Abstract
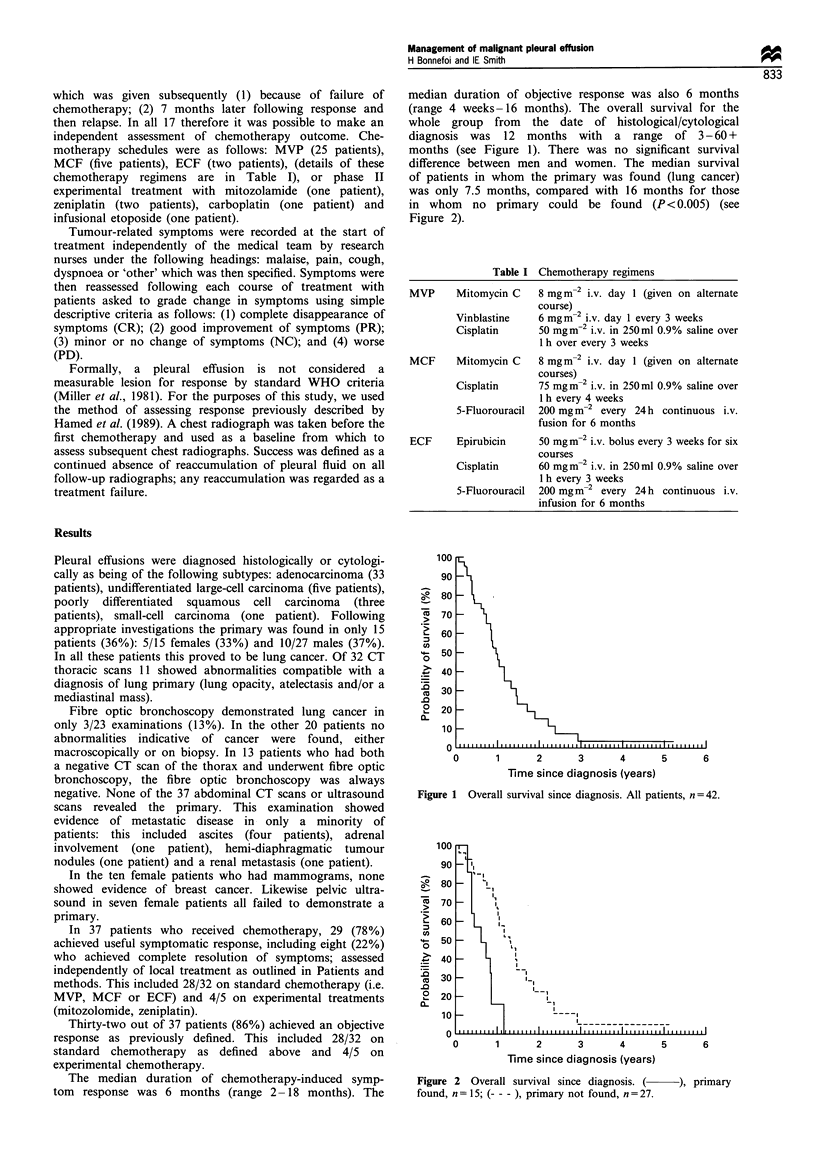
The objective of the study was to review the natural history of patients with a malignant pleural effusion but without obvious evidence of a primary, to assess the value of investigations used to look for a primary and to assess the response to palliative chemotherapy. This was done by a retrospective study of patients' notes at the Lung Unit, Royal Marsden Hospital, Sutton, Surrey. Improvement in tumour-related symptoms (and duration) on chemotherapy was assessed by the patient before the first course of chemotherapy and following each course using simple descriptive criteria as follows: (1) complete disappearance of symptoms (CR); (2) good improvement in symptoms (PR); (3) minor or no change in symptoms (NC); (4) worse symptoms (PD). Pleural effusion objective response (and duration) according to Hamed definition: success defined as a continued absence of reaccumulation of pleural fluid on all follow-up radiographs; any reaccumulation was regarded as a treatment failure. Overall survival was measured from the date of histological/cytological diagnosis to death. The study included 42 patients, 27 males and 15 females with a median age of 55 years. A primary was found in 15 patients (36%), and considered to be lung cancer. A total of 11/32 (34%) had a thoracic computed tomography (CT) scan with abnormalities compatible with a diagnosis of lung primary. When thoracic CT scan was negative, fibre optic bronchoscopy was always negative (0/13). Abdominal and pelvic CT scan, abdominal ultrasound, pelvic ultrasound and mammograms failed to reveal the primary. Twenty-three patients underwent local treatment and 37 received systemic chemotherapy. A total of 29/37 (78%) patients achieved symptomatic improvement (median duration, 6 months) and 32/37 (86%) an objective response of their pleural effusion on chemotherapy (median duration, 6 months). The median survival of the whole group was 12 months (3-60+ months). In this series the thoracic CT led to a diagnosis of lung primary in 34% of the cases. Other radiological examinations and bronchoscopy were unhelpful. Chemotherapy achieved symptom relief in 78% of patients.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abbruzzese J. L., Abbruzzese M. C., Hess K. R., Raber M. N., Lenzi R., Frost P. Unknown primary carcinoma: natural history and prognostic factors in 657 consecutive patients. J Clin Oncol. 1994 Jun;12(6):1272–1280. doi: 10.1200/JCO.1994.12.6.1272. [DOI] [PubMed] [Google Scholar]
- Ellis P. A., Smith I. E., Hardy J. R., Nicolson M. C., Talbot D. C., Ashley S. E., Priest K. Symptom relief with MVP (mitomycin C, vinblastine and cisplatin) chemotherapy in advanced non-small-cell lung cancer. Br J Cancer. 1995 Feb;71(2):366–370. doi: 10.1038/bjc.1995.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinsilver S. H., Barrows A. A., Braman S. S. Fiberoptic bronchoscopy and pleural effusion of unknown origin. Chest. 1986 Oct;90(4):516–519. doi: 10.1378/chest.90.4.516. [DOI] [PubMed] [Google Scholar]
- Fentiman I. S., Millis R., Sexton S., Hayward J. L. Pleural effusion in breast cancer: a review of 105 cases. Cancer. 1981 Apr 15;47(8):2087–2092. doi: 10.1002/1097-0142(19810415)47:8<2087::aid-cncr2820470830>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Fentiman I. S., Rubens R. D., Hayward J. L. A comparison of intracavitary talc and tetracycline for the control of pleural effusions secondary to breast cancer. Eur J Cancer Clin Oncol. 1986 Sep;22(9):1079–1081. doi: 10.1016/0277-5379(86)90009-x. [DOI] [PubMed] [Google Scholar]
