family Physician Workforce Survey (NFPWS) is to try to understand where family physicians in Canada go between the time of residency training and later practice. Health human resource planning by the profession and policy makers can be enhanced by more detailed data on these movements. Young doctors’ migration is not to be considered a problem, but rather a process that needs to be fully understood. The results of this study should be viewed as baseline data for rigorous tracking studies that would follow residency graduates over time.
METHODS
Sample
Information for this cross-sectional study came from the College of Family Physicians of Canada’s NFPWS15 conducted in 2001 as a census survey of all practising family physicians in Canada. Population information was obtained from Table 051–0001 on the Statistics Canada website.16 The 2001 NFPWS questionnaire was developed by a working group of the Janus Project Coordinating Committee who wanted to ensure that data gathered in the 2001 survey would be comparable to that gathered in the 1997–1998 National Family Physician Survey. The committee also wanted the questionnaire to explore new areas of interest. A pilot study was conducted in the summer of 2000, and the resulting recommendations were included in the final version of the questionnaire. National-level estimates based on 2001 NFPWS results are considered accurate to within ± 0.64% 19 times out of 20.
Data and definitions
Items from the self-administered questionnaire that were used for this study are place of residency program (Atlantic—Dalhousie University, Memorial University of Newfoundland; Quebec—Laval University, McGill University, University of Montreal, University of Sherbrooke; Ontario—McMaster University, Queen’s University, University of Ottawa, University of Toronto, University of Western Ontario; Prairies—University of Alberta, University of Calgary, University of Manitoba, University of Saskatchewan; British Columbia—University of British Columbia; Territories—none) and current region of practice (Atlantic—Newfoundland and Labrador, Nova Scotia, Prince Edward Island, New Brunswick; Quebec; Ontario; Prairies—Manitoba, Saskatchewan, Alberta; British Columbia). Omission of the territories and amalgamation of provinces were dictated by small sample size and the need to protect confidentiality.
The variables calculated in this study were as follows.
Staying refers to family physicians whose current region of practice was the same as their place of residency program.
Outflow refers to family physicians who trained in a region and who now practised in a different region.
Inflow refers to family physicians who practised in a region but were trained in another region.
Net gain or loss refers to the number of family physicians trained in a region who were not practising in that region (outflow) minus the number of family physicians trained in other regions who were practising in that region (inflow).
RESULTS
The target population for the 2001 NFPWS was the 25 520 eligible family physicians practising in Canada. Of these, 13 088 completed the questionnaire for a response rate of 51.2%. Analysis of basic demographic characteristics revealed that response rates varied by sex and geographic location (ie, the percentage of men and women and the geographic location of respondents were different from the distribution of these 2 characteristics for the total physician population). To adjust for significant differences in response rates by sex and health region and for nonresponse bias, the data were weighted. These weighting procedures were used to generate estimates for the entire eligible family physician population in Canada (ie, 25 520). Simply stated, about half of Canadian family physicians responded to the survey, and their answers were weighted by sex and geographic location to represent all Canadian physicians.
Of the total weighted sample, 14 332 physicians who indicated where they did their family medicine residency became the sample for this study. The remaining physicians were not included for 1 of the following reasons: they did not answer the question on residency training, they had done a rotating internship rather than a residency, they had trained outside Canada, or they did not answer other questions necessary for analysis. Confirmation that this sample size was a reasonable reflection of the number of family physicians who had completed residency training was established by comparing this number with the number of family medicine residents trained each year as tracked by the Association of Faculties of Medicine in Canada and the Canadian Post-MD Education Registry.
Of the 5 regions of Canada (Atlantic, Quebec, Ontario, Prairies, and British Columbia), Quebec produced the highest percentage of these residency graduates (5121, 35.6%) and British Columbia the lowest (794, 5.5%). The number of residents trained per 10 000 population was 5.71 in the Atlantic region, 6.92 in Quebec, 3.97 in Ontario, 4.63 in the Prairies, and 1.95 in British Columbia.
