Abstract
Background
A greater knee adduction moment increases risk of medial tibiofemoral osteoarthritis (OA) progression. Greater toe‐out during gait shifts the ground reaction force vector closer to the centre of the knee, reducing the adduction moment. The present study was designed to test whether greater toe‐out is associated with lower likelihood of medial OA progression.
Methods
Baseline assessments included: kinematic/kinetic gait parameters using an optoelectronic camera system, force platform and inverse dynamics to calculate three‐dimensional external knee moments; toe‐out angle (formed by the line connecting heel strike and toe‐off plantar surface centres of pressure and the forward progression line; knee pain; and full‐limb alignment. Knee x‐rays (semi‐flexed) were obtained at baseline and at 18 months, with progression noted as medial joint space grade worsening. With logistic regression, odds ratios (ORs) for progression/5° toe‐out were estimated.
Results
In the 56 subjects (59% women, mean age 66.6 years, body mass index (BMI) 29), baseline toe‐out angle was less in knees with than without progression (difference –4.4, 95% CI –8.5 to –0.3). Greater toe‐out was associated with reduced likelihood of progression (OR 0.60, 95% CI 0.37 to 0.98). Adjusting for age, gender, BMI, pain severity and disease severity, the OR was 0.62, 95% CI 0.36 to 1.06. Adjusting for adduction moment (second peak), the OR was 0.72, 95% CI 0.40 to 1.28.
Conclusions
Osteoarthritic knees that progressed had less toeing‐out than knees without progression. Greater toe‐out was associated with a lower likelihood of progression. Adjustment for covariates did not alter the OR, although the 95% CI included 1. Further adjustment for adduction moment did alter the OR, consistent with the possibility that a mechanism of the effect may be via lowering of the adduction moment.
Knee osteoarthritis (OA) is a major cause of symptoms and chronic disability in older individuals. In knee OA, disease is most commonly present in the medial tibiofemoral compartment. The susceptibility of the medial compartment to OA may relate to the greater load—that is, 60–80% of the total load—distributed to the medial compartment as compared with the lateral compartment during gait even in healthy knees. Excessive medial compartment loading is widely believed to contribute to medial OA development and progression.
From a biomechanical perspective, changes in certain kinematic or kinetic parameters during gait could, in theory, reduce medial load. Identifying, from among those parameters with a biomechanical rationale, which ones are linked to a reduction in the risk of knee OA progression over time is key information to direct development of novel, and potentially disease‐modifying, rehabilitative intervention.
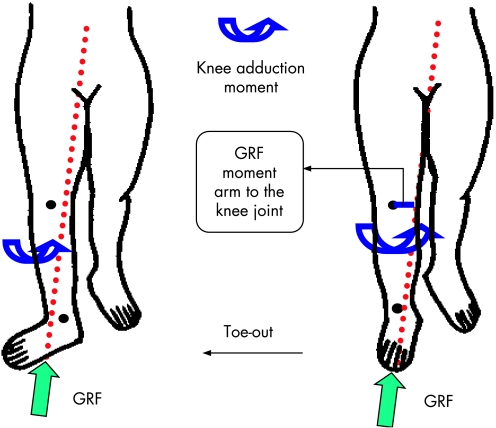
Walking with a greater toe‐out angle (the angle formed by the long axis of the foot—that is, mid‐heel to second toe, and the straight‐forward line of progression of the body) may reduce the knee adduction moment,1,2,3,4 a correlate of medial load and a predictor of medial OA progression.5 The product of the ground reaction force (GRF) vector in the frontal plane and the perpendicular distance from the GRF vector to the knee joint centre of rotation (the frontal plane moment arm) is a major determinant of the magnitude of the knee adduction moment (see fig 1).4 In theory, out‐toeing during gait shifts the GRF vector closer to the knee joint centre and decreases this moment arm, thereby reducing the knee adduction moment (fig 1).1 In keeping with this theory, greater toe‐out angle was inversely related to the external knee adduction moment during the late stance phase of gait in persons with healthy knees and in persons with knee OA.2,3
Figure 1 Out‐toeing during walking shifts the ground reaction force (GRF) vector closer to the knee joint centre and thus reduces the GRF moment arm (solid line) to the knee joint centre and knee adduction moment (adapted from Wang et al1).
