Summary
FOXP3 is probably the best marker available currently for identifying natural regulatory T cells (Tregs) in mice and humans. Evidence from mouse literature suggests that natural FOXP3+ Tregs are formed in the thymus and expand in the periphery to contribute significantly to peripheral Tregs. In this review, we discuss recent reports that show that, in humans, the formation of FOXP3+ Tregs is a natural consequence of T cell activation and that de-novo peripheral generation of FOXP3+ Tregs is a much more dominant source of circulating Tregs than natural thymically derived Tregs. We also suggest that the role of Tregs in human diseases must be reviewed in light of these new findings and great caution should be exercised in immunotherapeutic interventions that involve the modulation or generation of putative Tregs.
Keywords: Regulatory T cells, Activated T cells, FOXP3, CD4, CD8, Human, adaptive Tregs
Introduction
Regulation of the immune system is a key concept in immunology. In recent times, many cell types have been shown to possess the capacity to regulate immune responses, including the CD4+CD25high regulatory T cells (“Tregs”), CD4+ Tr1 cells, CD4+ Th3 cells, CD8+CD28− T cells, CD4−CD8− T cells and NKT cells, among others [1]. The mechanisms of suppression are incompletely understood and seem to vary considerably between the various subsets and also between in vivo versus in vitro conditions [2].
One of the best-characterized subsets of immune regulatory cells is the CD4+CD25+/high Tregs. In mice, FOXP3 appears to have emerged as the definitive marker for such Tregs [3]. Recent studies have also elucidated the molecular mechanisms underlying the suppression by FOXP3, which involves repression of NFAT and NFκB and consequently IL-2 secretion [4,5].
However, in humans the significance of FOXP3 is complicated by the knowledge that CD4+CD25−FOXP3− T cells can be induced to express FOXP3 simply on activation [6]. This may also happen in mice under certain conditions such as the presence of TGFβ or low dose antigenic stimulation [7,8]. This phenomenon raised the important question whether Tregs are formed in the thymus and then persist/expand in the periphery or whether they can be induced de novo in the periphery during antigen-specific stimulation. While in mice the former mechanism has been shown to be important [9], recent reports from human studies provide strong support for the latter mechanism with an intrinsic connection between effector and regulatory functionality as different states of differentiation. Modulation of Tregs as well as their generation are being proposed as therapeutic interventions in several disease settings [10], sometimes with disastrous consequences [11]. Therefore, a thorough understanding of the unique biology of human Tregs is crucial for the correct interpretation of published and unpublished data, before therapeutic interventions can be undertaken. For example, based on FOXP3 expression or in vitro regulatory activity, Tregs (envisioned as a stable population of cells involved purely in immune regulation) are hypothesized to be involved in various human diseases from cancer and infections to autoimmunity, allergy and asthma [12–16]. A great deal of this evidence might be explained by the fact that all of these diseases involve immune activation during their pathogenesis and FOXP3+ T cells with regulatory activity may be a transient form attained during the activation of regular effector T cells. Thus, Tregs that are cross-sectionally enumerated in these diseases may be neither a unique nor a stable population.
FOXP3 expression by all T cells during activation
Induction of FOXP3 on activation of human CD4+CD25− T cells in vitro was first noted in studies from the laboratory of Ziegler, SF as early as 2003 [17,18]. However, at that time it was widely thought that the induced FOXP3+ T cells are expanded from contaminating regulatory T cells in the starting population [3,19–21]. Development of flow cytometric antibodies against FOXP3 has allowed us to exclude that possibility and confirm earlier findings that FOXP3 can indeed be expressed on activated CD4+ T cells [22]. Most importantly, we noted that FOXP3 expression was not unique to a subset of activated cells. Rather, every T cell that gets activated goes through a phase of FOXP3 expression [23–25]. Moreover, any mode of activation appeared to induce such expression, including anti-CD3, allogeneic stimulation as well as antigen-specific stimulation [23]. Culturing human or mouse CD25− T cells in the presence of TGF-β results in the production of FOXP3+ T cells [7,26]. This had led some to suggest that presence of exogenous TGF-β in human serum used for culturing cells is responsible for FOXP3 expression by activated T cells. However, our studies using serum-free media (X-vivo) or anti-TGF-β in serum-containing cultures show essentially similar dynamics of FOXP3 expression (unpublished data). It is possible that TGF-β secreted by stimulated T-cells or other immune cells may mediate the induction of FOXP3 expression [27]. Importantly, if traces of TGF-β present in body fluids or made by other immune cells are responsible for such FOXP3 induction, it could be argued that this may be very relevant during in vivo T-cell activation.
It still remains somewhat controversial whether these activated FOXP3+ T cells represent suppressive Tregs. Rapid downregulation of FOXP3 in activated T cells have led some to question the suppressive capability of these induced FOXP3-expressing cells without even performing suppression assays on these populations [25,28]. In some studies, use of bulk cultures in suppression assays has failed to show suppressive activity in such activated cultures [24]. However, such bulk cultures contain a significant proportion of non-activated, non-proliferating T cells, as revealed by the incorporation of CFSE staining in these assays. Upon purification of either CD25+ cells or proliferating cells (CFSE-low) from these cultures, suppressive activity can be definitively demonstrated in these induced FOXP3+ T cells [23]. Other studies have also corroborated that transient induction of FOXP3 by activation in human T cells does confer regulatory properties to those cells [6,17,18,24,29,30]. These observations raise the possibility that expression of FOXP3 and regulatory activity might just be a step in the activation of all human T cells [23]. Transient acquisition of suppressive activity during activation might be a mechanism of limiting excessive immune activation and damage at the site of inflammation.
A majority of the activated cells that express FOXP3 eventually downregulate FOXP3 expression, corresponding to a diminution in their suppressive ability. However, a small percentage of these cells continue to sustain FOXP3 expression. Such residual FOXP3 expression was seen under all activation conditions even 15–20 days post stimulation. This residual Treg population was probably responsible for some suppressive ability in these relatively long-term cultures. Of course, it still remains to be seen whether FOXP3 expression is merely coincident with the suppressive ability of Tregs or is causally linked. It is entirely possible that FOXP3-independent pathways are involved in the mechanism of suppression [29]. Regardless of the mechanism, it appears that such transient upregulation of FOXP3 and regulatory ability, followed by sustenance of such ability in a smaller proportion of cells may be a way of generating Tregs in the periphery following antigen stimulation. This mechanism would also ensure that Tregs would have a very broad reactivity against self and foreign antigens.
A recent report examining the dynamics of TGF-β-induced FOXP3+ T cells using GFP-FOXP3 knock-in mice has made interesting observations [26]. These mice allow clear distinction of induced and natural Treg populations. It was found that the induced Tregs are very similar to natural Tregs in cytokine and suppression profile. Loss of FOXP3 resulted in loss of suppressive capability in induced Tregs. When induced Tregs were transferred into naïve mice it was found that though most of them downregulated FOXP3, while a certain percentage of these cells continued to persist and were very similar to natural Treg populations. These observations are very similar to what we have reported about FOXP3-expressing T cells in humans. Thus, some of the dynamics of activated human T-cells may be similar to TGF-induced mouse Tregs.
In the mouse thymus it has been noted that cells with the highest affinity go on to become FOXP3+ Tregs [31]. Similar mechanisms might operate in the periphery during activation wherein responding cells with the highest affinity/avidity may contribute to the population of circulating regulatory T cells. Supporting this idea, a recent study using MHC class II tetramers and activation analysis to detect autoantigen-specific T cells in the peripheral blood of type I diabetes mellitus patients found that the high avidity T cells preferentially acquired regulatory features compared to the low avidity T cells [32].
Natural Tregs have been shown to be anergic in proliferation and cytokine secretion in vitro, but the same may not be true in vivo [33]. An important observation is that suppressive activity of induced FOXP3+ T cells is coincident with effector activity. Induced FOXP3+ cells have the ability to secrete some effector cytokines such as TNF-α [23]. The ability to secrete cytokines has been interpreted previously to mean that they do not have regulatory properties [25,28]. However, we believe that regulatory activity and effector function can co-exist in the same cell at the same time and mere presence of some effector function does not automatically exclude regulatory functionality. Such a cell possessing dual function of suppressor and helper activity has been described during the earlier incarnation of Tregs as suppressor T cells during the 1970’s [34]. Recent evidence from mouse models also shows that effector function can co-exist with FOXP3 expression and regulatory activity. A recent report clearly showed that FOXP3+ T cells can co-express the pathogenic cytokine IL-17 and that IL-17 cells can be double positive for FOXP3 and IL-17 during their formation [35]. This report also showed that FOXP3+ Tregs could be converted into stable IL-17 expressing T cells in the presence of IL-6 and absence of TFG-β. Another study has reported that IFN-γ can be expressed by Tregs in vivo in a demyelinating disease model [36].
Peripheral generation/persistence of Tregs
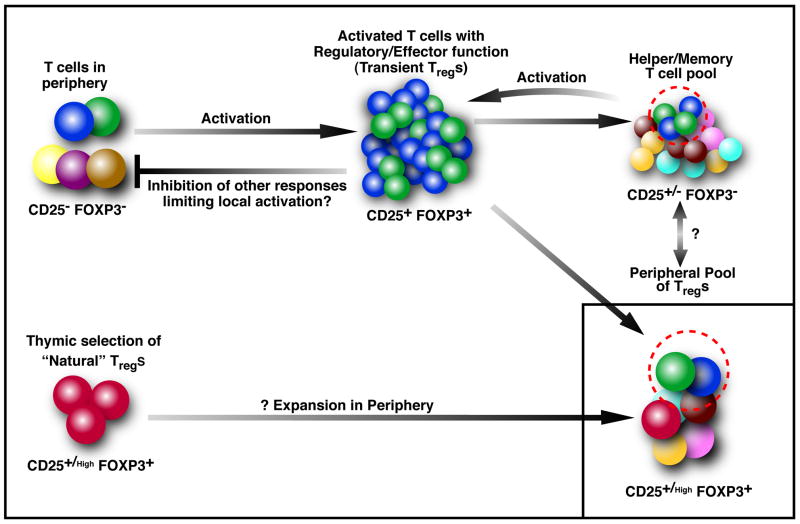
Even though a clear distinction is commonly made between natural thymically generated Tregs and induced Tregs, so far there is no clear marker that can distinguish them in humans. Although there is strong evidence in mice regarding the thymic origin of the regulatory T cells, there is little evidence for their thymic origin in adult humans. In fact, it is not even clear if they are functionally distinct subsets. In mice, it is conceivable that natural Tregs might play an important role in controlling immune responses during the short life span of a mouse housed in a controlled environment. However, the same cannot be extrapolated to humans with their long life spans, early thymic involution and continual antigenic exposure during a lifetime. Thus, it seems rather unlikely that a small subset of thymically generated Tregs would persist throughout the lifespan of humans without any peripheral induction or expansion of naturally derived Tregs. Key evidence for the peripheral generation of Tregs comes from an elegant study from the laboratory of Akbar AN, in which a novel deuterium labeling method was used to determine how human Tregs are generated or persist in the periphery [37,38]. Human Tregs were found to be a rapidly proliferating population compared to naive or memory T cells, but were short-lived and underwent apoptosis at a far higher rate than naive or memory cells. Hence, they concluded that thymically generated Tregs or expansion of natural Tregs cannot explain lifelong persistence of human Tregs, especially with the observation that Treg numbers do not decline with age [37]. Thus, most of the Tregs must be constantly produced in the periphery from a non-thymic source. When they compared the TCR repertoires of CD4+CD45RO+CD25hi and CD4+CD45RO+CD25− populations, they found striking similarity in the breadth of Vβ usage between the two populations. Furthermore, it was also determined that there was close clonal homology between the two populations suggesting that they are derived from the same precursor population. Interestingly, Vβ usage in CMV-specific T cell populations was similar between memory T cells and FOXP3+ regulatory T cell populations, suggesting that they were formed from the same precursor population at the same time during an anti-CMV immune response in the body. Taken together with the in vitro data, this supports a model where, during an antigen-specific response, all activated T cells attain a FOXP3+ regulatory state, with the potential to persist as Tregs (see Figure 1). However, only a small subset persists with this phenotype and contributes to the circulating Treg pool. Most cells downregulate FOXP3, probably contract in numbers and reside in the memory pool, only to repeat this process during re-exposure. It is still unclear whether cells from these two pools can interconvert in vivo, an important issue that needs to be addressed in future studies. In addition, more studies are required to ascertain the relative contribution of peripheral versus thymically derived Tregs in adult humans.
Figure 1. A model of peripheral Treg formation in adult humans, as a consequence of activation.
Every time there is activation of T cells in the periphery, the responding T cells upregulate FOXP3 and CD25 transiently. This is associated with transient suppressive activity and also some effector functions. The suppressive activity may serve to inhibit untoward responses from lower affinity/potentially cross-reactive T cells. During the response, only a subset of these activated T cells retain FOXP3 and contribute to the peripheral pool of FOXP3+ Tregs, persisting for longer periods in the FOXP3+ suppressive state. The majority of the activated cells downregulate FOXP3, contract in numbers and contribute to the peripheral memory pool. Such memory cells have the potential to contribute to the peripheral Treg pool in future activation cycles. Of note, the T cell receptor distribution of the memory pool and the Treg pool are similar, suggesting common precursors. It is still unclear whether there is direct conversion of “stable” Tregs into memory and/or effector cells in vivo. In the thymus, positive selection of T cells with intermediate affinity for self antigens results in the formation of a population of natural FOXP3+ Tregs. While these may be a major source of peripheral Tregs in mice and probably in human infants, most of these may not persist during adult life in humans. Thus, peripherally generated Tregs with diverse antigenic specificities are the major source of circulating Tregs in adult human beings.
Presence of FOXP3+ T cells at inflammatory sites and during chronic infections suggests the in vivo relevance of these mechanisms. Various immunomodulatory therapies such as glatiramer acetate therapy for multiple sclerosis, allergen injections for allergic rhinitis and venom anaphylaxis have also been known to induce various forms of regulatory T cells, suggesting potential peripheral de novo origin of these cells [39–41]. It remains to be seen whether in vivo FOXP3+ T cells indeed downregulate FOXP3 and, more importantly, what factors/mechanisms are involved in their stable sustenance versus phenotypic reversal [42].
Transient formation of CD8+FOXP3+ Tregs during activation
Though FOXP3 expression is associated with CD4+ Tregs, it is very interesting to note that CD8+ T cells have also been shown to express FOXP3 [22,23,28,30,43,44]. CD8+FOXP3+ T cells with contact-dependent suppressive activity were induced in type 1 diabetes patients treated with a modified anti-CD3 monoclonal antibody [30]. The CD8+ Tregs were able to mediate contact dependent suppression of CD4+ T cells in-vitro to both antigen-specific and non-specific stimulation. A longitudinal study revealed increased numbers of CD8+FOXP3+ T cells in treated patients compared to untreated controls after 12 days of anti-CD3 mAb treatment. Some CD8+FOXP3+ T cells were found to persist even 12 weeks after treatment. The presence of these cells is direct evidence for the induction and persistence of FOXP3+ T cells on activation in vivo. It remains to be seen if the CD8+FOXP3+ T cells possess any cytotoxic function besides the direct suppressive function. For example, we have observed the induction of cytotoxic, suppressive CD8+ T cells during chronic treatment of multiple sclerosis with glatiramer acetate [39,45].
CD8+CD28−FOXP3+ T cells are known to be formed under conditions of allostimulation in human transplant patients [44]. However, they seem to suppress by upregulation of immunoglobulin like transcripts ILT-3 and 4 on APCs [46,47]. But why do CD8+ T cells in the PBMC of healthy volunteers express scant FOXP3 or even CD25 for that matter compared to CD4+ T cells in the periphery? One would expect them to show similar levels of FOXP3 and CD25 expression since their kinetics of CD25 and FOXP3 expression after stimulation are similar. It is possible that most of the FOXP3 expressing CD8+ T cells are short lived and undergo apoptosis or they may persist at the site of activation. These issues regarding the biology of CD8+ Tregs still need to be sorted out.
Similarities between activated T cells and Tregs
Tregs have been associated with multiple markers including CD25, CTLA-4, GITR, CD69, CD44, FOXP3 and more recently downregulated CD127 [21,48]. Despite intensive research over the last few years there are still no surface or intracellular markers, which clearly distinguish Tregs from activated T cells in humans. Even the pattern of the most promising markers like FOXP3 and low CD127 can be mimicked by activated T cells [23]. A recent study looking at micro RNAs expressed by regulatory T cells also determined that both Tregs and activated T cells have very similar micro RNA expression profiles suggesting that even their regulation at the mRNA level might be similar [49]. Activation through TCR is closely linked to the suppressive activity. It is known that specific or non-specific TCR stimulation is necessary for suppression by Tregs in in vitro cultures [31]. Activation through TCR was found to be necessary for FOXP3 binding and repression by histone deacetylation of the IL-2 and IFNγ locus in T cells [50]. Recent reports analyzing genome wide targets of FOXP3 using CHIP to chip assays determined that FOXP3 represses and activates key genes involved in T cell activation [51,52], further evidence of the close relationship between T cell activation and acquisition of suppressive capability. Hence, serious consideration should be given to accumulating evidence that circulating human Tregs may be a form of activated T cell, merely representing a peripheral state of differentiation with different functionality.
Thus, while there appear to be clear differences in the intracellular signaling pathways in a resting T-cell and a Treg, it is possible that once an activated T-cell expresses FOXP3, pathways similar to Tregs also get activated, causing them to have similar functions. The precise gene expression and biochemical differences, if any, between transient FOXP3-expressing activated T-cells and ex vivo Tregs have yet to be elucidated.
Revisiting Tregs in human disease and therapy
In light of these emerging concepts regarding the biology of human Tregs, it is prudent to re-interpret existing data regarding the involvement of regulatory T cells in human diseases and to rephrase the important issues that need to be addressed before delving into therapeutic modulation.
Tregs are hypothesized to be involved in multiple clinical scenarios such as autoimmune disorders, asthma, cancer and infection. Tregs isolated from patients with various autoimmune diseases, such as multiple sclerosis [53,54], myasthenia gravis [55], psoriasis [56] and autoimmune polyglandular syndrome type II [57] have a reduced capacity to suppress compared to Tregs from healthy individuals, while the total Treg numbers are comparable. Could this reduced ability reflect the proportion of transient versus stable Tregs in the ex vivo population? It is tempting to speculate that when a healthy immune system encounters autoantigens (or cross-reactive exogenous antigens), it maintains a robust population of autoantigen-specific Tregs during such a response. In contrast, autoantigen-specific responses in autoimmune conditions may result in a more interchangeable, transient formation of effector/Treg cells. This raises concerns about therapies that are targeted toward in vivo or in vitro generation of Tregs. In such approaches, it is not enough simply to show FOXP3 expression and an in vitro suppressive ability of a preparation of T cells. Rather, it is critical to evaluate the stability of such a phenotype to avoid disastrous consequences. For example, protocols to expand/induce Tregs either in a non-specific or antigen-specific manner tend to use anti-CD3, anti-CD28, IL-2, TGF-β or modified DC [30,58–60]. In all approaches, T cells are essentially being activated, which we now know can lead to a transient formation of FOXP3+ regulatory T cells. The key issue is to dissect how this phenotype may be sustained in vitro and, even more so, in vivo (where there is an inherent danger of apoptosis and/or loss of function on one end, or even a reversal to a pathogenic function at the other extreme). Such an unfortunate sequence of events may have been exemplified by the recent anti-CD28 super agonist (TGN1412) trial where attempts to expand Tregs in humans, based on in vitro FOXP3 and suppression readouts, ended in untoward consequences [61], including a massive cytokine storm from unrestrained T cell activation [62]. As suggested by data from humanized mice and rats using the same superagonist [63,64], this most likely represented only a transient induction of Tregs.
Unlike autoimmunity, patients with malignancies (such as breast, ovarian, pancreatic, skin, liver and lung cancers) or viral infections (such as HIV, hepatitis B, hepatitis C and CMV) have increased Treg numbers and function [65–69]. Presumably, the depletion of Tregs in these patients increases the anti-cancer or antiviral responses. However, the FOXP3+ T cells that infiltrate tumors or are formed during viral infections may well represent an anti-tumor or antiviral response. Supporting this notion is the observation that acute viral infections (that get cleared) are also accompanied by the increased generation of FOXP3+ “Tregs” [70,71]. In multiple reports, tissue-infiltrating FOXP3+ T cells are thought of as a unique and stable population of immune regulatory cells that are distinct from the responding effector cells. In fact, chronic antigenic exposure or modified antigen presentation during viral infection or cancer may result in the skewing of an effector T cell response toward a sustained Treg phenotype. This concept opens the possibility of dissecting the mechanisms that operate in such sustenance. Thus, rather than depletion of Tregs or stimulation of the immune system, the counter-intuitive approach of blocking repeated stimulation of these T cells may be the correct immune therapeutic strategy. If the operating mechanisms are left intact, mere depletion of Tregs may lead to two untoward effects: (1) This approach may deplete the very cells that are tumor- or virus-specific and (2) The effector cells remaining in the host would still respond in a manner that promoted Treg formation.
In conclusion, current evidence from studies on human Tregs suggests a model that is quite distinct from that in mice, necessitating specific human studies before embarking on therapeutic intervention. It appears that the generation of transient FOXP3+ regulatory T cells is the norm during CD4 and CD8 T cell activation. Only a small subset of such cells probably persist as stable Tregs or dynamically interchange with the effector/memory pool. Moreover, such peripheral generation of Tregs, rather than thymic derivation, is the major source of circulating Tregs in adult human beings. Future studies focused on issues regarding the mechanism of their sustenance versus reversal will provide important insights into the potential targets of therapeutic intervention.
Acknowledgments
Our work is supported by grants (to N.J.K.) from the NIH and National MS Society (NMSS). V.P. is a postdoctoral fellow of the NMSS and N.J.K. is a Harry Weaver Neuroscience Scholar of the NMSS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shevach EM. From vanilla to 28 flavors: multiple varieties of T regulatory cells. Immunity. 2006;25:195–201. doi: 10.1016/j.immuni.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 2.von Boehmer H. Mechanisms of suppression by suppressor T cells. Nat Immunol. 2005;6:338–344. doi: 10.1038/ni1180. [DOI] [PubMed] [Google Scholar]
- 3.Fontenot JD, Rudensky AY. A well adapted regulatory contrivance: regulatory T cell development and the forkhead family transcription factor Foxp3. Nat Immunol. 2005;6:331–337. doi: 10.1038/ni1179. [DOI] [PubMed] [Google Scholar]
- 4.Wu Y, Borde M, Heissmeyer V, Feuerer M, Lapan AD, Stroud JC, et al. FOXP3 controls regulatory T cell function through cooperation with NFAT. Cell. 2006;126:375–387. doi: 10.1016/j.cell.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 5.Lopes JE, Torgerson TR, Schubert LA, Anover SD, Ocheltree EL, Ochs HD, et al. Analysis of FOXP3 reveals multiple domains required for its function as a transcriptional repressor. J Immunol. 2006;177:3133–3142. doi: 10.4049/jimmunol.177.5.3133. [DOI] [PubMed] [Google Scholar]
- 6.Ziegler SF. FOXP3: Of Mice and Men. Annu Rev Immunol. 2006;24:209–226. doi: 10.1146/annurev.immunol.24.021605.090547. [DOI] [PubMed] [Google Scholar]
- 7.Chen W, Jin W, Hardegen N, Lei KJ, Li L, Marinos N, et al. Conversion of peripheral CD4+CD25− naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kretschmer K, Apostolou I, Hawiger D, Khazaie K, Nussenzweig MC, von Boehmer H. Inducing and expanding regulatory T cell populations by foreign antigen. Nat Immunol. 2005;6:1219–1227. doi: 10.1038/ni1265. [DOI] [PubMed] [Google Scholar]
- 9.Picca CC, Caton AJ. The role of self-peptides in the development of CD4+ CD25+ regulatory T cells. Curr Opin Immunol. 2005;17:131–136. doi: 10.1016/j.coi.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Taams LS, Palmer DB, Akbar AN, Robinson DS, Brown Z, Hawrylowicz CM. Regulatory T cells in human disease and their potential for therapeutic manipulation. Immunology. 2006;118:1–9. doi: 10.1111/j.1365-2567.2006.02348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vitetta ES, Ghetie VF. Immunology. Considering therapeutic antibodies. Science. 2006;313:308–309. doi: 10.1126/science.1130482. [DOI] [PubMed] [Google Scholar]
- 12.Beyer M, Schultze JL. Regulatory T cells in cancer. Blood. 2006;108:804–811. doi: 10.1182/blood-2006-02-002774. [DOI] [PubMed] [Google Scholar]
- 13.Dejaco C, Duftner C, Grubeck-Loebenstein B, Schirmer M. Imbalance of regulatory T cells in human autoimmune diseases. Immunology. 2006;117:289–300. doi: 10.1111/j.1365-2567.2005.02317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Umetsu DT, DeKruyff RH. The regulation of allergy and asthma. Immunol Rev. 2006;212:238–255. doi: 10.1111/j.0105-2896.2006.00413.x. [DOI] [PubMed] [Google Scholar]
- 15.Suvas S, Rouse BT. Treg control of antimicrobial T cell responses. Curr Opin Immunol. 2006;18:344–348. doi: 10.1016/j.coi.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Rouse BT, Sarangi PP, Suvas S. Regulatory T cells in virus infections. Immunol Rev. 2006;212:272–286. doi: 10.1111/j.0105-2896.2006.00412.x. [DOI] [PubMed] [Google Scholar]
- 17.Walker MR, Carson BD, Nepom GT, Ziegler SF, Buckner JH. De novo generation of antigen-specific CD4+CD25+ regulatory T cells from human CD4+CD25− cells. Proc Natl Acad Sci U S A. 2005;102:4103–4108. doi: 10.1073/pnas.0407691102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker MR, Kasprowicz DJ, Gersuk VH, Benard A, Van Landeghen M, Buckner JH, et al. Induction of FoxP3 and acquisition of T regulatory activity by stimulated human CD4+CD25− T cells. J Clin Invest. 2003;112:1437–1443. doi: 10.1172/JCI19441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fehervari Z, Sakaguchi S. CD4+ Tregs and immune control. J Clin Invest. 2004;114:1209–1217. doi: 10.1172/JCI23395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shevach EM. Regulatory/suppressor T cells in health and disease. Arthritis Rheum. 2004;50:2721–2724. doi: 10.1002/art.20500. [DOI] [PubMed] [Google Scholar]
- 21.Liu W, Putnam AL, Xu-Yu Z, Szot GL, Lee MR, Zhu S, et al. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med. 2006 doi: 10.1084/jem.20060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roncador G, Brown PJ, Maestre L, Hue S, Martinez-Torrecuadrada JL, Ling KL, et al. Analysis of FOXP3 protein expression in human CD4+CD25+ regulatory T cells at the single-cell level. Eur J Immunol. 2005;35:1681–1691. doi: 10.1002/eji.200526189. [DOI] [PubMed] [Google Scholar]
- 23.Pillai V, Ortega SB, Wang CK, Karandikar NJ. Transient regulatory T-cells: a state attained by all activated human T-cells. Clin Immunol. 2007;123:18–29. doi: 10.1016/j.clim.2006.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE. Transient expression of FOXP3 in human activated nonregulatory CD4(+) T cells. Eur J Immunol. 2007;37:129–138. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- 25.Allan SE, Crome SQ, Crellin NK, Passerini L, Steiner TS, Bacchetta R, et al. Activation-induced FOXP3 in human T effector cells does not suppress proliferation or cytokine production. Int Immunol. 2007;19:345–354. doi: 10.1093/intimm/dxm014. [DOI] [PubMed] [Google Scholar]
- 26.Selvaraj RK, Geiger TL. A kinetic and dynamic analysis of Foxp3 induced in T cells by TGF-beta. J Immunol. 2007;178:7667–7677. doi: 10.4049/jimmunol.178.12.7667. [DOI] [PubMed] [Google Scholar]
- 27.Tran DQ, Ramsey H, Shevach EM. Induction of FOXP3 expression in naive human CD4+FOXP3− T cells by T cell receptor stimulation is TGFβ-dependent but does not confer a regulatory phenotype. Blood. 2007 doi: 10.1182/blood-2007-06-094656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gavin MA, Torgerson TR, Houston E, Deroos P, Ho WY, Stray-Pedersen A, et al. Single-cell analysis of normal and FOXP3-mutant human T cells: FOXP3 expression without regulatory T cell development. Proc Natl Acad Sci U S A. 2006;103:6659–6664. doi: 10.1073/pnas.0509484103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahic M, Yaqub S, Johansson CC, Tasken K, Aandahl EM. FOXP3+CD4+CD25+ adaptive regulatory T cells express cyclooxygenase-2 and suppress effector T cells by a prostaglandin E2-dependent mechanism. J Immunol. 2006;177:246–254. doi: 10.4049/jimmunol.177.1.246. [DOI] [PubMed] [Google Scholar]
- 30.Bisikirska B, Colgan J, Luban J, Bluestone JA, Herold KC. TCR stimulation with modified anti-CD3 mAb expands CD8+ T cell population and induces CD8+CD25+ Tregs. J Clin Invest. 2005;115:2904–2913. doi: 10.1172/JCI23961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 32.Mallone R, Kochik SA, Reijonen H, Carson B, Ziegler SF, Kwok WW, et al. Functional avidity directs T-cell fate in autoreactive CD4+ T cells. Blood. 2005;106:2798–2805. doi: 10.1182/blood-2004-12-4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sakaguchi S. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol. 2005;6:345–352. doi: 10.1038/ni1178. [DOI] [PubMed] [Google Scholar]
- 34.Gershon RK, Eardley DD, Naidorf KF, Ptak W. The hermaphrocyte: a suppressor-helper T cell. Cold Spring Harbor symposia on quantitative biology. 1977;41(Pt 1):85–91. doi: 10.1101/sqb.1977.041.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Xu L, Kitani A, Fuss I, Strober W. Cutting edge: regulatory T cells induce CD4+CD25−Foxp3− T cells or are self-induced to become Th17 cells in the absence of exogenous TGF-beta. J Immunol. 2007;178:6725–6729. doi: 10.4049/jimmunol.178.11.6725. [DOI] [PubMed] [Google Scholar]
- 36.Korn T, Reddy J, Gao W, Bettelli E, Awasthi A, Petersen TR, et al. Myelin-specific regulatory T cells accumulate in the CNS but fail to control autoimmune inflammation. Nat Med. 2007;13:423–431. doi: 10.1038/nm1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vukmanovic-Stejic M, Zhang Y, Cook JE, Fletcher JM, McQuaid A, Masters JE, et al. Human CD4+ CD25hi Foxp3+ regulatory T cells are derived by rapid turnover of memory populations in vivo. J Clin Invest. 2006;116:2423–2433. doi: 10.1172/JCI28941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akbar AN, Vukmanovic-Stejic M, Taams LS, Macallan DC. The dynamic co-evolution of memory and regulatory CD4+ T cells in the periphery. Nat Rev Immunol. 2007;7:231–237. doi: 10.1038/nri2037. [DOI] [PubMed] [Google Scholar]
- 39.Karandikar NJ, Crawford MP, Yan X, Ratts RB, Brenchley JM, Ambrozak DR, et al. Glatiramer acetate (Copaxone) therapy induces CD8 T cell responses in patients with multiple sclerosis. J Clin Invest. 2002;109:641–649. doi: 10.1172/JCI14380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hong J, Li N, Zhang X, Zheng B, Zhang JZ. Induction of CD4+CD25+ regulatory T cells by copolymer-I through activation of transcription factor Foxp3. Proc Natl Acad Sci U S A. 2005;102:6449–6454. doi: 10.1073/pnas.0502187102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Till SJ, Francis JN, Nouri-Aria K, Durham SR. Mechanisms of immunotherapy. J Allergy Clin Immunol. 2004;113:1025–1034. doi: 10.1016/j.jaci.2004.03.024. quiz 1035. [DOI] [PubMed] [Google Scholar]
- 42.Macdonald KP, Kuns RD, Rowe V, Morris ES, Banovic T, Bofinger H, et al. Effector and regulatory T-cell function is differentially regulated by RelB within antigen-presenting cells during GVHD. Blood. 2007;109:5049–5057. doi: 10.1182/blood-2007-01-067249. [DOI] [PubMed] [Google Scholar]
- 43.Morgan ME, van Bilsen JH, Bakker AM, Heemskerk B, Schilham MW, Hartgers FC, et al. Expression of FOXP3 mRNA is not confined to CD4+CD25+ T regulatory cells in humans. Hum Immunol. 2005;66:13–20. doi: 10.1016/j.humimm.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 44.Manavalan JS, Kim-Schulze S, Scotto L, Naiyer AJ, Vlad G, Colombo PC, et al. Alloantigen specific CD8+CD28− FOXP3+ T suppressor cells induce ILT3+ ILT4+ tolerogenic endothelial cells, inhibiting alloreactivity. Int Immunol. 2004;16:1055–1068. doi: 10.1093/intimm/dxh107. [DOI] [PubMed] [Google Scholar]
- 45.Tennakoon DK, Mehta RS, Ortega SB, Bhoj V, Racke MK, Karandikar NJ. Therapeutic induction of regulatory, cytotoxic CD8+ T cells in multiple sclerosis. J Immunol. 2006;176:7119–7129. doi: 10.4049/jimmunol.176.11.7119. [DOI] [PubMed] [Google Scholar]
- 46.Kim-Schulze S, Scotto L, Vlad G, Piazza F, Lin H, Liu Z, et al. Recombinant Ig-like transcript 3-Fc modulates T cell responses via induction of Th anergy and differentiation of CD8+ T suppressor cells. J Immunol. 2006;176:2790–2798. doi: 10.4049/jimmunol.176.5.2790. [DOI] [PubMed] [Google Scholar]
- 47.Chang CC, Ciubotariu R, Manavalan JS, Yuan J, Colovai AI, Piazza F, et al. Tolerization of dendritic cells by TS cells: the crucial role of inhibitory receptors ILT3 and ILT4. Nat Immunol. 2002;3:237–243. doi: 10.1038/ni760. [DOI] [PubMed] [Google Scholar]
- 48.Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, Landay A, et al. Expression of interleukin IL-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J Exp Med. 2006 doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cobb BS, Hertweck A, Smith J, O’Connor E, Graf D, Cook T, et al. A role for Dicer in immune regulation. J Exp Med. 2006;203:2519–2527. doi: 10.1084/jem.20061692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen C, Rowell EA, Thomas RM, Hancock WW, Wells AD. Transcriptional regulation by foxp3 is associated with direct promoter occupancy and modulation of histone acetylation. J Biol Chem. 2006;281:36828–36834. doi: 10.1074/jbc.M608848200. [DOI] [PubMed] [Google Scholar]
- 51.Marson A, Kretschmer K, Frampton GM, Jacobsen ES, Polansky JK, MacIsaac KD, et al. Foxp3 occupancy and regulation of key target genes during T-cell stimulation. Nature. 2007;445:931–935. doi: 10.1038/nature05478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zheng Y, Josefowicz SZ, Kas A, Chu TT, Gavin MA, Rudensky AY. Genome-wide analysis of Foxp3 target genes in developing and mature regulatory T cells. Nature. 2007;445:936–940. doi: 10.1038/nature05563. [DOI] [PubMed] [Google Scholar]
- 53.Viglietta V, Baecher-Allan C, Weiner HL, Hafler DA. Loss of functional suppression by CD4+CD25+ regulatory T cells in patients with multiple sclerosis. J Exp Med. 2004;199:971–979. doi: 10.1084/jem.20031579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haas J, Hug A, Viehover A, Fritzsching B, Falk CS, Filser A, et al. Reduced suppressive effect of CD4+CD25high regulatory T cells on the T cell immune response against myelin oligodendrocyte glycoprotein in patients with multiple sclerosis. Eur J Immunol. 2005;35:3343–3352. doi: 10.1002/eji.200526065. [DOI] [PubMed] [Google Scholar]
- 55.Balandina A, Lecart S, Dartevelle P, Saoudi A, Berrih-Aknin S. Functional defect of regulatory CD4+CD25+ T cells in the thymus of patients with autoimmune myasthenia gravis. Blood. 2005;105:735–741. doi: 10.1182/blood-2003-11-3900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sugiyama H, Gyulai R, Toichi E, Garaczi E, Shimada S, Stevens SR, et al. Dysfunctional blood and target tissue CD4+CD25high regulatory T cells in psoriasis: mechanism underlying unrestrained pathogenic effector T cell proliferation. J Immunol. 2005;174:164–173. doi: 10.4049/jimmunol.174.1.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kriegel MA, Lohmann T, Gabler C, Blank N, Kalden JR, Lorenz HM. Defective suppressor function of human CD4+ CD25+ regulatory T cells in autoimmune polyglandular syndrome type II. J Exp Med. 2004;199:1285–1291. doi: 10.1084/jem.20032158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yamazaki S, Inaba K, Tarbell KV, Steinman RM. Dendritic cells expand antigen-specific Foxp3+ CD25+ CD4+ regulatory T cells including suppressors of alloreactivity. Immunol Rev. 2006;212:314–329. doi: 10.1111/j.0105-2896.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 59.Beyersdorf N, Hanke T, Kerkau T, