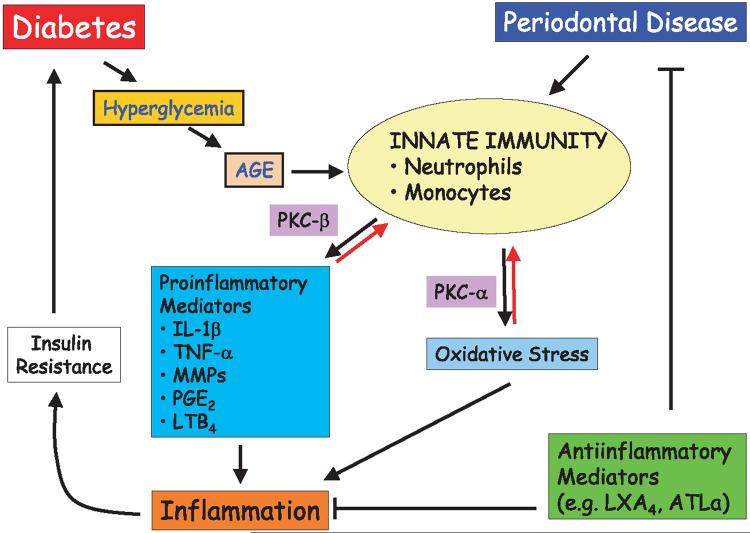
Fig. 1.
Pathways of pathogenesis in diabetic periodontitis. Diabetes initiates a series of innate immune responses through production of advanced glycated end-products (AGEs) as a result of hyperglycemia. Innate immune responses via neutrophils and monocytes lead to proinflammatory cytokine production and will generate oxidative stress through the activities of protein kinase C beta (PKC-β) and PKC-α, respectively. These mediators of host response, in turn, result in inflammatory processes, which would further complicate the glycemic control through insulin resistance. Periodontal disease has a direct effect on the deterioration of diabetic state through the chronic inflammatory changes. All these processes could be potentially blocked through the use of anti-inflammatory mediators. AGE, advanced glycated end-products; PKC, protein kinase C; IL-1β, interleukin-1β; TNF-α, tumor necrosis factor-α; MMPs, matrix metalloproteinases; PGE2, prostaglandin E2; LTB4, leukotriene B4; LXA4, lipoxin A4; ATL-α, aspirin-triggered lipoxin-α.