Figure 2.
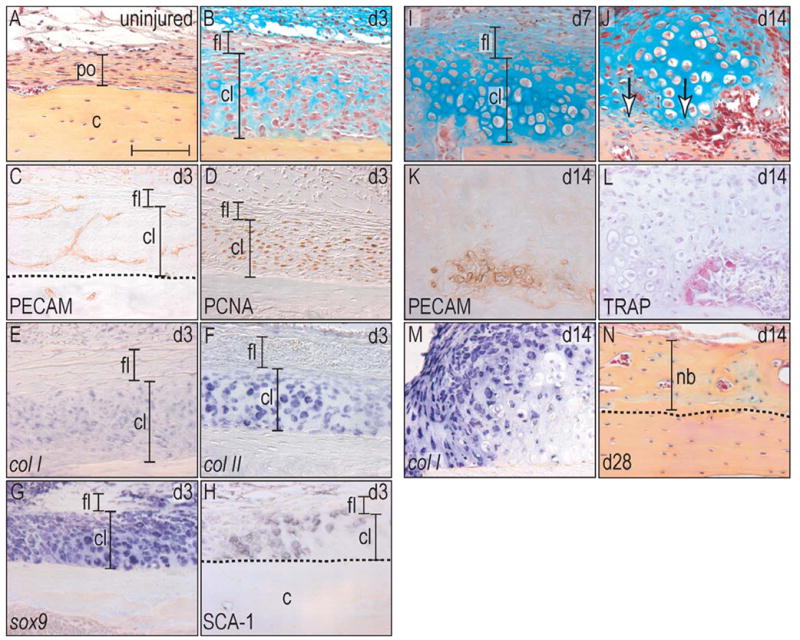
Implant placement induces periosteal proliferation and finally endochondral bone formation.
(A) Uninjured periosteum consists of a one cell layer thick cambial layer that is surrounded by a thicker fibrous layer. (B) At post-surgical day 3, the cambial layer has thickened almost tenfold, whereas the fibrous layer did not change histologically. (C) Newly formed vessels invaded into the cambial layer and created a capillary network. (D) PCNA-staining showed proliferative activity exclusively in the cambial layer. (E–G) In situ hybridization revealed that the proliferating cells were also positive for the osteochondroprogenitor cell marker col I, col II, sox9. (H) Sca-1 immunohistochemistry confirmed their osteoprogenitor capacity. (I) At post-surgical day 7, osteochondroprogenitor cells differentiated into chondrocytes with a subset showing signs of hypertrophy. (J) After 14 days, first signs of bone matrix deposition were evident (arrows), (K) and this mineralization was located close to newly formed vasculature. (L) Simultaneously with the deposition of a new bone matrix, TRAP positive osteoclasts started to remodel the newly deposited bone. (M) Col I in situ hybridization labeled the majority of cells in the periosteum, indicating their osteogenic potential, but was absent in hypertrophic chondrocytes. (N) At post-surgical day 28, the program of endochondral bone formation had finished and the new matrix was almost indistinguishable from the preexisting cortical bone. Abbreviations: c: cortex; cl: cambial layer; fl: fibrous layer; nb: new bone; po: periosteum. Scale bar: 100 μm.
