Abstract
We describe how connections among nursing home staff impact the care planning process using a complexity science framework. We completed six-month case studies of four nursing homes. Field observations (n = 274), shadowing encounters (n = 69), and in-depth interviews (n = 122) of 390 staff at all levels were conducted. Qualitative analysis produced a conceptual/thematic description and complexity science concepts were used to produce conceptual insights. We observed that greater levels of staff connection were associated with higher care plan specificity and innovation. Connection of the frontline nursing staff was crucial for (1) implementation of the formal care plan and (2) spontaneous informal care planning responsive to changing resident needs. Although regulations could theoretically improve cognitive diversity and information flow in care planning, we observed instances of regulatory oversight resulting in less specific care plans and abandonment of an effective care planning process. Interventions which improve staff connectedness may improve resident outcomes.
Keywords: care plan, case study, complexity science, nursing homes
Care planning is generally considered to be a key activity in the delivery of services to nursing home residents. State regulations describe the care planning process as an “essential” means of ensuring comprehensive, resident-specific care.1 Indeed, the Omnibus Budget Reconciliation Act (OBRA) of 1987 mandated the use of interdisciplinary care planning teams and established a “Minimum Data Set” (MDS) of resident-specific information that must be collected to inform the care planning process.2–4 A new staff position, the “MDS Nurse,” was created to lead the care planning process.5
Despite the emphasis placed on care planning, several studies have raised questions about its effectiveness. First, coordination among interdisciplinary care plan team members appears difficult to achieve, and has not improved following the implementation of the MDS.6,7 Second, several studies have revealed discrepancies between activities recorded in the care plan and actual care delivery.8,9 It appears that the potential impact on improving resident outcomes has not been fully realized.
Complexity science offers a useful lens through which to examine such lapses in coordination and implementation of care planning. Complexity science is the study of how living things behave in complex systems such as nursing homes.10 Complex systems are composed of a large number of people with multiple interactions where order emerges regardless of hierarchical systems of control.11 An individual is “connected” to other people in the system through their relationships and interactions, and the connections influence both the individual and the system as a whole.12 Complexity science suggests that a high density of connections between staff at all levels will permit at least two vital things to occur which will facilitate effective care planning.13,14 First, connection allows resident-specific information to flow freely through the system, and thus, to be available for problem-solving. Second, connection allows staff with different training, experiences, and backgrounds to come together to interpret this information. This “cognitive diversity” will provide a broad and rich interpretation of data.15
When staff interacts freely, sharing new information and their collective cognitive diversity in the process called self-organization, resulting behaviors may be more effective.10,11 In systems where staff members have high-quality relationships with others, good flow of new information, and are able to capitalize on cognitive diversity in problem-solving (effective self-organization), positive outcomes for the organization are more likely to be achieved. On the other hand, when there are barriers to relationships, constraints on new information flow, and where multiple perspectives on an issue are not considered (ineffective self-organization), the outcomes are likely to be poor. In the case of nursing homes, effective self-organization would be expected to result in a care plan that is more innovative, resident-specific, and sensitive to change (Figure 1). It is noteworthy that the OBRA regulations would seem to foster the system parameters of “cognitive diversity” and multiple connections by mandating an interdisciplinary team and “information flow” by creating an MDS.
FIGURE 1.
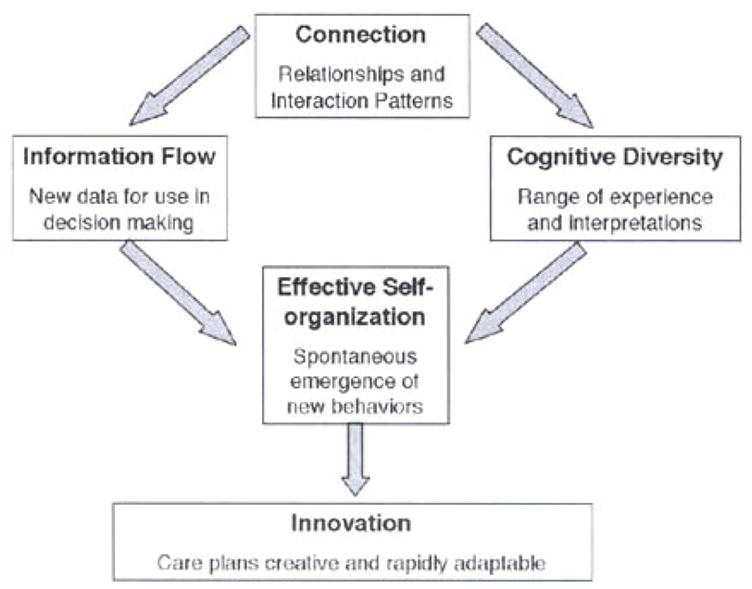
Conceptual Model of how System Parameters Impact Care planning Process
We used data from a multiple case study of nursing home management practices with complexity science as its conceptual model. Using case study methodology, we sought to: (1) describe how different patterns of connection among staff impacted the care planning process with respect to information flow, cognitive diversity, self-organization, and innovation; and (2) to explore how state regulations facilitated or impeded the care planning process.