We tested the hypothesis that greater toe‐out angle assessed during quantitative gait analysis is associated with a reduced likelihood of ipsilateral medial tibiofemoral OA progression.
Methods
Participants
MAK (Mechanical Factors in Arthritis of the Knee) is a natural history study of knee OA at Northwestern University. As previously described,6 MAK participants were recruited from several community sources. Inclusion and exclusion criteria were based on recommendations from a National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)/National Institute on Aging (NIA) workshop.7 Inclusion criteria were definite osteophytes in one or both knees, and at least a little difficulty (graded using a Likert scale) with two or more items in the Western Ontario and McMaster University Osteoarthritis Index physical function scale. Exclusion criteria were a corticosteroid injection within 3 months, avascular necrosis, inflammatory arthritis, periarticular fracture, Paget's disease, villonodular synovitis, joint infection, ochronosis, neuropathic arthropathy, acromegaly, haemochromatosis, Wilson's disease, osteochondromatosis, gout, pseudogout, osteopetrosis, bilateral total knee replacement or plans for replacement within the next year.
Additional exclusion criteria for the current study were: replacement of any lower extremity joint; bilateral lateral tibiofemoral OA (based upon the presence of grade 2—that is, definite narrowing, or worse, using the 0–3 scale of the Osteoarthritis Research Society International (OARSI) atlas8). Institutional Review Board approval was obtained. All participants gave informed consent.
Quantitative gait analysis to measure toe‐out angle and knee joint moments
Fifty‐seven MAK participants underwent quantitative gait analysis in the gait lab of Rush‐Presbyterian‐St. Luke's Medical Center, within 1 month of their MAK evaluation. The Computerized Functional Testing Corporation (Chicago, IL, USA) system was used, including four optoelectronic cameras (Qualisys, Gothenburg, Sweden) with a sampling frequency of 120 Hz and a single multicomponent force plate (Bertec, Columbus, OH, USA).
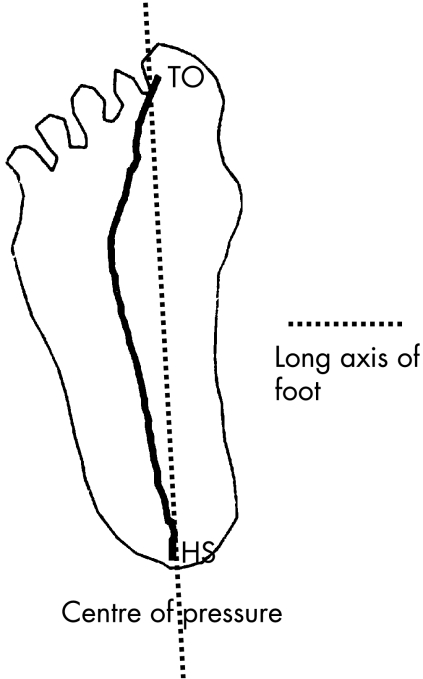
The path of the centre of pressure on the plantar surface of the foot (ie, where the GRF vector can be considered to be acting during gait) was determined from force plate data. The long axis of the foot was formed by connecting the centre of pressure at the time of heel strike with the centre of pressure at toe‐off (fig 2). The toe‐out angle of each leg was computed as the angle formed by the intersection of the long axis of the foot and the direction of forward progression.
Figure 2 The solid line represents the centre of the pressure path from heel strike (HS) to toe‐off (TO). The dashed line represents the long axis of the foot.
Six passive markers were used in the rigid link segment model, placed at the following landmarks: lateral‐most aspect of the superior iliac crest; greater trochanter; lateral joint axis line of the knee; lateral malleolus; lateral aspect of the calcaneous; and base of the fifth metatarsal. Inverse dynamics based on a link segment model were used to calculate the external moments (in three planes) at the hip, knee and ankle joint centres, using the three‐dimensional kinematic data acquired by the cameras along with the GRF and moments obtained with the force plate.