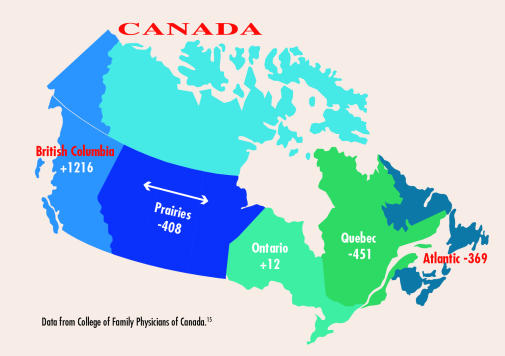
Table 115 shows the staying and outflow proportions in each region. A high of 81.6% of Quebec residents stayed to practise in Quebec, and a low of 13.8% of Atlantic region residents stayed to practise there. Table 2 15 shows the staying and inflow proportions in each region. A high of 90.7% of family physicians practising in British Columbia were trained elsewhere, and a low of 10.4% of family physicians practising in Quebec were trained elsewhere. Figure 115 shows the net gain or loss of residents in numbers rather than percentages in each region. British Columbia had the highest net gain (1216 physicians). Quebec, the Prairies, and the Atlantic region had similar net losses (−451, −408, −369, respectively). Ontario had an almost equal balance of gains and losses.
Table 1.
Family physicians staying and outflow (N =14 332)s
| REGION | TOTAL TRAINED | STAYING N (%) | OUTFLOW N (%) |
|---|---|---|---|
| Atlantic | 1330 | 183 (13.8) | 1147 (86.2) |
| Quebec | 5106 | 4169 (81.6) | 937 (18.4) |
| Ontario | 4702 | 2334 (49.6) | 2368 (50.4) |
| Prairies | 2405 | 595 (24.7) | 1810 (75.3) |
| British Columbia | 789 | 187 (23.7) | 602 (76.3) |
| TOTAL | 14 332 | 7468 (52.1) | 6864 (47.9) |
Data from College of Family Physicians of Canada.15
Table 2.
Family physicians staying and inflow (N =14 332)
| REGION | TOTAL PRACTISING IN REGION | STAYING N (%) | INFLOW N (%) |
|---|---|---|---|
| Atlantic | 961 | 183 (19.0) | 778 (81.0) |
| Quebec | 4655 | 4169 (89.6) | 486 (10.4) |
| Ontario | 4714 | 2334 (49.5) | 2380 (50.5) |
| Prairies | 1997 | 595 (29.8) | 1402 (70.2) |
| British Columbia | 2005 | 187 (9.3) | 1818 (90.7) |
| TOTAL | 14 332 | 7468 (52.1) | 6864 (47.9) |
Data from College of Family Physicians of Canada.15
Figure 1.
Net gain or loss of family medicine residents: Outflow minus inflow.
Data from College of Family Physicians of Canada.15
Analysis of 3 groups of family physicians by years in practice (=10 years, 11 to 20 years, and >20 years) showed generally the same results for staying, inflow, outflow, and net gain or loss, but there were some exceptions. Differences of =5% are noted. No differences in outflow were found between physicians who had been in practice =10 years and those who had been in practice >11 years, except in Ontario where outflow was higher among those who had been in practice for =10 years (55.5% versus 48.6%). Outflow from the Atlantic, Prairies, and British Columbia regions was lower for those in practice =20 years compared with those in practice >20 years (Atlantic—83.8% versus 89.2%; Prairies—72.0% versus 80.5%; British Columbia—66.7% versus 79.1%).
Analysis of 2 groups of family physicians by location of medical school (same region as region of residency and different region from region of residency) gave the same results as the overall group analysis except for Quebec and the Prairies. Differences of =5% are noted. Outflow from the Prairies and Quebec was lower when medical school and residency were in the same region (Quebec—same location, 13.1% outflow, versus different location, 34.8% outflow; Prairies—same location, 72.8% outflow, versus different location, 78.9% outflow).
DISCUSSION
The literature often focuses on the effect of training location (usually defined as urban or rural) on location of practice in urban or rural settings. This study adds to the literature by focusing on region of training and choice of practice location.
What we need, in addition to these data, is a full follow-up cohort tracking study to assess the relative influence of place of early education, medical residency, and other factors on location of practice. What we know from this study is that half of Canadian family physicians were practising in regions different from the regions where they did their residency programs. Inflow and outflow varied by region. The flow of residents into and out of a region was not balanced, except in Ontario. In Ontario, half of the residents trained in Ontario stayed there to practise and half left the province. At the same time, half came into Ontario to practise from other provinces in Canada. In the Atlantic and Prairie regions, a low proportion stayed, but a substantial proportion flowed in; nonetheless, the net result was a loss. In Quebec, a high proportion of family physicians stayed after residency, and a low proportion flowed in, resulting in a net loss. In British Columbia, a low proportion stayed but a high proportion flowed in, resulting in a large net gain.