DESIGN AND METHODS
Four nursing homes, referred to as “Windy Lane,” “Harbor,” “Sweet Dell,” and “Ivy Vines,” were enrolled in a comparative, multiple case study of relationship patterns and management practices. Facilities were located in one of six counties and were selected using a random number generator. Facility administrators agreed to enroll the nursing homes in the case study. Informed consent processes were employed for all individuals interviewed. The university institutional review board approved all study procedures.
SAMPLE AND PROCEDURES
Potentially, all staff members from all departments were included in the study. Overall, 390 staff were directly observed during 274 field observations, which included 69 shadowing encounters and 122 in-depth interviews. Across the four cases, approximately 47 percent of the staff was white and 75 percent was female (Table 1).
Table 1.
Demographic Characteristics of Staff Members Participating in the Case Study
| Sweet Dell (n = 104) | Harbor (n = 119) | Windy Lane (n = 97) | Ivy Vines (n = 82) | |
|---|---|---|---|---|
| Female (%) | 84 | 82 | 79 | 74 |
| White (%) | 60 | 51 | 36 | 39 |
| African American (%) | 36 | 39 | 33 | 46 |
| Other/Unknown (%) | 4 | 10 | 31 | 15 |
| Employed less than 1 year (%) | 16 | 13 | 33 | 20 |
| Employed 5+ years (%) | 32 | 8 | 4 | 23 |
DATA COLLECTION
Two field researchers collected data in each facility over six months. The complexity science framework was used in the study design to focus the observations and interviews on staff interaction patterns and the consequences on the quality of care delivered. The field researchers observed daily routines and meetings, including care planning meetings and processes, primarily on day shift. Researchers also “shadowed” staff from all levels and disciplines during a typical day (n = 69), including usual members of the care plan team (MDS Nurse, Social Workers [SWsJ, Activities Directors, Dietary Directors, Nursing Staff). Depth interviews with key informants from all disciplines were completed (n = 122), and included probes on how information was gathered, how people were involved in care planning, and care plan implementation. Floor nurses and Certified Nursing Assistants (CNAs) were interviewed to obtain diverse perspectives. Detailed field notes were transcribed after each field observation. All interviews were taped and transcribed verbatim.
Reliability and validity were sought by conducting interviews with a wide range of staff until no new themes emerged (theme saturation). Data triangulation included data collected from observation, interviews, and documents.16 At the end of each case study, a summary of our findings was presented to the participants as both an individual and organizational “member check.”17
ANALYSIS
Using an open coding technique, at least two team members coded each document. Emerging themes were discussed at weekly research team meetings. Field researchers provided immediate feedback and were then asked to seek additional data that substantiated or refuted the theme. The coded data related to care planning processes and outcomes were then analyzed using meaning condensation to create a “Conceptual/Thematic Description.” This type of analysis uses imported concepts or themes to reframe a phenomenon (the care planning process).12,18 In addition, “connection maps” were created by the research team during data analysis retreats at the close of each case study. These maps were drawn from the direct observations as well as staff reports of their patterns of information exchange and the nature of their relationships.
Case study summaries, describing the care planning process in each facility with interpretation using the guiding framework, were reviewed independently by team members who identified both missing themes and themes not adequately supported by the data. Throughout the analysis process, we reread the original text to ensure that our results were supported in context of the whole field note or interview.
FINDINGS
Four distinct patterns of staff connection were observed as shown in Figure 2. The findings below describe the nature of these connections and potential consequences for innovation in care planning. Work titles that would identity an individual staff member in the nursing home are replaced with “care plan team member,” indicating a member of the formal care plan team; “frontline nursing staff,” indicating nurses working directly with residents; “nurse manager,” indicating an RN-level nurse with supervisory responsibilities; or “interdisciplinary team member,” indicating a nonnursing discipline (e.g., social work, physical therapy, activities, medical practitioner) who is not a member of the formal care team.
FIGURE 2.