The external moments were calculated by taking into account the moment about the joint centre (created by the GRF) and inertial forces. An external moment is equal and opposite to the internal moment created by muscles, soft tissues and joint contact forces. The external moments were normalised to each subject's body weight multiplied by body height.
The examiner and the investigator processing the gait data were blinded to all radiographic data.
Measurement of covariates
Knee pain severity in the past week was measured using 100 mm visual analogue scales, with separate scales for the right and left knees. The scales were anchored at 0 with “no pain” and at 100 with “pain as bad as it could be”, and standardised instructions were given.
Disease severity was assessed using the Kellgren and Lawrence (K/L) grading system from knee x‐rays acquired with the protocol described below. In the K/L system, 0 = normal, 1 = possible osteophytes, 2 = definite osteophytes, possible joint space narrowing, 3 = moderate osteophytes, definite narrowing, some sclerosis, possible attrition, 4 = large osteophytes, marked narrowing, severe sclerosis, definite attrition.
To assess the severity of varus malalignment, an anteroposterior full‐limb radiograph was obtained using a protocol we have previously described.6 Alignment was measured by one reader as the angle formed by the intersection of the line connecting centres of the femoral head and intercondylar notch with the line connecting centres of the ankle talus surface and tibial spine tips. Our reliability with this approach is high, as previously reported.6
Assessment of OA progression
Bilateral weightbearing knee x‐rays were obtained at baseline and 18 months, following the Buckland–Wright protocol.9 This protocol meets criteria set by the NIAMS/NIA workshop7 and OARSI.10 Knee position, beam alignment, magnification correction and measurement landmarks were specified. The semi‐flexed position of this protocol superimposes anterior and posterior medial tibial margins. Tibial rim alignment and tibial spine centred in the notch were confirmed fluoroscopically before x‐rays were taken. X‐rays were obtained in one unit by two trained technicians. Foot maps made at baseline were used at follow‐up.
Medial tibiofemoral OA progression was defined as any worsening in radiographic medial joint space grade between baseline and 18 months. The illustrated OARSI atlas grades (none, possibly, definitely, severely narrowed joint space)8 were used by one reader. Reliability for radiographic grading (of joint space and K/L) for the single reader was very good (kappa coefficient 0.85–0.86). The knee x‐ray reader was blinded to the gait analysis data.
Statistical analysis
Logistic regression analysis was used to assess the effect of increased toe‐out angle on the odds of medial OA progression in the index knee. Knees with a tibiofemoral joint space grade of 3 at baseline were excluded from analysis, since further progression was not possible. Results are presented as odds ratios (ORs) per 5° of toe‐out angle. There was no precedent in the literature on which to base a choice of toe‐out angle increment for the presentation of our results. We chose 5° as an increment that is small but more tangible and interpretable than 1°. Analyses were adjusted for age (treated as a continuous variable), gender, body mass index (BMI) (continuous), knee pain (continuous) and disease severity (as reflected by K/L grade coded as indicator variables using K/L = 0 as the reference).
Additional analyses further adjusted for the knee adduction moment and the hip external rotation moment (as continuous variables). We specifically considered the first peak, second peak and maximum of the knee adduction moment. If the toe‐out angle effect was achieved in part or wholly via reduction of the adduction moment at the knee, then we expected some reduction of the toe‐out angle/progression relationship after adjusting for the knee adduction moment. Since hip external rotation may contribute to the toe‐out angle and since another hip moment (ie, hip abduction moment) magnitude protected against knee OA progression,11 we examined whether the toe‐out angle/progression relationship was reduced after accounting for potential confounding by the hip external rotation moment.
Results
Our sample consisted of 56 participants (59% women). The mean (SD) age was 66.6 (8.6) years and the mean (SD) BMI was 29.0 (4.2) kg/m2. Of the 56 knees, 40 were K/L 2 and 16 were K/L 3. Fifteen of 56 knees progressed, a rate similar to that found in previous studies using a comparable approach to assess progression.
Table 1 shows the mean toe‐out angle, maximum knee adduction moment, first peak knee adduction moment and second peak knee adduction moment for all knees, and then separately for progressing and non‐progressing knees.
Table 1 The mean toe‐out angle, and the maximum, first and second peak external knee adduction moment (% body weight×height) for all knees and for progressing vs non‐progressing knees.
| All knees, mean (SD) | Progressing knees, mean (SD) | Non‐progressing knees, mean (SD) | Difference between progressing and non‐progressing knees (95% CI of difference) | |
|---|---|---|---|---|
| Toe‐out angle (°) | 21.3 (6.9) | 18.1 (8.4) | 22.5 (6.0) | –4.4 (–8.5 to –0.3) p = 0.03 |
| Maximum knee adduction moment | 2.92 (0.86) | 3.39 (0.82) | 2.74 (0.81) | 0.65 (0.15 to 1.14) p = 0.01 |
| First peak knee adduction moment | 2.91 (0.85) | 3.37 (0.83) | 2.74 (0.81) | 0.63 (0.14 to 1.12) p = 0.01 |
| Second peak knee adduction moment | 2.06 (0.84) | 2.53 (0.96) | 1.88 (0.73) | 0.64 (0.16, 1.13) p = 0.01 |
A 95% CI for the difference that excludes 0 is statistically significant.
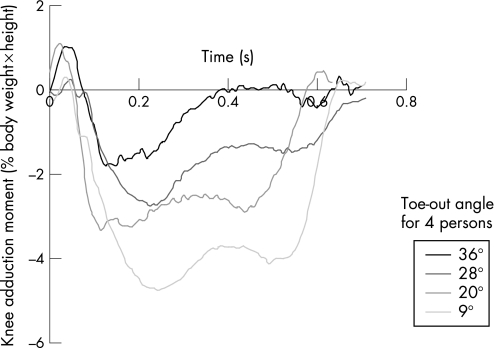
The trajectory of the external knee adduction moment is illustrated for knees from four participants who walked with different toe‐out angles (fig. 3). The participants with larger toe‐out angles had smaller knee adduction moments.
Figure 3 Trajectories of the knee adduction moment are shown for four participants with different toe‐out angles. The x‐axis is time during the gait cycle. The y‐axis is the magnitude of the knee adduction moment.
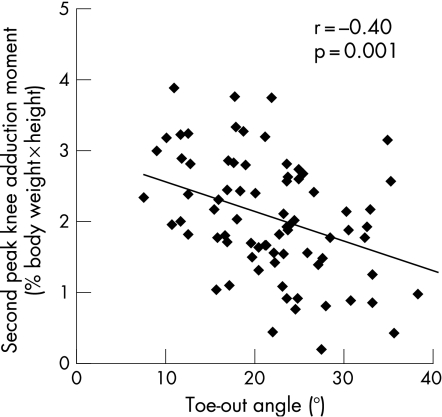
In the full sample, the magnitude of the toe‐out angle was correlated with the second peak of the knee adduction moment (r = –0.41, p = 0.002) and the hip external rotation moment (r = 0.29, p = 0.03), but not the maximum knee adduction moment (r = –0.09) or the first peak of the adduction moment (r = –0.09). The scatterplot in fig 4 illustrates the correlation between toe‐out angle and the second peak of the knee adduction moment.
Figure 4 Scatterplot illustrating the extent of correlation between the toe‐out angle and the second peak of the knee adduction moment.
A greater toe‐out angle at baseline was associated with a reduced likelihood of medial OA progression in the subsequent 18 months (table 2). Adjustment for potential confounders, including age, gender, BMI, knee pain severity and baseline disease severity, minimally changed the magnitude of the OR. There was some evidence of attenuation adjusting for the second peak of the adduction moment (see table 2) and possibly after adjusting for the first peak (adjusted OR 0.67, 95% CI 0.39 to 1.14), but none with adjustment for the maximum adduction moment (adjusted OR 0.59, 95% CI 0.34 to 1.03). There was little change in the OR with adjustment for the hip external rotation moment (table 2).
Table 2 The OR for medial tibiofemoral osteoarthritis progression per 5° toe‐out angle is shown, first unadjusted, and then adjusted for the noted variables.
| Covariates | Toe‐out angle OR for medial OA progression (95% CI) per 5° of toe‐out angle |
|---|---|
| Toe‐out angle (unadjusted) | 0.60 (0.37 to 0.98) |
| Toe‐out angle + age, gender, BMI, knee pain severity, baseline disease severity | 0.62 (0.36 to 1.06) |
| Toe‐out angle + age, gender, BMI, knee pain severity, baseline disease severity + varus malalignment | 0.68 (0.39 to 1.17) |
| Toe‐out angle + age, gender, BMI, knee pain severity, baseline disease severity + second peak knee adduction moment | 0.72 (0.40 to 1.28) |
| Toe‐out angle + age, gender, BMI, knee pain severity, baseline disease severity + hip external rotation moment | 0.61 (0.35 to 1.08) |
BMI, body mass index; OA, osteoarthritis.
A 95% CI that excludes 1 is statistically significant at an α = 0.05 level.
Discussion
Osteoarthritic knees that progressed had a significantly smaller toe‐out angle measured during quantitative gait analysis than knees that did not progress. A greater toe‐out angle at baseline was associated with a reduced likelihood of medial tibiofemoral OA progression over the following 18 months. Adjusting for potential confounders including age, gender, BMI and baseline disease severity did not alter the magnitude of the OR, although the 95% CI included 1. The OR magnitude was altered, however, by adjusting for knee adduction moment, especially the second peak. The relationship between greater toe‐out angle during gait and knee OA progression has not been reported previously.
By moving the GRF vector closer to the knee joint centre, out‐toeing has the potential to reduce the knee adduction moment. The magnitude of the adduction moment at the knee reflects in large part the product of the frontal plane GRF and the frontal plane moment arm.4 Hunt et al found that knees with OA had a greater peak knee adduction moment and frontal plane moment arm, but a lower frontal plane GRF than knees without OA.4 They found a strong correlation between peak knee adduction moment and peak frontal plane moment arm (ie, r = 0.77 and 0.57 in affected and unaffected knees, respectively). On the other hand, the correlation between GRF and the knee adduction moment was relatively weak (r = 0.19 and 0.25). Their results support the study of interventions that reduce the frontal plane moment arm as a potential means of reducing the knee adduction moment.4 The association of greater toe‐out angle (which reduces the moment arm) with reduced likelihood of OA progression adds further support to this concept.
There have been few reports dealing specifically with the toe‐out angle during gait in persons with knee OA. Wang and colleagues1 reported a positive correlation between the ankle inversion moment and the knee adduction moment in persons with knee OA; they proposed a greater toe‐out angle as a potential way to decrease the ankle inversion moment and, thereby, the knee adduction moment. Subsequent work by this group revealed a correlation between the ankle inversion moment and the toe‐out angle (r = 0.68).2 Teichtahl and colleagues reported that the offspring of persons with medial knee OA walked with a smaller toe‐out angle than age‐, gender‐ and BMI‐matched control subjects; there was no difference between groups in peak adduction moment.12
In keeping with our results, previous cross‐sectional studies have found a correlation between toe‐out angle and the second peak of the knee adduction moment, with r values of –0.45 in persons with knee OA3 and –0.44 in persons with healthy knees.2 Further, we report the longitudinal relationship of toe‐out angle to OA disease progression and its partial attenuation by adjusting for the second peak of the knee adduction moment. The current results are consistent with the concept that the mechanism of the effect of out‐toeing may be via a reduction in the magnitude of the adduction moment, particularly the second peak. The mild attenuation seen with adjustment for varus malalignment may reflect the strong relationship between alignment and the adduction moment. The second peak of the adduction moment represents just one instant during the gait cycle, while toe‐out walking occurs during the entire second half of the stance phase. In theory, adjusting for the integral of the adduction moment over a larger portion of the second half of stance may result in greater attenuation of the toe‐out angle effect.
These results characterise the longitudinal relationship between toe‐out angle during gait and knee OA progression, a relationship implied by cross‐sectional studies and biomechanical theory but not previously described. At present, other than weight loss, there are no treatments for knee OA that modify the likelihood or rate of disease progression. Rehabilitative interventions are typically low in cost and could be applied alone or in conjunction with future pharmacological therapies. Toe‐out angle is potentially modifiable using gait training or foot orthotics.
It is important to emphasise that this was an observational study. Clinical trials will be essential to reveal the magnitude of any effect of increasing toe‐out angle on osteoarthritic disease progression at the knee.
In summary, osteoarthritic knees that progressed had a significantly smaller toe‐out angle measured during quantitative gait analysis than knees that did not progress. A greater toe‐out angle at baseline was associated with a reduced likelihood of medial tibiofemoral OA progression over the following 18 months. The toe‐out angle relationship with knee OA progression was partially attenuated by adjusting for the second peak of the knee adduction moment, in keeping with the possibility that a mechanism of the toe‐out angle effect may be via a reduction in the adduction moment.
Abbreviations
BMI - body mass index
GRF - ground reaction force
K/L - Kellgren and Lawrence
MAK - Mechanical Factors in Arthritis of the Knee
NIAMS/NIA - National Institute of Arthritis and Musculoskeletal and Skin Diseases/National Institute on Aging
OA - osteoarthritis
OARSI - Osteoarthritis Research Society International; OR, odds ratio
Footnotes
Funding: NIH/NIAMS p60 ar48098, RO1 48748, R01 AR46225, RR00048.
Competing interests: None.
References
- 1.Wang J W, Kuo K N, Andriacchi T P, Galante J O. The influence of walking mechanics and time on the results of proximal tibial osteotomy. J Bone Joint Surg Am 199072905–909. [PubMed] [Google Scholar]
- 2.Andrews M, Noyes F R, Hewett T E, Andriacchi T P. Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. J Orthop Res 199614289–295. [DOI] [PubMed] [Google Scholar]
- 3.Hurwitz D E, Ryals A B, Case J P, Block J A, Andriacchi T P. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res 200220101–107. [DOI] [PubMed] [Google Scholar]
- 4.Hunt M A, Birmingham T B, Giffin J R, Jenkyn T R. Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis. J Biomech 2006392213–2220. [DOI] [PubMed] [Google Scholar]
- 5.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee OA. Ann Rheum Dis 200261617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma L, Song J, Felson D T, Cahue S, Shamiyeh E, Dunlop D D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001286188–195. [DOI] [PubMed] [Google Scholar]
- 7.Dieppe P, Altman R D, Buckwalter J A.et al Standardization of methods used to assess the progression of osteoarthritis of the hip or knee joints. In: Kuettner KE, Goldberg VM, eds. Osteoarthritic disorders. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1995481–496.
- 8.Altman R D, Hochberg M, Murphy W A, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthr Cartilage 199533–70. [PubMed] [Google Scholar]
- 9.Buckland‐Wright C B. Protocols for precise radio‐anatomical positioning of the tibiofemoral and patellofemoral compartments of the knee. Osteoarthr Cartilage 19953(Suppl A)71–80. [PubMed] [Google Scholar]
- 10.Task Force of the Osteoarthritis Research Society Special Report: design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the OARS. Osteoarthr Cartilage 19964217–244. [DOI] [PubMed] [Google Scholar]
- 11.Chang A, Hayes K, Dunlop D, Song J, Hurwitz D, Cahue S, Genge R, Sharma L. The hip abduction moment and protection against medial tibiofemoral osteoarthritis progression. Arthritis Rheum 2005523515–3519. [DOI] [PubMed] [Google Scholar]
- 12.Teichtahl A J, Morris M E, Wluka A E, Bach T M, Cicuttini F M. A comparison of gait patterns between the offspring of people with medial tibiofemoral osteoarthritis and normal controls. Clin Exp Rheumatol 200321421–423. [PubMed] [Google Scholar]