These results represent a reality that requires health human resource planning. In Ontario, an increase in family medicine resident spaces would yield 50% more doctors for Ontario’s citizens. In all the other regions except Quebec, it would yield a lower percentage increase in doctors. It is often thought that staying in the same region for both medical school and residency increases the chances a practitioner will stay in that region. One study in Virginia found this to be the case.13 Our study showed it was the case only for Quebec and the Prairies.
Limitations
The first limitation concerns the use of weighting in the NFPWS.15 While using population weighting was necessary to adjust the data for differential response by sex and region, using it assumed that the physicians who responded to the survey were in no other ways different from the total population of Canadian family physicians. Other than sex and geographic location, data are unavailable for comparing respondents’ characteristics and practice patterns with those of the total population. Therefore, it is not possible to determine whether survey respondents were different from or similar to physicians who did not respond.
Another limitation is the need to aggregate some provinces into regions because of small sample sizes. It should be noted that there could be variations within these regions that aggregation masks. As well, the data in this study are cross sectional. The physicians were surveyed at one point in time, reflecting only current practice location. It is not possible to track changes over time with cross-sectional data.
Conclusion
Our data suggest that adjustments to residency program numbers at medical school or provincial levels has an effect on the country as a whole because of the movement of graduates from region to region. Health human resource planners need to consider residents’ choice of practice location as a national issue and ensure communication and coordination occurs on a national level.
This study provides information about the effect of family medicine residency location on family physicians’ practice location. Such information adds to the health human resource literature concerning the factors that affect where family physicians choose to practise.
Acknowledgment
The research was conducted at the Thames Valley Family Practice Research Unit, a Health-Systems-linked research unit funded by the Ontario Ministry of Health and Long-Term Care. The views in this paper are those of the authors and do not necessarily reflect the views of the Ministry of Health and Long-Term Care. This report utilizes original data collected for the College of Family Physicians of Canada’s National Family Physician Workforce Database. This database is part of the College of Family Physicians of Canada’s JANUS Project: Family Physicians Meeting the Needs of Tomorrow’s Society. The study was also supported by the Canadian Institute for Health Information, the Canadian Medical Association, La fédération des médecins omnipracticiens du Québec, Health Canada, Scotiabank, Merck Frosst, and the Royal College of Physicians and Surgeons of Canada. The authors thank Sarah Scott, Janus Project Coordinator at the College of Family Physicians of Canada for help with data analysis.
EDITOR’S KEY POINTS
Much of the literature on the relationship between family practice residency location and practice location has focused on the role of rural training. This study provides a snapshot of the flow of family physicians from region to region across Canada.
Half of Canadian family physicians were practising in geographic regions different from those where they did their residency. There is, however, much regional variation. Quebec has the highest percentage of family medicine residents staying in the region.
All regions have a net loss of family medicine residents, except for Ontario and British Columbia. Net gains in British Columbia account for 99% of the net losses from the other regions of Canada.
POINTS DE REPÈRE DU RÉDACTEUR
Une bonne partie de la littérature sur la relation entre le lieu de pratique d'un médecin et celui où il a fait sa résidence a porté sur l'influence des stages en région rurale. Cette étude nous offre une image instantanée des déplacements des médecins de famille entre les régions du Canada.
a moitié des médecins de famille canadiens pratiquaient dans une région géographique différente de celle où ils avaient fait leur résidence. Il y a toutefois beaucoup de différences entre les régions. C'est au Québec qu'on observe le plus fort pourcentage de résidents en médecine familiale qui choisissent de ne pas migrer.
Toutes les régions sauf l'Ontario et la Colombie-Britannique enregistraient une perte nette de résidents en médecine familiale. Les gains nets en Colombie-Britannique représentaient 99% des pertes nettes des autres régions.
Footnotes
This article has been peer reviewed.
Contributors
Ms Ryan and Dr Stewart contributed to study concept and design; data analysis and interpretation; and preparing the article for submission.
Competing interests
None declared
References
- 1.Dault M, Lomas J, Barer M on behalf of the Listening for Direction II partners. Listening for Direction II: national consultation on health services and policy issues for 2004–2007. Ottawa, Ont: Canadian Health Services Research Foundation and Institute of Health Services and Policy Research, Canadian Institutes of Health Research; 2004. [Accessed 2007 January 12]. Available from: http://www.chsrf.ca/other_documents/listening/pdf/LfD_II_Final_Report_e.pdf. [Google Scholar]
- 2.Romanow RJ. Building on values: the future of health care in Canada. Final report. Ottawa, Ont: Commission on the future of Health Care in Canada; 2002. [Accessed 2007 January 12]. Available from: http://www.hc-sc.gc.ca/english/pdf/romanow/pdfs/HCC_Final_Report.pdf. [Google Scholar]
- 3.McKendry R. Physicians for Ontario: Too many? Too few? For 2000 and beyond. Report of the Fact Finder on Physician Resources in Ontario. Toronto, Ont: Ontario Ministry of Health and Long-Term Care; 1999. [Accessed 2007 January 12]. Available from: http://www.health.gov.on.ca/english/public/pub/ministry_reports/mckendry/mckendry.pdf. [Google Scholar]
- 4.Expert Panel on Health Professional Human Resources. Shaping Ontario’s physician workforce. Final report. Toronto, Ont: Ontario Ministry of Health and Long-Term Care; 2001. [Accessed 2007 January 12]. Available from: http://www.health.gov.on.ca/english/public/pub/ministry_reports/workforce/workforce.pdf. [Google Scholar]
- 5.Pagliccia N, Rahim-Jamal S, Reid R, Kazanjian A. Issues in physician resources planning in BC: key determinants of supply and distribution. Update of selected tables using 1998–99 and 1999–00 data. Working paper. Vancouver, BC: Centre for Health Services and Policy Research; 2002. [Accessed 2007 January 12]. Available from: http://www.chspr.ubc.ca/files/publications/2002/hhru02-03W.pdf. [Google Scholar]
- 6.Health Canada. Health human resources: balancing supply and demand. [Accessed 2007 January 12];Health Policy Res Bull. 2004 8:1. Available from: http://www.hc-sc.gc.ca/sr-sr/alt_formats/iacb-dgiac/pdf/pubs/hpr-rps/bull/2004-8-hhr-rhs/2004-8-hhr-rhs_e.pdf.
- 7.Nova Scotia Health. Health human resources action plan. Halifax, NS: Nova Scotia Health; 2005. [Accessed 2007 January 12]. Avaialable from: http://www.gov.ns.ca/heal/downloads/hhr%20action%20plan-full%20book.pdf. [Google Scholar]
- 8.New Brunswick Department of Health. Healthy futures: securing New Brunswick’s health care system. The provincial health plan 2004–2008. Saint John, NB: New Brunswick Department of Health; 2004. [Accessed 2007 March 1]. Available from: http://www.gnb.ca/0051/pdf/healthplan-2004-2008_e.pdf. [Google Scholar]
- 9.Bowman RC, Penrod JD. Family practice residency programs and the graduation of rural family physicians. Fam Med. 1998;30(4):288–92. [PubMed] [Google Scholar]
- 10.Peach HG, Trembath M, Fensling B. A case for more year-long internships outside metropolitan areas? Med J Aust. 2004;180(3):101–2. doi: 10.5694/j.1326-5377.2004.tb05829.x. [DOI] [PubMed] [Google Scholar]
- 11.Pacheco M, Weiss D, Vaillant K, Bachofer S, Garrett B, Dodson WH, III, et al. The impact on rural New Mexico of a family medicine residency. Acad Med. 2005;80(8):715–6. doi: 10.1097/00001888-200508000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Rourke JT, Incitti F, Rourke LL, Kennard M. Relationship between practice location of Ontario family physicians and their rural background or amount of rural medical education experience. Can J Rural Med. 2005;10(4):231–9. [PubMed] [Google Scholar]
- 13.Owen JA, Hayden GF, Bowman RC. Influence of places of birth, medical education, and residency training on the eventual practice location of family physicians: recent experience in Virginia [letter] South Med J. 2005;98(6):674–5. doi: 10.1097/01.SMJ.0000161753.31008.F0. [DOI] [PubMed] [Google Scholar]
- 14.Seifer SD, Vranizan K, Grumbach K. Graduate medical education and physician practice location. Implications for physician workforce policy. JAMA. 1995;274(9):1068–74. [PubMed] [Google Scholar]
- 15.College of Family Physicians of Canada. National Family Physician Workforce Survey 2001. Mississauga, Ont: College of Family Physicians of Canada; 2001. [Accessed 2007 February 15]. Available from: http://www.cfpc.ca/local/files/Programs/Janus%20project/NFPWS2001_Questionnaire_en.pdf. [Google Scholar]
- 16.Statistics Canada. Table 051–0001 Estimates of population, by age and sex, Canada, provinces and territories, annual (persons unless otherwise noted) Ottawa, Ont: Statistics Canada; 2006. [Google Scholar]