Abstract
Background
Cutaneous spider naevi are commonly considered to be a clinical sign of chronic liver disease. Little is known about their occurrence in children.
Aim
To evaluate the occurrence of spider naevi in children with and without liver disease.
Methods
The presence of spider naevi was investigated in 460 children, 34 of whom had chronic liver disease.
Results
Of children without liver involvement, 38% had at least one spider naevus. The prevalence of spider naevi increased with age. Of control patients aged 5 to 15 years, 2.5% had more than five spiders present. Although eight of 10 children with cirrhosis had at least one spider naevus, only four of 34 children with chronic liver disease had five or more spiders present. Most spiders were on the hands and very few were >5 mm in size.
Conclusions
Children with liver disease rarely have large numbers of spider naevi. Although the finding of five or more spider naevi is more common in liver disease, many normal children also have one or more of these lesions.
Keywords: child, chronic liver disease, spider naevus
Spider naevi (fig 1), also known as spider angiomas or vascular spiders, are commonly associated with chronic liver disease in adults.1 Over the years spiders in adults have been linked with cirrhosis from a variety of causes, but especially alcoholic cirrhosis.1,2,3,4 Although Wenzl and Burgert reported on the occurrence of spider naevi in children 40 years ago,5 the frequency with which they occur in normal children is not widely recognised,6,7 and their relative abundance in children with liver disease has not been studied. Our aim in this study was to examine the occurrence of spider naevi in children with and without chronic liver disease.
Methods
Children aged 1 to 15 with liver disease (excluding those who had undergone liver transplantation) attending the National Children's Liver Unit at Our Lady's Hospital for Sick Children in Dublin, and children without liver involvement attending general paediatric outpatient clinics or inpatients with a variety of conditions in the same hospital, were examined for the presence of spider naevi. The number of naevi, their size and location, and the presence or absence of liver disease, the underlying diagnosis, and other relevant clinical signs were noted. Children without liver disease were divided on an a priori basis into three groups according to their age (1–5 years; 5–10 years, and 10–15 years).
Results
In all, 528 children were examined, 260 boys and 268 girls. Sixty eight children were excluded, mostly because of age <1 year or >15 years, or inadequate documentation. Thus 460 patients were eligible for the study: 34 with chronic liver disease and 426 without liver involvement.
Figure 1 Typical small spider naevus on the forearm of an otherwise healthy 7 year old boy. Consent was obtained for publication of this figure.
Children without liver disease
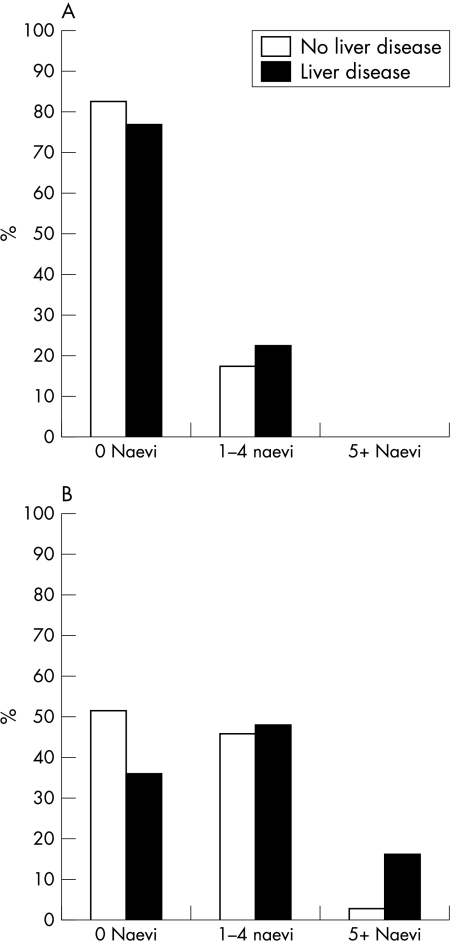
Thirty eight per cent of the children (n = 162) without any evidence of liver disease had at least one spider naevus present, with most having between one and four. However, seven children (1.64%) had more than five spider naevi. There were no differences between boys and girls in terms of numbers of spiders found (data not shown). The prevalence of spider naevi increased with age (fig 2). For example, among children aged 1–5 years, only 25 of 142 (17.6%) had any spiders and none had five or more. In contrast, 77 of 163 (47.2%) of those aged 5–10 years and 60 of 121 (49.6%) of those aged 10–15 years had spiders present. The difference in the occurrence of spider naevi in those aged 1–5 years compared with those aged over 5 years was significant (odds ratio (OR) = 4.79, p = 0.001). Approximately 2.5% of those over 5 years had five or more naevi (fig 2B). The maximum number of spiders in any child without liver disease was 11.
Figure 2 (A) Spider naevi in children aged 1–5 years. (B) Spider naevi in children aged 5–15 years.
Children with chronic liver disease
The specific diagnoses among 34 children with chronic liver disease included autoimmune hepatitis, α1‐antitrypsin deficiency, cystic fibrosis associated liver disease, and progressive familial intrahepatic cholestasis. Ten of these patients had cirrhosis and three were cholestatic. Forty seven per cent had no spider naevi present and only four of 34 (11.8%) had five or more naevi. It is noteworthy that of the nine children under the age of 5 years with chronic liver disease, none had more than five spider naevi. In children with liver disease overall, two of nine 1–5 year olds (22%), six of 11 5–10 year olds (55%), and 10 of 14 10–15 year olds (71%) had at least one spider. Only three of 10 children with fibrosis/cirrhosis had more than five spiders present.
In general, most spiders were found on the hands, regardless of the presence or absence of liver involvement. Of spiders graded for size (n = 354 in controls; n = 104 liver disease), more than two thirds in both groups were less than 2 mm in diameter. However, larger spiders (>5 mm) were more common in children with liver involvement than in those without (13.4% v 6.5%, OR = 2.06).
Discussion
For the practising paediatrician this study helps to address two clinical questions that commonly arise: first, do otherwise well children with several spider naevi need to be extensively investigated for the presence of liver disease? And second, in the evaluation of children with suspected liver disease are spider naevi a good marker of chronicity?
What is already known on this topic?
Cutaneous spider naevi are considered a marker of chronic liver disease in adults
The relative occurrence of spider naevi in children with and without liver disease has not been studied
What this study adds
Multiple (>5) spider naevi may be present in otherwise well children without liver disease
Most children with chronic liver disease appear to have few or no spider naevi
With regard to the clinical relevance of spiders in otherwise normal children, we have shown that a small proportion of the paediatric population can have a substantial number of spider naevi without any evidence of liver disease. It is important to recognise that the children in this study with more than five spider naevi (one of them had 11) had no other clinical evidence of liver disease. Four had normal liver biochemistry and one who was followed up for three years has not developed liver disease. Therefore, we feel the presence of multiple spider naevi in an otherwise well child with a normal physical examination can be a normal finding and may not warrant extensive laboratory or radiological investigation for underlying chronic liver disease.
With regard to the issue of whether spider naevi provide a useful marker of chronicity in those suspected of liver disease, our data suggest that the majority of children with established chronic liver disease will not have large numbers of spider naevi, especially those aged less than 5 years. Therefore, although spider naevi should be sought in those with suspected liver involvement, the presence and quantity of these lesions may not be a sensitive marker of underlying chronic liver disease.
Footnotes
Competing interests: none declared
Consent was obtained for publication of figure 1.
References
- 1.Bean W B. The cutaneous arterial spider: a survey. Medicine 194524243–331. [Google Scholar]
- 2.Li C P, Lee F Y, Hwang S J.et al Spider angiomas in patients with liver cirrhosis: role of vascular endothelial growth factor and basic fibroblast growth factor. World J Gastroenterol 200392832–2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li C P, Lee F Y, Hwang S.et al Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function. Scand J Gastroenterol 199934520–523. [DOI] [PubMed] [Google Scholar]
- 4.Witte C L, Hicks T, Renert W.et al Vascular spider: a cutaneous manifestation of hyperdynamic blood flow in hepatic cirrhosis. South Med J 197568246–248. [PubMed] [Google Scholar]
- 5.Wenzl J E, Burgert E O. The spider naevus in infancy and childhood. Paediatrics 196433227–233. [PubMed] [Google Scholar]
- 6.Gill D, O'Brien N.Paediatric clinical examination, 4th edition. London: Churchill Livingstone, 200311225 [Google Scholar]
- 7.Darmstadt G. The skin. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson's textbook of pediatrics, 16th edition. Philadelphia: WB Saunders, 20006561978 [Google Scholar]