Abstract
Objective
To propose e‐learning methods that address the fundamental problems related to sonographic training in rheumatology.
Methods
The project was designed for rheumatologists with strong motivation to learn ultrasound. A modular approach was constructed, consisting of a basic 3‐day residential course, followed by a 6‐month period of web‐based tutoring, and culminating in a final 2‐day residential course with a formal assessment of competency.
Results
The website (http://www.e‐sonography.com) was accessed by all 60 participants. A mean of 20 (range 10–80) log‐on sessions were registered for each participant, and a mean of 250 min (range 60–600 min) of web access was recorded. A total of 163 sonographic images were submitted by 18 (30%) participants. The majority of the images focused on the following anatomical areas: shoulder 49 (30%), hand 34 (21%) and knee 20 (12%). A total time investment of approximately 14 h was made by the US tutors over the 6‐month period for interaction with the participants.
Conclusions
The e‐learning methods described in this report represent the first attempt to adopt a novel technique to circumvent several of the inherent barriers to the many facets of teaching musculoskeletal ultrasound to a wide audience.
Sonographic training in rheumatology is considered by many to be a virtually endless process, and currently there is no agreement between recognised experts on the best approach to adopt.1,2,3,4,5,6 In recent years, several proposals have been put forward with the aim of addressing the specific difficulties encountered by rheumatologists training in ultrasonography (US).7,8,9
Direct supervision by an expert is universally recognised as a core element for appropriate training in US.1,4,10,11 Unfortunately, this approach is beset with logistical difficulties in terms of the relative lack of recognised tutors together with constraints on time for both tutor and student.
The primary aim of this report is to propose methods that directly address these fundamental problems in a web‐based approach. As a secondary aim, we endeavoured to provide an overall assessment of clinical US competency.
Methods
The project was designed for rheumatologists with strong motivation to learn US and was advertised in all Italian rheumatology departments. A modular approach to training was constructed, consisting of a basic 3‐day residential course, according to the standard provided by The European League Against Rheumatism (EULAR) sonography courses, followed by a 6‐month period of web‐based tutoring and culminating in a final 2‐day residential course with a formal assessment of competency.
The basic course
The introductory basic US course was organised for a total of 60 rheumatologists from all over Italy. The main aim of the introductory course was to convey basic knowledge in clinical US. The programme included lectures and practical sessions with healthy subjects and patients with rheumatic disease. Dedicated presentations were given related to the eight anatomical sites indicated in the published guidelines of musculoskeletal US in rheumatology 4: shoulder, elbow, wrist, hand, hip, knee, ankle and foot.
Practical sessions were focused on conveying the following issues: optimisation of the setting of US systems, fundamentals of the scanning technique, identification of basic US patterns of normal anatomy and recognition of basic pathological findings in patients with rheumatic disease.
The web‐based learning module
In the intervening 6‐month period between the introductory basic course and the final module, candidates were encouraged to access the website (http://www.e‐sonography.com) both for educational purposes and to submit their own US images for interaction with tutors.
The website is divided into five main parts.
Teaching aids including a pictorial gallery containing 40 representative US images covering technology and pathology, links to internet sources including 24 freely accessible scientific papers and a list of current textbooks.
A database containing the entire compendium of standard scans from the eight anatomical sites, and three types of images, shown in (fig 1).
Interaction between the rheumatologist in training and the tutors. The participants submitted their own US images for comment. The system records the authorship of the US images but displays them anonymously. In this way, the tutors were able to be critical when necessary, without fear of pillorying. A gallery of submitted images and the corresponding comments of the tutor were freely accessible to all the participants in an open forum.
Testing basic US knowledge in rheumatology. It comprised sets of multiple‐choice questions (MCQs) focusing on four main topics (US technique, US anatomy, US pathology and US image interpretation) with only a single correct answer. The correct answer was provided together with specific literature references, where appropriate. A score > 75% was required to pass each set of MCQs.
Fifty longitudinal dorsal scans of metacarpophalangeal joints in patients with rheumatoid arthritis (25 greyscale and 25 power Doppler images) to train participants in grading synovitis and degree of power Doppler signal, using a recognised semiquantitative scoring system ranging from 0 to 3.12
Figure 1 An example of a web page displaying the three types of images (the anatomical image, the probe image and the sonographic image) obtained by selecting the anterior transverse scan in neutral position at the bicipital groove (>) of the shoulder. t = biceps tendon; d = deltoid muscle. The anatomical image: images obtained at three different levels, from the most superficial to the deepest, showing the most relevant structures visualised by US. Each image can be maximised, with an accompanying detailed legend (fig 1B–D). The probe image: an image showing the exact positioning of the probe, using a coloured band indicating the probe footprint as a reference. The sonographic image: a representative image of US anatomy or pathology with a detailed legend.
The competency assessment
This was formulated in two steps.
Interpretation of US findings. Following a brief tutorial given during the basic course on scoring synovitis and power Doppler signal, participants were asked to independently evaluate 50 US images. Re‐evaluation of the same images was performed at the end of the 6‐month period of web‐based learning.