- Hainsworth J. D., Johnson D. H., Greco F. A. Cisplatin-based combination chemotherapy in the treatment of poorly differentiated carcinoma and poorly differentiated adenocarcinoma of unknown primary site: results of a 12-year experience. J Clin Oncol. 1992 Jun;10(6):912–922. doi: 10.1200/JCO.1992.10.6.912. [DOI] [PubMed] [Google Scholar]
- Hamed H., Fentiman I. S., Chaudary M. A., Rubens R. D. Comparison of intracavitary bleomycin and talc for control of pleural effusions secondary to carcinoma of the breast. Br J Surg. 1989 Dec;76(12):1266–1267. doi: 10.1002/bjs.1800761214. [DOI] [PubMed] [Google Scholar]
- Kiang D. T., Kennedy B. J. Estrogen receptor assay in the differential diagnosis of adenocarcinomas. JAMA. 1977 Jul 4;238(1):32–34. [PubMed] [Google Scholar]
- Little A. G., Kadowaki M. H., Ferguson M. K., Staszek V. M., Skinner D. B. Pleuro-peritoneal shunting. Alternative therapy for pleural effusions. Ann Surg. 1988 Oct;208(4):443–450. doi: 10.1097/00000658-198810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masood S. Use of monoclonal antibody for assessment of estrogen and progesterone receptors in malignant effusions. Diagn Cytopathol. 1992;8(2):161–166. doi: 10.1002/dc.2840080214. [DOI] [PubMed] [Google Scholar]
- Miller A. B., Hoogstraten B., Staquet M., Winkler A. Reporting results of cancer treatment. Cancer. 1981 Jan 1;47(1):207–214. doi: 10.1002/1097-0142(19810101)47:1<207::aid-cncr2820470134>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Mottolese M., Venturo I., Donnorso R. P., Curcio C. G., Rinaldi M., Natali P. G. Use of selected combinations of monoclonal antibodies to tumor associated antigens in the diagnosis of neoplastic effusions of unknown origin. Eur J Cancer Clin Oncol. 1988 Aug;24(8):1277–1284. doi: 10.1016/0277-5379(88)90215-5. [DOI] [PubMed] [Google Scholar]
- Nystrom J. S., Weiner J. M., Wolf R. M., Bateman J. R., Viola M. V. Identifying the primary site in metastatic cancer of unknown origin. Inadequacy of roentgenographic procedures. JAMA. 1979 Jan 26;241(4):381–383. [PubMed] [Google Scholar]
- Ruckdeschel J. C., Moores D., Lee J. Y., Einhorn L. H., Mandelbaum I., Koeller J., Weiss G. R., Losada M., Keller J. H. Intrapleural therapy for malignant pleural effusions. A randomized comparison of bleomycin and tetracycline. Chest. 1991 Dec;100(6):1528–1535. doi: 10.1378/chest.100.6.1528. [DOI] [PubMed] [Google Scholar]
- Sears D., Hajdu S. I. The cytologic diagnosis of malignant neoplasms in pleural and peritoneal effusions. Acta Cytol. 1987 Mar-Apr;31(2):85–97. [PubMed] [Google Scholar]
- Steckel R. J., Kagan A. R. Diagnostic persistence in working up metastatic cancer with an unknown primary site. Radiology. 1980 Feb;134(2):367–369. doi: 10.1148/radiology.134.2.7352215. [DOI] [PubMed] [Google Scholar]
- Stewart J. F., Tattersall M. H., Woods R. L., Fox R. M. Unknown primary adenocarcinoma: incidence of overinvestigation and natural history. Br Med J. 1979 Jun 9;1(6177):1530–1533. doi: 10.1136/bmj.1.6177.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang V., Fernando H. C., Goldstraw P. Pleuroperitoneal shunt for recurrent malignant pleural effusions. Thorax. 1990 May;45(5):369–372. doi: 10.1136/thx.45.5.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb W. R., Ozmen V., Moulder P. V., Shabahang B., Breaux J. Iodized talc pleurodesis for the treatment of pleural effusions. J Thorac Cardiovasc Surg. 1992 May;103(5):881–886. [PubMed] [Google Scholar]
- Woods R. L., Fox R. M., Tattersall M. H., Levi J. A., Brodie G. N. Metastatic adenocarcinomas of unknown primary site: a randomized study of two combination-chemotherapy regimens. N Engl J Med. 1980 Jul 10;303(2):87–89. doi: 10.1056/NEJM198007103030205. [DOI] [PubMed] [Google Scholar]


