In the 5th century BC, Hippocrates wrote in his third book Of the epidemics (p 35):
7. But there were also other fevers, as will be described. Many had their mouths affected with aphthous ulcerations. There were also many defluxions about the genital parts, and ulcerations, boils (phymata), externally and internally, about the groins. Watery ophthalmies of a chronic character, with pains; fungous excrescences of the eyelids, externally and internally, called fig, which destroyed the sight of many persons. There were fungous growths, in many other instances, on ulcers, especially on those seated on the genital organs. There were many attacks of carbuncle (anthrax) through the summer, and other affections, which are called “the putrefaction” (seps); also large ecthymata, and large tetters (herpetes) in many instances.1
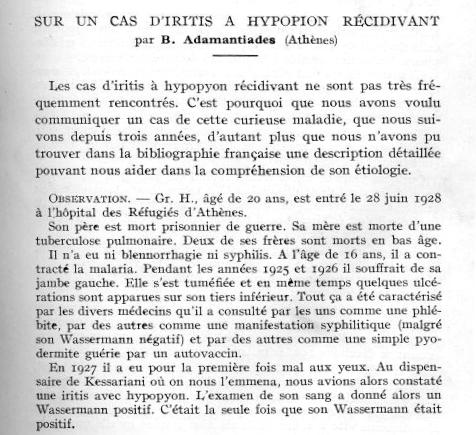
The syndrome was first clearly redescribed by the Greek ophthalmologist Benedict [Benediktos] Adamantiades in 1930–312 and again, independently, by the Turkish dermatologist Hulusi Behçet in 1937. According to Kaklamani et al,3 at the annual meeting of the Medical Society of Athens on 15 November 1930, Benediktos Adamantiades (1875–1962), from Bursa in Turkey, presented a 20‐year‐old man with the three cardinal signs of the disease (see fig 1). This predates his paper of 1931.4 At the age of 18, the patient presented with oedema and ulcerations of the left leg, diagnosed as thrombophlebitis. In the next 2 years (1928–30), he developed recurrent iritis with hypopyon in both eyes, which led to blindness and optic atrophy, scrotal ulcers healing with scars, oral aphthous ulcers and a sterile recurrent arthritis of both knees. Bacterial cultures of the knee and punctures of the anterior eye chamber were sterile, and inoculation into experimental animals proved to be negative. Staphylococci had grown in cultures from scrotal ulcers and a tonsillar abscess.
Figure 1 Adamantiades: on a case of recurrent iritis hypopion.
Table 1 Diagnostic criteria for Adamantiades–Behçet's syndrome (International Study Group for Behçet's Disease, 1990).
| Recurrent oral aphthae | At least three times a year (plus any two of the following four criteria) |
| Genital ulcerations | Active lesion or scar |
| Skin lesions | Erythema nodosum, foliculitis, other ulcerations |
| Involvement of the eye | Anterior or posterior uveitis, or retinal vasculitis |
| Positive pathergy test | Hyper‐reactivity of the skin to pinprick (sterile pustule formed in 24–48 h) – a red papule or pustule >2 mm at the prick site |
Adamantiades suggested a classification with (1) ocular, (2) mucocutaneous and (3) systemic forms,5 later describing thrombophlebitis as a fourth form. He believed that it was a generalised inflammation probably caused by focal staphylococcal infection. He acknowledged publications by Reis (1906) on iritis with erythema nodosum, and Gilbert (1920), who described a similar case with staphylococcal pyoderma; both implicated chronic infections, pyogenic or tuberculous.
In 1937, the syndrome was portrayed independently in three patients by the Turkish dermatologist Hulusi Behçet (1889–1948).6 He suggested a viral aetiology. The University of Istanbul named its medical library after him. Adamantiades–Behçet's disease with relapsing polychondritis has been named the MAGIC syndrome (mouth and genital ulcers with inflamed cartilage).