-
Formal assessment of overall competency in basic musculoskeletal US was carried out in accordance with the method described by Taggart et al7:
-
-
A. Thirty MCQs covering technique, anatomy, pathology and image interpretation.
-
-
B. Practical US session with healthy subjects. Each candidate performed and stored 15 standard scans in a 30 min period.
-
-
C. Practical US session with two patients. Each candidate performed and stored images of two anatomical regions over 30 min.
-
-
A score of at least 80% was required to pass the MCQ questionnaire. In the practical sessions, the stored images were evaluated according to the quality of the pictures obtained and adherence to the findings detected by experienced operators, who acted as the gold standard. Again, a score of 80% was required to pass these sections of the examination. All three components of the examination had to be passed for a participant to be judged successful.
Participants were also asked to complete a satisfaction questionnaire relating to the educational value of the experience.
Results
The basic course
In all, 60 participants attended the 3‐day basic US course. Table 1 gives an overview of the demographic and technological background of the candidates.
Table 1 Demographic and technological backgrounds of the participants attending the ultrasonography course, subdivided according to their success in the final competency assessment.
| Passed (n = 14) | Failed (n = 46) | |
|---|---|---|
| Demography | ||
| Rheumatology trainee | 4 (28.6%) | 10 (21.7%) |
| Rheumatology specialist | 10 (71.4%) | 36 (78.3%) |
| Training | ||
| Trained by rheumatologist | 5 (35.8%) | 8 (17.4%) |
| Trained by radiologist | 3 (21.4%) | 5 (10,9%) |
| Trained by both rheumatologist and radiologist | 3 (21.4%) | 3 (6,5%) |
| Self–taught | 3 (21.4%) | 17 (36,9%) |
| No training | 0 | 13 (28,3%) |
| Current practice | ||
| Use of US: diagnostic | 13 | 26 |
| Use of US: US guidance | 11 | 16 |
| Use of US: monitoring | 11 | 16 |
| Use of US for research purposes | 9 | 12 |
| Departmental track record in US | 11 | 15 |
| equipment | ||
| US equipment— owned | 12 (85.8%) | 20 (43.5%) |
| US equipment— shared | 1 (7.1%) | 7 (15.2%) |
| US equipment— borrowed | 1 (7.1%) | 6 (13%) |
| No access to US system | 0 | 13 (28.3%) |
| Use of the website | ||
| Information search | 14 (100%) | 46 (100%) |
| Submission of images | 11 (78.6%) | 7 (15.2%) |
US, ultrasonography.
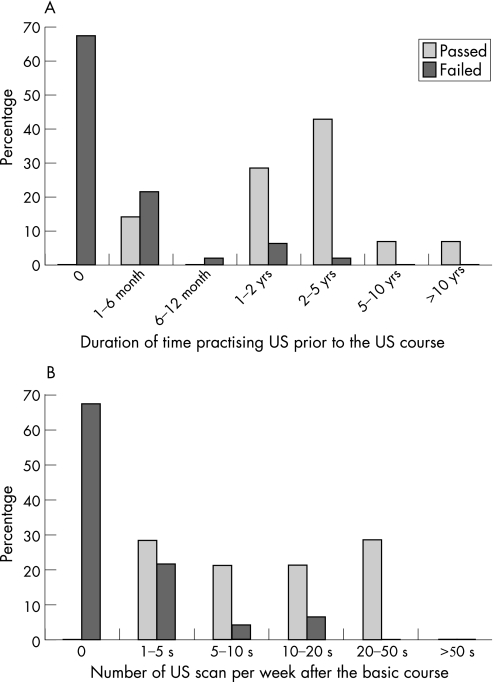
Figure 2 describes the duration of time each candidate had been practising US before attending the course (fig 2A), and the number of scans performed per week after the basic course (fig 2B).
Figure 2 (A) Duration of time spent by candidates practising (US) before the course. (B) Number of US scans performed by candidates in routine practice on a weekly basis.
The website
The website was accessed by all 60 participants. A mean of 20 (range 10–80) log‐on sessions was registered for each participant, and a mean of 250 min (range 60–600 min) of web access was recorded. A total of 163 US images were submitted by 18 (30%) of the 60 participants. The majority of the US images focused on the following anatomical areas: shoulder 49 (30%), hand 34 (21%) and knee 20 (12%).
The comments made by the tutors covered the following main categories: reasons for considering a US image to be of unacceptable quality (ie, lack of recognised landmarks essential for standardisation of the scan), advice aiming to improve the quality of the US images (ie, use of a larger quantity of gel, reduction of the degree of probe compression, increasing the level of magnification to better appreciate some details contained in the US images) and guidance on how to describe the basic US findings. The tutors scored each US image globally with a number ranging from 0 to 10. A total time investment of approximately 14 h was made by the US tutors over the 6‐month period for interaction with participants.
The competency assessment
After 6 months of e‐learning, there was an improvement in the percentage of participants who agreed with the tutors in the evaluation of synovitis and power Doppler signal at the metacarpophalangeal joints in 19 (76%) out of 25 greyscale images and in 18 (72%) out of 25 power Doppler images.
