Abstract
Aim
To investigate missed opportunities to reveal existing but not formerly diagnosed coronary heart disease cases and related risk factors in primary health care.
Methods
The study comprised 850 people aged over 30 years with no known history of coronary heart disease, receiving health services from a primary care center located in a suburban area of Antalya, Turkey. Data on their age, gender, education level, health insurance status, income, smoking behavior, and physical activities were collected. Undiagnosed coronary heart disease patients were determined by the Rose questionnaire, physical examination, and electrocardiogram. Height and weight, blood pressure, serum glucose and cholesterol levels were measured, and body-mass index and waist-hip ratio calculated. Each patient was given a risk score regarding age, smoking behavior, systolic blood pressure, and cholesterol levels. Estimated risk ratio of each person for developing coronary heart disease in the next decade was determined.
Results
The number of formerly undiagnosed coronary heart disease cases was 126 (14.8%). Overall mean (±standard deviation) risk score for developing coronary heart disease in the next decade in study group was 6.1 ± 6.8. Diseases facilitating development of coronary heart disease: hypertension, diabetes, and hypercholesterolemia were present in 255 (30.4%), 70 (8.2%), and 364 (43.4%) participants, respectively. Obesity was detected in 315 (37.1%) subjects and there were 222 (26.1%) current smokers. For patients who attended primary health care, the estimated percentage risk for developing coronary heart disease in the next ten years was 7 to 45% in men and 2 to 45% in women.
Conclusion
Opportunities to reveal coronary heart disease and its risk factors are being missed in primary care. Measures should be taken to ensure timely diagnosis of coronary heart disease and related risk factors.
Although the etiology and pathophysiology of cardiovascular diseases are well known today, and more effective tools are available to prevent these diseases, they are still the cause of one third of deaths (1,2). About 32 million people develop heart attacks and strokes every year (3). Opportunistic screening is a term which is used to describe the alertness of health care providers to seek for the symptoms and signs of some major disorders such as coronary heart disease, hypertension, hypercholesterolemia, cervical carcinoma, and breast cancer in all patients, regardless of what the main problem is (4). Any health risk can be isolated easily and cost-effectively by this approach in individuals applying for health services for any reason (5). Such an approach provides primary and secondary prevention in patients with pre-existing coronary heart disease (5,6). Neglected opportunistic approach is called “missed opportunity” (7).
Primary Health Care Services in Turkey are organized on the basis of the Law of “Socialization of Health Services,” legislated in 1961. Primary care services are free and provided by the state. The core institution of primary health care is health center in which the staff from different occupation groups such as the physician, dentist, nurse, midwife, health technician, and administrator works as a team. These centers deliver health care services to 10 000 to 40 000 people, depending on location in urban or rural areas. These services include preventing and treating communicable diseases and control of chronic diseases in addition to preventive measures such as immunization, family planning, mother and child care, public health education, environmental health, and health improvement (7).
Turkish people use primary health care institutions at least 2.6 times a year, and the majority of them can find a solution for their health problems in primary care settings without the need to apply for secondary health services (8). This means that the possibility of identifying coronary heart disease and its risk factors is high in primary care if an opportunistic approach is adopted. However, management of coronary heart disease in Turkey is mainly under the responsibility of cardiologists and internists who work in hospitals. There is no reference to coronary heart disease in “Diagnosis and Treatment Guidelines for Primary Health Care” published by Turkish Ministry of Health in 2002 (9) and in “Non-communicable Disease Control Program” initiated in 2002 (10). People with coronary heart disease-related complaints are generally admitted to hospitals or specialists directly, without any barrier in primary care. This causes a lack of interest in coronary heart disease among primary health care providers. We hypothesized that a considerable amount of opportunities to reveal undiagnosed coronary heart disease cases and related risk factors in primary care could be missed. The purpose of this study was to investigate missed opportunities to determine undiagnosed coronary heart disease cases and related risk factors in primary health care.
Methods
Setting
The study was descriptive by design. It was carried out in a suburban locality 8 km far from the city center of Antalya. The majority of the families living in this region migrated from east and southeast parts of Turkey due to socioeconomic reasons. The region has one primary health care center in which there are 9 general practitioners (GPs), 8 nurses, 14 midwives, 2 health care workers, and 2 retainers. Total population of the region is 36 194, according to data from 2003. The number of individuals aged over 30 is 15 695. Three outpatient clinics are available and daily number of examinations at the Center is about 200. The examination rate per individual per year is about 0.8 (11).
Sampling
Participants were selected systematically among all patients applying to the Center for any health problem in a three-month time period, with a sampling rate of 1:3. They were approached when were about to leave the building after an examination by one of the GPs of the center. The first one of every three patients (ie, 1st, 4th, 7th, etc.) was interviewed and 850 subjects matching the inclusion criteria were included in the study group. Inclusion criteria were age over 30 and no known history of coronary heart disease.
All participants were informed about the study and verbal consent was obtained from each. Personal data such as age, gender, education level, health insurance, and income were collected. Undiagnosed coronary heart disease patients were determined and every participant was given a risk score according to the scale used in the Framingham study (12,13) on the basis of age, history of smoking, systolic blood pressure, and cholesterol levels. The risk score ranged from -12 to 18 in women and from -4 to 17 in men. High density lipoprotein (HDL)-related risk score was not measured due to economical restrictions and was presumed zero for each subject. Finally, risk ratio for developing coronary heart disease in the next decade was estimated for each person from the same scale (12,13).
Obesity, positive family history of coronary heart disease, and low physical activity were also accepted as risk factors for coronary heart disease development and were investigated, but not included in the calculations to determine risk scores.
Determination of patients with coronary heart disease
The Rose questionnaire (14) was used to determine and classify medical history of chest pain.. We chose this instrument because it has been already used to determine the prevalence of coronary heart disease in Turkish adults (15). Pain was classified into four groups: “any kind of chest pain,” “angina pectoris grade 1,” “angina pectoris grade 2,” and “possible angina pectoris”. Following physical examination, an electrocardiogram (ECG) was obtained from each participant in supine position. Print rate of the electrocardiograph was 25 mm/s and it was standardized for generating 10 mm deflections for 1 mV change in voltage. Minnesota Codes (14) were used to record ECG findings.
Diagnosis of coronary heart disease
Coronary heart disease or suspected diagnosis was made when the patients had at least one of the following criteria (15): 1) angina pectoris confirmed using a questionnaire (no aortic valve disease or hypertrophic cardiomyopathy detected with physical examination and ECG) with or without hypertensive heart disease. Hypertensive heart disease was defined as hypertension and left ventricular hypertrophy in ECG or apical shift to the left or strong beats felt in apical region by hand in physical examination or possible angina and/or hypertension and left bundle-branch block or left ventricular hypertrophy findings in ECG; 2) ECG findings suggestive of old myocardial infarction (silent ischemia); and 3) signs of congestive heart failure (CHF) unrelated to congenital, valvular, or hypertensive conditions.
Diagnosis of possible coronary heart disease
Patients were diagnosed with possible coronary heart disease when they had at least one of the following criteria: 1) suspicious chest pain for angina pectoris (with or without hypertension); 2) findings of differentiation at left bundle branch block, ischemic type ST segment, or T wave, samples of exact inferior or front wall MI for people over 40 without any other disease who did not have angina; and 3) left ventricular hypertrophy sample in electrocardiograms for people aged over 60.
Patients with valve pathology, coronary heart disease or arrhythmia were referred to secondary health care centers for further investigation and treatment. A standard written feedback form used in daily routine practice was completed for each case and sent to hospitals with patients to confirm or deny our diagnoses.
Determination of coronary heart disease risk factors and measurements
Hypertension. Blood pressure of each participant was measured twice with an interval of 15 minutes. All measurements were performed by the same person from the left arm and the arithmetic mean value of two measurements was recorded. Participants were classified into four groups regarding their blood pressure values (16): 1) normal (<120/80 mm Hg); 2) pre-hypertension (between 120-139/80-89 mm Hg); 3) stage 1 hypertension (between 140-159/90-99 mm Hg); 4) stage 2 hypertension (≥160/100).
Patients under antihypertensive therapy or who declared to have hypertension were also accepted as hypertensive even if their blood pressures were normal.
Diabetes and hypercholesterolemia. Serum cholesterol and fasting blood glucose (FBG) levels were measured using capillary blood samples obtained from the distal phalanx of the second digit after 8 or more hours of fasting by a Reflotron device (Roche Diagnostics, Mannheim, Germany) standardized every morning with control sticks (Accutrend Cholesterol code: 119, Accutrend Glucose code: 896; Roche Diagnostics). Results obtained from the Reflotron were highly correlated (98%) with the results of a reference laboratory in the first 30 cases with no significant difference between them (paired t test, P = 0.280).
The diagnoses of hypercholesterolemia and diabetes were confirmed when serum cholesterol levels were ≥200 mg/dL and FBG levels were ≥126mg/dL, respectively (17,18).
The patients receiving therapy for diabetes and/or hypercholesterolemia were considered diabetic or hypercholesterolemic, respectively, even if their measurements were normal.
Obesity. Height and body weight of the participants were measured with a resolution of 5 mm for height and 100 g for weight. Body-mass index (BMI) was calculated for each participant by dividing body weight in kilogram by square of height in meters. Subjects having BMI values ≥30 kg/m2 were considered obese (19).
Waist circumference was measured by a plastic tape measure at the midline between the lower rib margin and the iliac crest in erect position at the end of a gentle expiration. Hip circumference measurements were done at the line between the great trochanters (20), and waist-to-hip ratios of the subjects were calculated. Abdominal obesity was diagnosed when the waist circumference was ≥94 cm for men or ≥80 cm for women. Values ≥102 cm for men and ≥88 cm for women were considered to be the critical point for obesity. Waist-to-hip ratios ≥0.95 in men and ≥0.80 in women were accepted as the indicator of abdominal obesity (21).
Smoking. The subjects were placed in one of the three following categories regarding their smoking behavior: current smokers, ex smokers, and never smokers (22).
Physical Activity. Occupational and leisure time physical activities were classified into 4 subcategories regarding the criteria used by Rotenbacher et al (23) and “Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance” (24). Participants were placed in one of the following categories regarding their physical activities:
Occupational physical activity: 1) sedentary – unemployed individuals or office workers, 2) light activity – housework, tailors, or secretaries; 3) medium activity – students, shop clerks, marketing people; 4) heavy activity – farmers, cleaning personnel, and manual workers, carriers.
Leisure time physical activity: 1) sedentary – mostly staying in the house; 2) light activity – working in the garden or walking; 3) medium activity – half an hour of sport activity (like aerobics) or 2 days per week; 4) heavy activity – sport activity (like aerobics) over half an hour and more than 3 days a week.
Data analysis
Data were analyzed on a database prepared on Statistical Package for the Social Sciences, version 13.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics is presented in the tables. χ2 tests were used to determine the differences between expected and observed frequencies in independent groups. We used t test and paired t test to compare the measurement values of two independent and dependent groups, respectively. Pearson correlation analysis was used to investigate the significance of the correlation between two measured variables. The level of significance for statistical analysis was set at P<0.05.
Results
Number of female and male participants was 477 (57.3%) and 363 (42.7%), respectively. Mean age ± standard deviation (SD) was 50.1 ± 12.6 (range, 30-77) years (Table 1).
Table 1.
Risk scores for developing coronary heart disease in the next decade in the study group according to socio-demographic characteristics*
| Characteristics | No. (%) | Mean risk score | P |
|---|---|---|---|
| Age: | |||
| 30-39 | 203 (23.9) | -1.7 ± 5.3 | <0.001† |
| 40-49 | 232 (27.3) | 4.7 ± 3.9 | |
| 50-59 | 184 (21.6) | 10.3 ± 3.3 | |
| 60-69 | 167 (19.7) | 12.4 ± 2.9 | |
| ≥70 | 64 (7.5) | 13.9 ± 3.0 | |
| Sex: | |||
| female | 487 (57.3) | 5.4 ± 7.9 | <0.001‡ |
| male | 363 (42.7) | 8.1 ± 4.6 | |
| Education: | |||
| none or only basic literacy skills | 209 (24.6) | 8.57 ± 4.52 | <0.001† |
| primary school | 468 (55.0) | 3.60 ± 6.06 | |
| secondary school or higher | 173 (20.4) | 1.54 ± 4.68 | |
| Health insurance: | |||
| insured | 684 (80.5) | 4.88 ± 5.89 | <0.001‡ |
| uninsured | 166 (19.5) | 2.75 ± 6.12 | |
| Perceived income: | |||
| low | 113 (13.3) | 4.63 ± 5.35 | 0.006† |
| sufficient | 224 (26.4) | 5.50 ± 4.73 | |
| high | 513 (60.4) | 3.98 ± 6.54 | |
| Total | 4.47 ± 5.99 |
*Risk scores (mean ± standard deviation) were calculated on the basis of age, history of smoking, systolic blood pressure, and cholesterol levels.
†One way ANOVA.
‡t test.
The distribution of patients according to chest pain and ECG findings can be seen in Table 2. The number of newly diagnosed and formerly unknown coronary heart disease cases was 126 (14.8%). Additionally, 82 (9.6%) individuals were suspected to have coronary heart disease (Table 3). Of 208 feedback forms sent to the hospitals to confirm or deny our coronary heart disease or possible coronary heart disease diagnoses, only 42 (20.2%) were returned. All the returned forms indicated that diagnoses were coronary heart disease and identical with ours. No feedback was obtained about remaining 84 coronary heart disease and 82 suspicious coronary heart disease cases.
Table 2.
Distribution of the participants according to the presence of chest pain and electrocardiogram findings
| Participants, No. (%) |
|||
|---|---|---|---|
| Diagnostic tool* | men | women | total |
| Rose Questionnaire: | |||
| no chest pain | 245 (67.5) | 323 (66.3) | 568 (66.8) |
| chest pain | 74 (20.4) | 39 (8.0) | 113 (13.3) |
| grade I | 62 (17.1) | 35 (7.2) | 97 (11.4) |
| grade II | 12 (3.3) | 4 (0.8) | 16 (1.9) |
| possible chest pain | 19 (5.2) | 48 (9.9) | 67 (7.9) |
| any kind of chest pain | 25 (6.9) | 77 (15.8) | 102 (12.0) |
| Electrocardiogram: | |||
| Q/QS (1.1 and 1.2) | 5 (1.4) | 8 (1.6) | 13 (1.5) |
| ischemia | 8 (2.3) | 9 (1.8) | 17 (2.0) |
| major abnormality | 5 (1.4) | 3 (0.6) | 8 (0.9) |
| minor abnormality | 3 (0.9) | 5 (1.0) | 8 (0.9) |
Table 3.
Distribution of participants according to having coronary heart disease and possible coronary heart disease*
| Participants, No. (%) |
|||
|---|---|---|---|
| Characteristics | men | women | total |
| Normal | 259 (71.3) | 383 (78.6) | 642 (75.6) |
| Coronary heart disease | 79 (21.8) | 47 (9.7) | 126 (14. 8) |
| AP with or without hypertensive heart disease | 75 (20.7) | 41(8.4) | 116 (13.7) |
| Old MI in electrocardiogram | 3 (0.8) | 6 (1.3) | 9 (1.0) |
| Congestive heart failure | 1 (0.3) | 0 (0.0) | 1 (0.1) |
| Possible coronary heart disease | 25 (6.9) | 57 (11.7) | 82 (9.6) |
| Possible angina pectoris | 19 (5.2) | 48 (9.9) | 67 (7.9) |
| Age >40 y and ischemia in ECG | 6 (1.7) | 8 (1.6) | 14 (1.6) |
| Age >60 y and LVH in ECG | - | 1 (0.2) | 1 (0.1) |
| Total | 363 (100.0) | 487 (100.0) | 850 (100.0) |
*Abbreviations: AP – angina pectoris; MI – myocardial infarction; LVH – left ventricular hypertrophy; ECG – electrocardiogram.
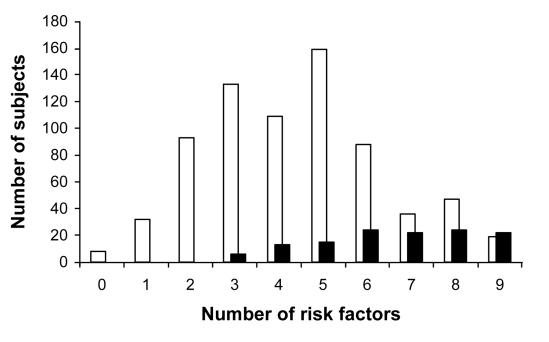
Mean coronary heart disease risk score was 6.6 ± 6.8. The scores increased with age until 60 years of age and the total mean risk score for men (8.1 ± 4.6) was significantly higher than that for women (5.4 ± 7.9) (P < 0.001, t test). The number of newly diagnosed stage I and II hypertension cases was 255 (30.4%). Diabetes was found in 70 (8.2%) participants. Hypercholesterolemia was revealed in 364 (43.4%) individuals who were unaware of this problem before (Table 4). Body mass index was over 30 kg/m2 in 315 (37.1%) subjects and waist/hip ratio was high in 106 (12.5%) cases (Table 5). The number of current smokers was 222 (26.1%). Occupational and leisure time physical activities were very low in 280 (32.9%) and 730 (85.9%) participants, respectively (Table 6). There was no coronary heart disease cases among individuals having less than 3 risk factors and 119 (84.9%) of coronary heart disease patients had at least 5 risk factors (Figure 1).
Table 4.
Distribution of participants according to blood pressure, serum glucose and cholesterol levels
| Participants, No. (%) |
|||
|---|---|---|---|
| Risk factor | men | women | total |
| Blood pressure in participants: | |||
| known to be normotensive: | 281 (43.4) | 367 (56.6) | 648 (76.2) |
| normal | 40 (14.3) | 98 (26.5) | 138 (21.3) |
| pre-hypertension | 143 (50.9) | 112 (30.6) | 255 (39.4) |
| stage I hypertension | 56 (19.9) | 78 (21.3) | 134 (20.7) |
| stage II hypertension | 42 (14.9) | 79 (21.6) | 121 (18.7) |
| known to be hypertensive: | 82 (40.6) | 120 (59.4) | 202 (23.8) |
| normal | 7 (8.6) | 8 (6.6) | 15 (7.4) |
| pre-hypertension | 11(13.4) | 5 (4.2) | 16 (7,9) |
| stage I hypertension | 11(13.4) | 14 (11.7) | 25 (12.4) |
| stage II hypertension | 53 (64.6) | 93 (77.5) | 146 (72.3) |
| Fasting blood glucose in participants: | |||
| known to have normal glucose: | 352 (43.3) | 460 (56.7) | 812 (95.5) |
| <126 mg/dL | 320 (90.9) | 422 (91.7) | 742 (91.4) |
| ≥126 mg/dL | 32 (9.1) | 38 (8.3) | 70 (8.6) |
| known to be diabetic: | 11 (28.9) | 27 (71.1) | 38 (4.5) |
| <126 mg/dL | 6 (54.5) | 16 (59.3) | 22 (57.9) |
| ≥126 mg/dL | 5 (45.5) | 11 (40.7) | 16 (42.1) |
| Serum cholesterol level in participants: | |||
| known to have normal cholesterol: | 352 (41.9) | 487 (58.1) | 839 (98.7) |
| <200 mg/dL | 173 (49.1) | 302 (62.0) | 475 (56.6) |
| ≥200mg/dL | 179 (50.9) | 185 (38.0) | 364 (43.4) |
| known to be hypercholesterolemic: | 11 (100) | - | 11 (1.3) |
| <200 mg/dL | - | - | - |
| ≥200 mg/dL | 11 (100) | - | 11 (100) |
Table 5.
Distribution of the subjects according to body mass index, waist circumference, and waist/hip ratio
| Participants, No. (%) |
|||
|---|---|---|---|
| Risk factor | men | women | total |
| BMI (kg/m2): | |||
| <18.5 | 5 (1.4) | 5 (1.1) | 10 (1.2) |
| 18.5-24.9 | 146 (40.2) | 112 (23.0) | 258 (30.4) |
| 25.0-29.9 | 133 (36.6) | 134 (27.5) | 267 (31.4) |
| 30.0-39.9 | 79 (21.8) | 203 (41.7)§ | 282 (33.1) |
| ≥40.0 | - | 33 (6.8) | 33 (3.9) |
| Waist circumference: | |||
| high* | 149 (41,0) | 335 (68.8)§ | 484 (56.9) |
| needs intervention† | 34 (22.8) | 257 (76.7)§ | 291 (60.1) |
| Waist/hip ratio: | |||
| high | 41 (11.3) | 65 (14.5)‡ | 106 (12.5) |
*Waist circumference ≥94 cm for men and ≥80 cm for women or waist/hip ratio ≥0.95 for men and ≥0.80 for women.
†Waist circumference ≥102 cm for men and ≥88 cm for women.
‡P = 0.400, χ2 test.
§P<0.001, χ2 test.
Table 6.
Distribution of the participants according to smoking behavior and physical activities
| Participants, No. (%) |
|||
|---|---|---|---|
| Characteristics | men | women | total |
| Smoking status: | |||
| never smoker | 90 (24.8) | 403 (82.8) | 493 (58.0) |
| ex smoker | 118 (32.5)† | 17 (3.5) | 135 (15.9) |
| current smoker | 155 (42.7)† | 67 (13.7) | 222 (26.1) |
| Occupational physical activity: | |||
| sedentary | 109 (30.0) | 171 (35.1)* | 280 (32.9) |
| light | 111 (30.6) | 251 (51.6) | 362 (42.6) |
| medium | 106 (29.2)† | 42 (8.6) | 148 (17.4) |
| heavy | 37 (10.2)† | 23 (4.7) | 60 (7.1) |
| Leisure time physical activity: | |||
| sedentary | 288 (79.4) | 442 (90.8) | 730 (85.8) |
| light | 60 (16.5)† | 45 (9.2) | 105 (12.4) |
| medium | 15 (4.1)† | - | 15 (1.8) |
*P<0.05 (0.03), χ2 test
†P<0.001.
Figure 1.
Distribution of formerly undiagnosed (missed), but newly diagnosed coronary heart disease (black columns) cases and normal participants (white columns) according to number of risk factors they have.
For patients who attended to primary health care, the estimated percentage risk for developing coronary heart disease in the next 10 years was 7 to 45% in men and 2 to 45% in women.
Discussion
Our study demonstrated that there were missed opportunities to diagnose coronary heart disease in patients with cardiovascular problems in primary care settings. In Turkey, individuals who seriously suspect to have heart related problems may apply directly to secondary health care centers and they have a chance to be diagnosed, treated, or warned about the risks they have. However, people who are seen by primary or maybe secondary health care providers from disciplines irrelevant to cardiology remain unaware of the disease or risks they have. Approximately one fourth of our participants who considered themselves free of cardiovascular problems or related risks after being seen by a physician were suddenly diagnosed with coronary heart disease or possible coronary heart disease after a short reevaluation. This is a dramatic indicator of a dysfunction in health care services.
The prevalence values of coronary heart disease and its risk factors in our study group were higher than those of general Turkish population (15,25), because we studied the patients with at least one health complaint.
There may be several reasons for missing the opportunities of determining coronary heart disease and related risk factors in primary care. In our opinion, an enormous caseload is the first reason. In the setting of our study, one physician is responsible for the care of nearly 4000 patients which presents an extremely higher caseload than is the case in developed countries (26). As a consequence, physicians have to restrict themselves to responding to presented health problems rather than searching for hidden possibilities. Another reason may be a common misperception among primary care providers, even among health administrators, that cardiovascular disorders should be dealt within secondary care settings. This misperception may cause among primary care providers a strong reluctance to deal with coronary heart disease and an ill working referral system between primary and secondary care. This reluctance is further increased by the possibility of direct applying to any level of health system. On the other hand, even if some primary care physicians really want to deal with this disease, there is no practical guideline available for them in Turkey. Unfortunately, coronary heart disease does not take part in the “Diagnosis and Treatment Guide for Primary Health Care” published by the Turkish Ministry of Health (9). The lack of required equipment like electrocardiographs or effective laboratories in primary care centers may be another reason for missing diagnoses. Although performing ECG and laboratory tests in primary care in every patient is both difficult to achieve an and cost-effective, involving the Rose questionnaire in routine history taking procedure can help the primary care physicians reveal coronary symptoms. Suspected cases determined by the Rose questionnaire may then be evaluated by ECG and laboratory tests or referred to secondary care institutions. Lack of feedback from secondary care about many of the referred patients – as shown in our study – may be another contributing factor for primary health care providers to refrain from coronary heart disease related issues.
Our results also showed that a considerable number of previously diagnosed diabetes, hypercholesterolemia, or hypertension cases are not under control despite receiving medical therapy. This indicates that it is not enough to determine the people under risk, but to provide an effective follow-up and intervention.
The limitation of our study is that it comes from a single primary care center. We cannot be sure that this center is representative of all primary care institutions in the country. Similarly designed but more comprehensive study should be conducted in order to provide more reliable results. Another major limitation is a lack of feedback from hospitals to confirm the diagnosis in two thirds of the coronary heart disease and all of the suspicious coronary heart disease patients. Receiving feedback seems to be possible in nearly one fifth of the referred cases. This low returning rate is an indicator of bad communication between different levels of the health system in Turkey. According to literature, some other countries also suffer from similar communication problems in their health systems (27,28).
In conclusion, our study confirmed the hypothesis that opportunities to reveal unknown coronary heart disease cases and related risk factors in primary care could be missed due to problems such as bad referral system between different levels of health system or high caseload. In order to reduce the number of missed cases, responsibility and importance of primary care should be emphasized by training people and health professionals and by establishing a working referral and communication system between different levels of health services. Current caseload in primary care should be lowered to increase the effectiveness of physicians. Although relevant practical guidelines and basic technical equipments are needed to increase the autonomy of primary care institutions in dealing with coronary heart disease and its risk factors, some measures such as smoking cessation programs or interventions concerning overweight people could be taken without any equipment. Such measures also increase the effectiveness of following-up individuals at risk. Further community based studies are needed to provide more comprehensive and real community based proposals.
Acknowledgment
The authors are grateful to the staff of primary health care center for their help in conducting this study. We give special thanks to Cengiz Ermis, Babur Dora, and Ozgur Tosun for their constructive comments and suggestions on early drafts of the manuscript. Akdeniz University Scientific Research Management Unit provided funding for this study.
References
- 1.Poulter N. Global risk of cardiovascular disease. Heart. 2003;89(Suppl 2):ii2–5. doi: 10.1136/heart.89.suppl_2.ii2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. CVD prevention and control: missed opportunities. Available from: http://www.who.int/cardiovascular_diseases/prevention_control/en/ Accessed: January 24, 2005.
- 3.World Health Organization. WHO CVD risk management package for low and medium resource settings. Geneva (Switzerland). World Health Organization; 2002. Available from: http://whqlibdoc.who.int/publications/2002/9241545852.pdf. Accessed: August 1, 2003.
- 4.Hutchison B, Birch S, Evans CE, Goldsmith LJ, Markham BA, Frank J, et al. Screening for hypercholesterolaemia in primary care: randomised controlled trial of postal questionnaire appraising risk of coronary heart disease. BMJ. 1998;316:1208–13. doi: 10.1136/bmj.316.7139.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brindle P, Fahey T. Primary prevention of coronary heart disease. BMJ. 2002;325:56–7. doi: 10.1136/bmj.325.7355.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brindle P, Emberson J, Lampe F, Walker M, Whincup P, Fahey T, et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003;327:1267. doi: 10.1136/bmj.327.7426.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dirican RM. Community medicine (Public Health) courses [in Turkish]. Ankara: Hatipoglu Yayinevi; 1990. p. 10-12. [Google Scholar]
- 8.The Hacettepe Institute of Population Studies (HIPS). Turkish Demographic and Health Survey (TDHS-1998). Ankara: Measure DHS+ Macro International Inc. 1999. [Google Scholar]
- 9.Turkish Ministry of Health. Diagnosis and treatment guidelines for primary health care [in Turkish]. Ankara: Saglik Projesi Genel Koordinatorlugu; 2002. [Google Scholar]
- 10.Turkish Ministry of Health. Non-communicable disease control program. Available from: http://www.antalyasm.gov.tr/proje/socak.htm. Accessed: May 16, 2007.
- 11.Primary Health Care Center Records. Antalya: June 2003. (Official record).
- 12.Lip GY, Nadar S. Atherosclerosis and coronary artery disease risk factors. In: Grobbee DE, Lip GY, editors. Risk factor management in coronary artery disease. Barcelona (Spain): Grafos S.A. Arte sobre papel; 2003. p. 9-17. [Google Scholar]
- 13.Turkish Society of Cardiology. Onat A, editor. Guidelines on management of coronary heart disease [in Turkish]. Istanbul (Turkey): Turk Kardiyoloji Dernegi; 1998. p. 15-30. [Google Scholar]
- 14.Rose GA, Blackburn H. Cardiovascular survey methods. Geneva: WHO; 1968. p. 137-72. [Google Scholar]
- 15.Onat A, Senocak MS, Surdum-Avci G, Ornek E. Prevalence of coronary heart disease in Turkish adults. Int J Cardiol. 1993;39:23–31. doi: 10.1016/0167-5273(93)90293-p. [DOI] [PubMed] [Google Scholar]
- 16.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 17.May HT, Muhlestein JB, Carlquist JF, Horne BD, Bair TL, Campbell BA, et al. Relation of serum total cholesterol, C-reactive protein levels, and statin therapy to survival in heart failure. Am J Cardiol. 2006;98:653–8. doi: 10.1016/j.amjcard.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization Department of Non-communicable Disease Management. Screening for type II diabetes. Report of World Health Organization and International Diabetes Federation Meeting. Geneva (Switzerland): World Health Organization; 2003. p. 29-35. [Google Scholar]
- 19.World Health Organization Expert Committee. Physical status: the use and interpretation of anthropometry. WHO Technical Report Series No.: 854. Geneva (Switzerland): World Health Organization; 1995. [PubMed] [Google Scholar]
- 20.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adult. NIH Publication No.: 98-4083. Bethesda (ME): National Institutes of Health; 1998. p. 178. [Google Scholar]
- 21.Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–61. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Guidelines for the conduct of tobacco smoking survey of the general population. Geneva: World Health Organization; 1982. WHO/SMO/83.4. [Google Scholar]
- 23.Rothenbacher D, Hoffmeister A, Brenner H, Koenig W. Physical activity, coronary heart disease, and inflammatory response. Arch Intern Med. 2003;163:1200–5. doi: 10.1001/archinte.163.10.1200. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system. Atlanta (GA): 2002. Available from: http://www.cdc.gov/brfss Accessed: March 24, 2005.
- 25.Satman I, Yilmaz T, Sengul A, Salman S, Salman F, Uygur S, et al. Population-based study of diabetes and risk characteristics in Turkey: results of the turkish diabetes epidemiology study (TURDEP). Diabetes Care. 2002;25:1551–6. doi: 10.2337/diacare.25.9.1551. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Highlights on health. Available from: http://www.euro.who.int/eprise/main/WHO/Progs/CHHNET/annex/20041126_5 Accessed: September 1, 2006.
- 27.Griffo R, Blondett M, Stellini F, Camerini A, Picciotto R. Implementing cardiovascular prevention in the real world: presentation of an integrated hospital-field model. Monaldi Arch Chest Dis. 2003;60:155–60. [in Italian] [PubMed] [Google Scholar]
- 28.Kordy MN, Ibrahim MA, al-Gamal FM, Bahnassy A, Milaat W. A study of the morbidity pattern of referred patients and the effectiveness of the referral system in primary health care centers. J Egypt Public Health Assoc. 1992;67:709–24. [PubMed] [Google Scholar]