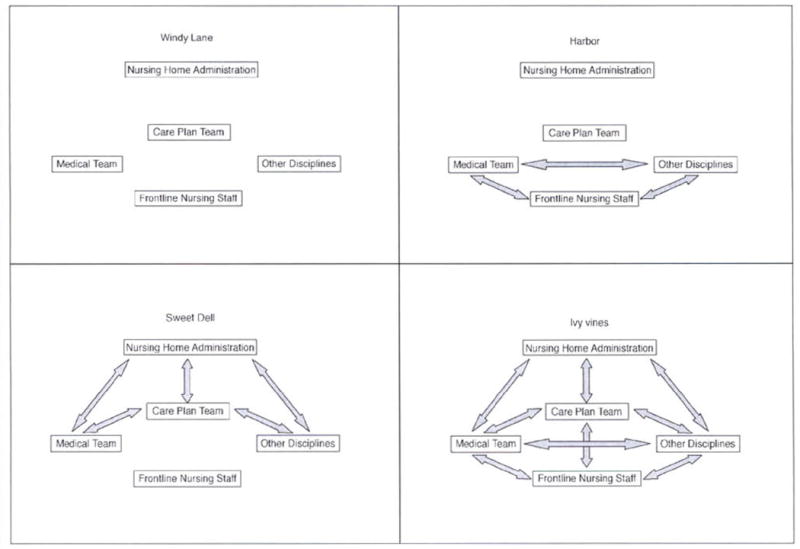
Connection Maps for the four Study Facilities. “Other Disciplines” Includes Rehabilitation, Dietary, Social Work, and Activities Staff. “Medical Team” Includes Attending Physicians, Psychiatrists, and Nurse Practitioners. “Care Plan Team” Includes MDS Nurses and any Other Team Members Assigned in That Facility, Often Social Work and Activities. “Frontline Nursing Staff” Includes floor Nurses (Generally LPNs) And CNAs. Arrows Between Boxes Indicate Connection, Information Flow, and Cognitive Diversity Between Group Members
WINDY LANE
Windy Lane experienced, extraordinary turnover through the case study period. In six months, the facility employed four Directors of Nursing (DONs), three Nursing Home Administrators (NHAs), and four mid-level manager positions. High turnover was evident among frontline caregivers [Licensed Practical Nurses (LPNs) and CNAs] as well.
Field note: LPN was giving two weeks notice and resigning effective April 8th. She said she wanted to… ”go somewhere where I’m more appreciated.” DON said this was the fourth resignation this week.
The absence of consistent leadership contributed to an isolating work environment, where staff just “did their job” but were unsure of expectations. They hoped that changing rules would not get them into trouble with the next supervisor.
LPN: Without us having a DON, it’s like when you were in high school and you had a substitute teacher… I just do it the best I can…
There were few connections within frontline staff or between the frontline staff and the care planning team, perhaps as a result of the high turnover and isolating work environment (Figure 2).
Researcher: Who are the main people that do the care planning? LPN: The [Care plan] lady, I don’t know her name… Researcher: How do they communicate the care plan back to you? LPN: That is the [problem], communicating that is not good. I don’t think I have gotten any messages from the [care plan team member] since I have been working here.
In this setting of turnover and thin connections between staff, the initially functioning care planning process at Windy Lane fell apart entirely. The care plan team members began to fill out their sections independently with the sole intent to fulfill regulatory obligations. They recognized that this was not optimal.
Field note: [Care plan team member] is now typing into the Care Plan section of the database. She says that right now, she’s just doing a “canned care plan.” It is better if it is resident-specific, but she’s just trying to get things done and she will therefore use the “canned” options that are offered [by the computer program] as responses to various flag issues. As she starts working with them, she comments, “These are terrible.”
There was no evidence that the care plan team members consulted with frontline staff during care planning. The resulting care plan was a nonspecific document lacking resident-specific information that was rarely used by the frontline nursing staff.
Researcher: So when you all come up with a plan or modify a plan, how does that trickle back down to the nurses? Care plan team member: Honestly, by word of mouth, because I mean it’s just a bit hard to believe that everybody out there’s gonna open the chart and look at the plan of care. They’re not. I didn’t [when I worked] on the floor.
In summary, the “care plan” at Windy Lane was strictly paperwork driven by regulatory requirements. Staff expected it to have no impact on resident care. Because of thin connections that limited information flow and cognitive diversity, effective self-organization was constrained and care planning was limited to “paper compliance.”
HARBOR
In contrast to the lack of connections among staff at Windy Lane, the pattern at Harbor was more complex. Multiple connections existed between the relatively stable frontline nursing staff (LPNs and CNAs) and other disciplines such as social work, therapy, and medicine. However, connections to the RN-level supervisors, especially the DON and MDS nurses, were absent or strained (Figure 2).
Interdisciplinary team member: But otherwise, the DON, the NHA, we try to avoid them… You really can’t trust them and I don’t get a good vibe from them.
The care planning team at Harbor was led by two RN-level MDS nurses, with the Directors of Social Work and Activities writing some sections independently. Care planning meetings were brief, and for the purpose of obtaining signatures on the appropriate documents. Little or no resident discussion occurred in these meetings.
Field note: [Field Researcher] tells (care plan team member] that she would like to see a care plan meeting. [Care plan team member] says, “We really just rush through them. There is not much to see.”
Administrators reported that interdisciplinary resident care discussions around specific problems, such as falls, also occurred at regularly scheduled “High-Risk Resident” meetings. However, in actuality, these meetings appeared to be infrequent.
Field note: I ask [an interdisciplinary team member) if there is going to be a High-Risk Resident meeting soon. She says, “Oh, we have not had one of those in months. I don’t expect us to.”
Although the MDS nurses took pains to interview every resident prior to writing the care plan, frontline nurses appeared to have little input into the content of formal care plans.
Nurse: Our [care plan team members] do all the care planning. Interviewer: Is anybody else involved? Nurse: Well, I guess actually pretty much the [care plan team member] does all the actual documenting in the care plan and the nurses on the floor have to follow that plan. Interviewer: Do they get any input into the care plan itself? Nurse: I have not seen any since I have been here.
Because of the thin connections between the care plan team and the frontline staff providing care, the care plan was generally not carried out at Harbor. Indeed, during a State Survey that we observed during the study period, the facility was cited several times for failure to implement interventions as stated on the care plan. One care plan team member expressed frustration at this apparent waste of her time and energy.
Care plan team member: So for the most part, care plans are not carried out here and that makes the whole thing seem like a waste for everyone and it frustrates me. I work on these care plans and never see the resident improve.
Although the formal written care plan had minimal impact on patient care at Harbor, there was evidence that spontaneous, self-organized care planning activities occurred between the frontline nursing staff and other members of the interdisciplinary team. These interactions were initiated by frontline staff for the purpose of creatively managing individual resident care issues. For example, facilitated by their multiple connections, several LPNs took the lead in developing a plan of care for their residents.
Field note: [The Physical Therapist] is discussing a resident with [LPN]- They discuss whether a resident needs restraints because the resident seems to be falling a lot. [The Physical Therapist] says, “No, I do not think so yet, but he may get some [additional PT interventions]”...They go on to discuss a new resident.
Although the care plan team at Harbor expended a great deal of time and effort on the formal care plans, without connections to the interdisciplinary team or the frontline nursing staff, their labor resulted only in paper. The self-organized care planning activities that arose in the frontline nursing staff to till this void were admirable but lacked the input of the RN-level staff which might have further improved care. In the example above, the falling resident might have benefited from a further assessment of risk factors such as medications or toileting practices––clinical insights that an RN could have brought to the discussion. Thus, although substantial staff time was spent fulfilling the letter of the law, the care actually delivered was not impacted by OBRA required care plans, but rather by self-organized care planning arising from the connections of the frontline staff outside of the traditional care plan meeting. This illustrates that self-organization will occur even in the absence of adequate information or cognitive diversity, but the resident outcome may not be optimal.
SWEET DELL
In contrast to the pattern of connections observed at Harbor, Sweet Dell had a stable staff with strong connections among the administration and care plan team, while the frontline staff remained isolated. The perception at all levels was that the LPNs were “tied to the med cart,” while care decisions were the domain of the RN-level staff. Formal care planning at Sweet Dell was taken very seriously by the administration and upper level staff.
SW Director: The care planning and the assessment piece is the meat of everything I mean, that’s central control, right there.
Two highly experienced MDS nurses led a well-connected interdisciplinary care planning team, including the DON, Nurse Supervisor, Dietary Director, Activities Director, and SW. A Quality Improvement Nurse and the NHA also had substantial connections with this group (Figure 2). Team members communicated frequently about resident needs in a variety of venues, and formal care plan meetings were regularly scheduled. In contrast to the brief, five-minute per resident meetings at Harbor, the Sweet Dell care plan meetings were lengthy and contained extensive discussions of resident care management.
MDS Nurse: We do a lot of our communications either in the hallway, over the telephone... But when we finally come together for a care plan meeting, then we all are basically just discussing what’s going on, discussing the resident, seeing that we are all on the same page. So COMMUNICATION happens...
In contrast to the strong connections among the care planning team members, connections between the care plan team and the frontline staff were thin (Figure 2). Communication occurred primarily in a hierarchical fashion that staff referred to as “the chain of command.” The CNAs spoke of information moving “up and down the alley,” with a single RN-manager responsible for communicating clinical information to the care plan team, and the care plan team’s decisions back to the frontline staff.
CNA: After we speak with the nurse we go through chains of command… The nurse on that hall, and then they talk to [the RN-manager] and she speaks with [the DON] and she speaks to the family.
As a result, the frontline staff had limited input into care plan development. The RN-manager noted that this frequently resulted in an impractical care plan.
RN-manager: [The Care Plan Team] says, “We are going to put them on a bowel and bladder plan. You go down there and you have the CNAs fill this out, and you make sure it is taken care of.” Well the first thing that they should have done is go to that CNA and found out, is this person a real candidate for the bowel and bladder program, you know what I am saying?
Not surprisingly, the carefully crafted care plans frequently languished on the chart, while frontline staff improvised their own plans for the resident.
Care plan team member: Whether what is on the care plan is implemented or NOT—that’s where the problem sometimes comes. Things just stay in the care plan… and things are done only when THEY [the frontline staff] think they could do it.
So while Sweet Dell had a fully functioning interdisciplinary team spending significant energy on creating a care plan individually tailored to the resident, the team’s thin connections to frontline staff diminished the plan’s utility. Moreover, there was evidence that Sweet Dell team members sometimes modified the content of the care plan because of fears of regulatory oversight.
(Field note from a Care Planning Meeting) Care Plan Team Member 1: “We are going to get killed by [the Physical Therapist’s part of the] care plan. It is too detailed.” Care Plan Team Member 2: “Yeah, there is stuff in there like ‘do this for 15 reps and then rest 15 seconds’ and if we do not do that in detail, we will get it. It needs to be general… If we spell it out in this detail we’re really at risk for the State comin’ in.”
Although the care plan was intended to be a communication tool, in this case, fear of a citation led to a dilution of this function. A less specific care plan would not convey the Physical Therapist’s intentions to the nurse aids who must implement them. The resident would therefore not benefit from the Physical Therapist’s intended intervention.
In summary, Sweet Dell’s communication patterns facilitated formal care planning but stifled both the implementation of the formal plan, and informal, self-organized care planning activities at the front line. Regulatory oversight of care planning led the team to generalize the content of their care plan, making it less likely to benefit the resident.
IVY VINES
Of the four case studies, Ivy Vines had by far the most extensive connections between all levels of staff (Figure 2). Turnover in the facility was relatively low and many administrators and frontline staff had worked in the facility for more than 10 years. There was a well-established interdisciplinary care plan team with frequent formal and informal communication.
[Care plan team member]: And the care plan team’s pretty close. We know about who has [decubitus ulcers]; who has falls; who’s not eating; who’s… not doing too well—and what we can do to improve it. So, the clinical team is pretty close. That plays a big part in the quality of care.
Unlike the care plan team at Sweet Dell, the care plan team at Ivy Vines was well connected to the frontline staff (Figure 2). Indeed, the formal care planning process at Ivy Vines used bedside rounds specifically to include the frontline staff.
MDS Nurse: We involve the CNAs; we involve the nurse; we involve the family, if they will come; we involve the residents… Most of the time, unless there are several family members, we will do it in the resident’s room. We’ll go to the nurses’ station and we talk to the nurses, we talk to the CNAs. If they’re not with somebody else, we’ll pull them into the room.
There was evidence that the CNAs at Ivy Vines, in contrast to the other three cases, actually used and valued the care plan as a tool to improve their care.
Interviewer: So, do you look at the care plan for the resident? CNA: Um hum… And that tell ’ya the patient got Parkinson’s—do they need a wheelchair? Do they do their own bath? You know… It’s good to do it that way, you know. You know about what’s goin’ on with that patient.
Informal care planning at Ivy Vines also happened spontaneously whenever staff was gathered together. For example, the daily administrative “stand up meeting” was a frequent venue for informal care planning discussions, allowing more rapid response to changing resident needs. This was fully supported by the Nursing Home Administrator who voiced concerns that the staff did not have enough time to discuss clinical issues.
Administrator: I’m concerned that [at Stand Up meeting] we don’t have a solid clinical discussion sometimes, the way I think we should. So, I’m thinkin’ of maybe establishing the one o’clock meeting for clinical matters, or to improve or expand the care planning concept… and have that group take a look at ongoing, urgent clinical situations.
Although this combination of formal and spontaneous care planning appeared effective, it had substantial administrative and regulatory repercussions for the facility. It was extraordinarily labor intensive to document mobile and impromptu care planning sessions to meet state requirements.
(Field note from a morning meeting) [Care plan team member 1] then talked about a follow-up meeting yesterday with a resident. [Care plant team member 2] said this amounted to a care plan meeting without her. The [Rehabilitation Director] was apparently at the meeting, and she talked about the things that had been decided and they both said they had done some paperwork … [Care plan team member 2] said, “Just so it’s followed through, ’cause I’m not gonna take the slap.”
(Field note from care plan meeting): Everyone talks about how far behind they are on paperwork. [Care plan team member]: “We are all so far behind all the time because it is impossible to do all the work that needs to be done … We do not even have time to know the patients because there is too much paperwork to do. This is the real story. I would not tell anyone to work in a nursing home.”
Indeed, when a State Survey occurred during the case study period, the facility received a number of citations related to MDS and care plan documentation. These citations included problems such as failure to keep old care plans on the chart long enough or missing signatures; none appeared to be related to care plan implementation. The facility’s response was to require the care plan team to complete an intensive, facility-wide chart audit to identify other documentation problems, and to “overhaul” the care plan process.
Field note from a Stand-up Meeting: [Administrator] then changed the subject and talked about the chart audits that they are trying to put in place as pan of the survey follow up … “I don’t think anyone associated with this wants to repeat this situation.” … [SW] said “we need to revise how we develop a care plan. It’s going to take more time to do that.” [The DON] said, “I have that as part of my action map: to improve quality of MDS, RAPs, care plan process.”
This time-consuming audit clearly distracted the team from ongoing clinical issues.
Field note during internal MDS audit: [Three care plan team members] were still trying to sort out the [MDS documents] that needed some changes. [The Business Manager] said to [a care plan team member] that she needed changes on Thickened Liquids. [The care plan team member], who was fully engaged in the MDS matter, said, “I can’t think clearly right now. Can I get back to you on that?”
Following the state survey visit, the facility moved care planning meetings away from the bedside and into a conference room in an effort to streamline the process and facilitate documentation. Although the long-term effect of this move on the quality and implementation of care plans is not known from our case study data, regulatory burden rather than patient care had become the focus of much of the teams’ discussion.
Field note from Morning Meeting: [Care plan team member] reported that she is “trying to keep people in the house so that we are full and have less paperwork.”
In summary, Ivy Vines initially used its extensive connections among staff to provide innovative, adaptable formal and informal care planning that actually reached the resident. However, their system clashed with the detailed State regulations about care plan documentation. Talented staff members were pulled away from resident care to focus on paperwork. In the end, the facility was forced to move to a care planning system that, as illustrated by the previous cases, is less likely to impact care delivered to the resident.
DISCUSSION
These case studies provide rich accounts of the care planning process actually operating in four skilled nursing facilities. Although the design limits us to hypothesis generation, several key issues are highlighted by our data.
As suggested by the complexity science framework, we observed an association between greater connection among staff and the innovation of care planning. Furthermore, strong connections between the frontline nursing staff and the interdisciplinary care plan team appear to be particularly vital to both formal care plan implementation and self-organized informal care planning. Although this result may not be surprising, it is striking how easily connection can be disrupted and care plan effectiveness diluted. We hypothesize, therefore, that the degree of frontline staff connectedness to the interdisciplinary care plan team is an important determinant of resident outcomes, and may account for the inconsistent care process changes observed after implementation of the RAI. 8,9 Although our study design does not allow us to systematically examine differences in resident outcomes across homes with different patterns of communication, some additional data suggest that it may be possible to examine this in the future. We collected publicly reported MDS quality prior to each case study, and calculated a quartile rank for each study facility compared to other NC nursing homes. Interestingly, Ivy Vines with its high density of connections was in the lowest quartile for adverse resident outcomes, whereas the other three homes ranked in the highest quartile. Interventions designed specifically to create or strengthen the number and quality of connections, either alone or in combination with traditional health services interventions, may he an effective way to achieve better resident outcomes and deserve further study.
Second, we observed that informal, impromptu care planning was more likely to include resident-specific information, and more likely to be implemented than the formal care plans. At the same time, we were repeatedly told about the tremendous time burden imposed by format care plan meetings and documentation. Given increasing resident frailty and a limited number of RN-level staff in nursing homes, it may be unwise to tie up the most highly trained staff with paperwork and meetings. New models of care planning are needed to get our professional staff out of the conference room and into real-time resident care decisions.
Finally, we observed a troubling impact of regulatory oversight on the care planning process. Although the intent of regulations may be to improve cognitive diversity and information flow in care planning, thin connections between the care plan team and the frontline nursing staff in three of the four homes severely limited their impact. More concerning, we observed that a “fear of a citation” led facilities to write less specific care plans and to abandon effective care planning processes. Better quality measures are needed so that regulators can fulfill their obligation to protect nursing home residents without focusing on documentation that may be unrelated to care actually delivered. Nursing homes may need to invest in new technologies such as computerized documentation and decision support systems, and provide administrative support to reduce the burden of documentation on their clinical staff.
Although other theories of group interaction, such as small group dynamics theories, could also he used to frame the care planning process, we believe that the complexity science framework presented here has both theoretical and practical advantages. First, care planning is a process that is carried out in a system. Small group dynamics (e.g., conflict, cohesion) are of less interest than the interactional relationship of members with the system. Second, group theory maintains that the connection in groups occurs in predictable patterns or “structure.” As can be seen from the connection maps in Figure 2, different communication patterns were observed despite the regulations attempting to standardize care planning team membership, and similar organizational composition. Complexity theory better explains these unpredictable connection patterns, and highlights them as key in determining information flow, self-organization, and innovation.
In addition to its theoretical advantages, framing our study in complexity science also offers practical implications for nursing home managers and practitioners seeking to improve it. First, our study suggests that ensuring opportunities for connection among diverse nursing home staff is vital in setting the stage for effective resident care planning. Managers should consider implementing systematic opportunities, such as shift report, meetings, and rounds, as well as encouraging informal staff interaction. Our case studies further suggest that frontline staff especially need to be connected to the interdisciplinary team and each other. Finally, facilitating information flow about resident care issues throughout the facility is a key step in fostering effective care planning. Current privacy laws make these challenging, but creative solutions through information technology or low-tech strategies, such as ensuring private space for shift report and staff discussions, can be employed. Although the care plan process is distinct in nursing homes, we believe that our findings are likely generalizable to other health settings where interdisciplinary cooperation is needed to produce quality outcomes.
Acknowledgments
This project was funded by NIH/NINR (2 R01 NR003178-04A2, Anderson, PI) with support of the Trajectories of Aging and Care Center (NINR 1 P20 NR07795-01, Clipp PI), the Hartford Interdisciplinary Geriatric Research Center at Duke University (RAND/John A. Hartford Foundation 2001-0349; RAND Project HE546, Colon-Emeric PI), the Claude A. Pepper Older American’s Independence Center AG-11268, and a Paul A. Beeson Award (NIA AG024787, Colon-Emeric PI).
Contributor Information
Cathleen S. Colón-Emeric, Assistant Professor of Medicine, Department of Medicine, Division of Geriatrics, and The Center for the Study of Aging and Human Development, Duke University Medical Center, Durham, North Carolina. E-mail: colon001@mc.duke.edu..
Deborah Lekan-Rutledge, Clinical Associate, The Trajectories of Aging and Care Center, Duke University School of Nursing, Box 3322, Duke University Medical Center, Durham, North Carolina. E-mail: deborah.lekan-rutledge@duke.edu..
Queen Utley-Smith, Assistant Professor of Nursing, The Trajectories of Aging and Care Center, Duke University School of Nursing, Duke University Medical Center, Durham, North Carolina. E-mail: queen.utley-smith@duke.edu..
Natalie Ammarell, Research Analyst, The Trajectories of Aging and Care Center, Duke University School of Nursing, Duke University Medical Center, Durham, North Carolina. E-mail: Natalie.ammarell@duke.edu..
Donald Bailey, Assistant Professor of Nursing, The Trajectories of Aging and Care Center, Duke University School of Nursing, Duke University Medical Center, Durham, North Carolina. E-mail: donald.bailey@duke.edu..
Mary L. Piven, Assistant Professor of Nursing, The Trajectories of Aging and Care Center, Duke University School of Nursing, and The Center for the Study of Aging and Human Development, Duke University Medical Center, Durham, North Carolina. E-mail: piven001@mc.duke.edu..
Kirsten Corazzini, Assistant Professor of Nursing, The Trajectories of Aging and Care Center, Duke University School of Nursing, and The Center for the Study of Aging and Human Development, Duke University Medical Center, Durham, North Carolina. E-mail: kirsten.corazzini@duke.edu..
Ruth A. Anderson, Professor of Nursing, The Trajectories of Aging and Care Center, Duke University School of Nursing, and The Center for the Study of Aging and Human Development, Duke University Medical Center, Durham, North Carolina. E-mail: ruth.anderson@duke.edu..
References
- 1.Dellefield ME. Interdisciplinary care planning and the written care plan in nursing homes: a critical review. Gerontologist. 2006;46(1):128–33. doi: 10.1093/geront/46.1.128. [DOI] [PubMed] [Google Scholar]
- 2.Hawes C, Mor V, Phillips CD, Fries BE, Morris JN, Steele-Friedlob E, et al. The OBRA-87 Nursing Home Regulations and Implementation of the Resident Assessment Instrument: Effects on Process Quality. Journal of the American Geriatric Society. 1997;45:977–85. doi: 10.1111/j.1532-5415.1997.tb02970.x. [DOI] [PubMed] [Google Scholar]
- 3.Hawes C, Morris J, Phillips C, Fries B, Murhpy K, Mor V. Development of the Nursing Home Resident Assessment Instrument (RAI) in the US. Age & Ageing. 1997;26(S2):19–26. doi: 10.1093/ageing/26.suppl_2.19. [DOI] [PubMed] [Google Scholar]
- 4.Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, et al. Designing the National Resident Assessment Instrument for Nursing Homes. Gerontologist. 1990;30:293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- 5.Piven M, Ammarell N, Bailey D, Corazzini K, Colón-Emeric C, Lekan-Rutledge D, et al. MDS Coordinator Relationships and Nursing Home Processes. Western Journal of Nursing Research. 2006;28:294–309. doi: 10.1177/0193945905284710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Achterberg W, Holtkamp C, Kerkstra A, Pot A, Ooms M, Ribbe M. Improvements in the Quality of Co-ordination of Nursing Care following Implementation of the Resident Assessment Instrument in Dutch Nursing Homes. Journal of Advanced Nursing. 2001;35(2):268–75. doi: 10.1046/j.1365-2648.2001.01843.x. [DOI] [PubMed] [Google Scholar]
- 7.Holtkamp C, Kerkstra A, Ribbe M, van Campen C, Ooms M. The Relation Between Quality of Co-ordination or Nursing Care and Quality of Life in Dutch Nursing Homes. Journal of Advanced Nursing. 2000;32(6):1364–73. doi: 10.1046/j.1365-2648.2000.01626.x. [DOI] [PubMed] [Google Scholar]
- 8.Bates-Jensen BM, Cadogan M, Osterweil D, Levy-Storms L, Jorge J, Al-Samarrai N, et al. The Minimum Data Set Pressure Ulcer Indicator: Does It Reflect Differences in Care Processes Related to Pressure Ulcer Prevention and Treatment in Nursing Homes? Journal of the American Geriatric Society. 2003;51(9):1203–12. doi: 10.1046/j.1532-5415.2003.51403.x. [DOI] [PubMed] [Google Scholar]
- 9.Schnelle JF, Cadogan MP, Yoshii J, Al-Samarrai NR, Osterweil D, Bates-Jensen BM, et al. The Minimum Data Set Urinary Incontinence Quality Indicators: Do They Reflect Differences in Care Processes Related to Incontinence? Medical Care. 2003;41(8):909–22. doi: 10.1097/00005650-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Anderson R, Issel L, McDaniel R. Nursing Homes as Complex Adaptive Systems: Relationship Between Management Practices and Resident Outcomes. Nursing Research. 2003;52:12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cilliers P. Complexity and Postmodernism: Understanding Complex Adaptive Systems. London: Routledge; 1998. [Google Scholar]
- 12.Anderson R, Crabtree B, Steele D, McDaniel R. Case Study Research: The View from Complexity Science. Qualitative Health Research. 2005;15(5):669–85. doi: 10.1177/1049732305275208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson R, McDaniel R. The Relationship of RN Participation in Organizational Decision Making to Quality of Care in Nursing Homes. Health Care Management Review. 1999;24(1):7–16. doi: 10.1097/00004010-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Ashmos D, Duchon D, McDaniel R. Participation as a Complicating Mechanism: The Effect of Clinical Professional and Middle Manager Participation on Hospital Performance. Health Care Management Review. 1998;23(4):7–21. doi: 10.1097/00004010-199802340-00002. [DOI] [PubMed] [Google Scholar]
- 15.McDaniel R, Walls M. Diversity as a Management Strategy for Organizations: A View through the Lens of Chaos and Quantum Theories. Journal of Management Inquiry. 1997;6:371–83. [Google Scholar]
- 16.Crabtree B, Miller W. Research Practice Setting: A Case Study Approach. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- 17.Utley-Smith Q, Bailey D, Ammarell N, Colón-Emeric C, Corazzini K, Lekan-Rutledge D, et al. Exit Interview-Consultation: A Research Validation Strategy. Western Journal of Nursing Research. 2006 doi: 10.1177/0193945905282301. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandelowski M, Barroso J. Classifying the Findings in Qualitative Studies. Qualitative Health Research. 2003;13:905–23. doi: 10.1177/1049732303253488. [DOI] [PubMed] [Google Scholar]