Of the 60 participants, 14 (23%) passed the overall competency assessment.
Subanalysis revealed that only three participants did not get the 80% of correct answers required to pass the MCQ section. The majority of participants who failed the overall competency assessment did so because of poor performance in the practical sessions.
In the satisfaction questionnaire, 55 (91.7%) participants reported that they found the course useful or very useful as an educational exercise.
Discussion
Our experience was designed in order to enhance the interaction between the rheumatologist training in US and experts in the field. The enterprise was well received by the participants, interest in the course was widespread, and the feedback was extremely positive from an educational perspective.
There was clear evidence that all participants accessed the website at some stage during the 6‐month period dedicated to e‐learning, most in search of support to US scanning. Only 28 participants (30%) submitted images to the website, because of limited access to a US system, and 14 participants had difficulty related to obtaining US images in digital form.
The concept of e‐learning in US was predominantly aimed at improving the level of basic knowledge pertinent to the performance and interpretation of US to a wide audience. Following 6 months of web‐based tutoring, participants showed an improvement in their ability to assess small‐joint synovitis, together with a high standard of general US knowledge, in the MCQ section of the final competency assessment.
Although only 23% of those attending the course passed the final competency assessment, it is clear that practical experience of US before the basic course, unrestricted access to equipment and regular performance of US scanning were the key determinants of success. Possible explanations for failure in the competency assessment for those who had unlimited access to US equipment include difficulties in adhering to the strict 15 min slot dedicated to each US examination during the practical sessions and in adapting to US equipment with which they were technically unfamiliar.
The website cannot substitute the importance of continual practical exposure to US and the acquisition of skill in the art of scanning.
To further evaluate the effectiveness of e‐learning methods, it would be advisable to offer the facility and free access to US systems providing digital US images, to groups of motivated rheumatologists having the same level of experience in US.
This web‐based modular approach to US training represents the first attempt to adopt a new technique to circumvent several of the inherent barriers to the many facets of teaching musculoskeletal US to a wide audience. Although the process will require evaluation in other centres, the experience has generated sufficient demand in Italy that the venture is being continued and developed further.
Acknowledgments
We thank Dr Gabriella Baldassare for her excellent organising skills and Dr Marco Santini for his excellent technical assistance.
Abbreviations
MCQ - multiple‐choice question
US - ultrasonography
Footnotes
Funding: This study was supported by a grant from Abbott Laboratories (Campoverde, Italy).
Competing interests: None declared.
References
- 1.Grassi W, Salaffi F, Filippucci E. Ultrasound in rheumatology. Best Pract Res Clin Rheumatol 200519467–485. [DOI] [PubMed] [Google Scholar]
- 2.Kane D, Grassi W, Sturrock R, Balint P V. Musculoskeletal ultrasound—a state of the art review in rheumatology. Part 2: clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology 200443829–838. [DOI] [PubMed] [Google Scholar]
- 3.Brown A K, O'Connor P J, Wakefield R J, Roberts T E, Karim Z, Emery P. Practice, training, and assessment among experts performing musculoskeletal ultrasonography: toward the development of an international consensus of educational standards for ultrasonography for rheumatologists. Arthritis Rheum 2004511018–1022. [DOI] [PubMed] [Google Scholar]
- 4.Backhaus M, Burmester G R, Gerber T, Grassi W, Machold K P, Swen W A.et al Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis 200160641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Speed C A, Bearcroft P W. Training in musculoskeletal sonography: report from the first BSR course. Rheumatology 200241346. [DOI] [PubMed] [Google Scholar]
- 6.Wakefield R J, Brown A K, O'Connor P J, Karim Z, Grainger A, Emery P. Musculoskeletal ultrasonography: what is it and should training be compulsory for rheumatologists? Rheumatology 200443821–822. [DOI] [PubMed] [Google Scholar]
- 7.Taggart A, Filippucci E, Wright G, Bell A, Cairns A, Meenagh G.et al Musculoskeletal ultrasound training in rheumatology: the Belfast experience. Rheumatology 200645102–105. [DOI] [PubMed] [Google Scholar]
- 8.Filippucci E, Unlu Z, Farina A, Grassi W. Sonographic training in rheumatology: a self teaching approach. Ann Rheum Dis 200362565–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D'Agostino M A, Maillefert J F, Said‐Nahal R, Breban M, Ravaud P, Dougados M. Detection of small joint synovitis by ultrasonography: the learning curve of rheumatologists. Ann Rheum Dis 2004631284–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faculty of Clinical Radiology, Royal College of Radiologists Ultrasound training recommendations for medical and surgical specialties. London: Royal College of Radiologists, 2005
- 11.Cunnington J, Hide G, Kane D. Training in musculoskeletal ultrasound by UK rheumatologists: when is now, but how? Rheumatology 2005441470–1472. [DOI] [PubMed] [Google Scholar]
- 12.Naredo E, Bonilla G, Gamero F, Uson J, Carmona L, Laffon A. Assessment of inflammatory activity in rheumatoid arthritis: a comparative study of clinical evaluation with Gray‐Scale and power Doppler ultrasonography. Ann Rheum Dis 200564375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]