Neurological symptoms
Onset of the disorder is usually in the third decade, affecting women more often than men. Orogenital ulceration is the cornerstone of the diagnosis, which can be made with increased confidence in the presence of concomitant ocular involvement, arthritis, skin lesions, thrombophlebitis, and cardiac or neurological7 signs. Neurological symptoms are seen to occur in 3.2–49% patients according to reports in different populations. They usually manifest within 5 years of onset. Severe headache is the most common initial neurological symptom. It first attracts attention with meningoencephalitis, a multiple sclerosis‐like illness, acute myelitis, stroke, and pseudotumour cerebri or a brainstem syndrome. Neurological complications8 progress to severe disability, with a high mortality rate. On MRI9 the basal ganglia, brainstem or deep white matter region produce a high signal on T2‐weighted images and an isointense or low signal on T1‐weighted images. Less often, a characteristic linear high signal is produced along the posterior limb of the internal capsule on T2‐weighted images.
Aetiology
Adamantiades–Behçet's syndrome is a systemic inflammatory disease seen frequently among the Japanese and among the population of the Mediterranean basin. Hence it is often called the Silk Road disease. Its geographical distribution is associated with the prevalence of human leucocyte antigens, especially HLA‐B5 and HLA‐B51. In the absence of a diagnostic laboratory test, reliance is placed on clinical diagnosis. The aetiology is imperfectly understood. Vasculitic lesions dominate the pathology. Endothelial injury due to the vasculitis causes activation of platelets, inhibition of fibrinolysis and inhibition of natural anticoagulants (reduced thrombomodulin).
An infective agent has long been postulated but never identified. Neutrophil hyperfunction and an increase in the CD8:CD4 cell ratio occur. An increase in circulating T cells bearing receptors is observed, and peptides derived from the 65 kDa heat shock proteins have been shown specifically to stimulate T cells from patients with the disease.10 The association with HLA B51 is established and associates with uveitis. There is some evidence that B12, DR7 and DR2 may also be linked to tissues affected by the disease.
Treatment is symptomatic and is based on courses of colchicine 0.6 mg twice daily. Topical and oral prednisone 1 mg/kg, or azathioprine 2–3 mg/kg/day, may be used in severe cases. Anti‐TNFα treatment with infliximab (10 mg/kg given twice over a month) has resulted in remissions of more than 12 months.11
Footnotes
Competing interests: None.
References
- 1.Feigenbaum A. Description of Behçet's syndrome in the Hippocratic third book of endemic diseases. Br J Ophthal 195640355–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adamantiades B.A case of recurrent hypopyon iritis. Athens Greece: Medical Society of Athens, 1930586–593.
- 3.Kaklamani V G, Vaiopoulos G, Kaklamanis P G. Behçet disease. Semin Arthritis Rheum 199827197–217. [DOI] [PubMed] [Google Scholar]
- 4.Adamantiades B. Sur un cas d'iritis á hypopion récidivant. Ann Ocul (Paris). 1931;164: 271–8, Full text in French at http://194.254.96.21/livanc/?cote = epo0034&p = 1&do = page (accessed 28 Apr 2006)
- 5.Adamantiadis B. Le symptome complexe de l'uvéite récidivante à hypopyon. Ann Ocul (Paris) 1953186846–856. [PubMed] [Google Scholar]
- 6.Behçet H. Über rezidivierende, aphthöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien. Dermat Wschr 19371051152–1157. [Google Scholar]
- 7.Ho C L, Deruytter M J. Manifestations of neuro‐Behcet's disease. Report of two cases and review of the literature. Clin Neurol Neurosurg 2005107310–314. [DOI] [PubMed] [Google Scholar]
- 8.O'Duffy J D. Behçet's disease. Curr Opin Rheumatol 1994639–43. [PubMed] [Google Scholar]
- 9.Tali E T, Atilla S, Keskin T.et al MRI in neuro‐Behcet's disease. Neuroradiology 1997392–6. [DOI] [PubMed] [Google Scholar]
- 10.Kidd D A, Steuer A, Denman A M.et al Neurological complications in Behçet's syndrome. Brain 19991222183–2194. [DOI] [PubMed] [Google Scholar]
- 11.Goossens P H, Verburg R J, Breedveld F C. Remission of Behcet's syndrome with tumour necrosis factor alpha blocking therapy. Ann Rheum Dis 200160637. [DOI] [PMC free article] [PubMed] [Google Scholar]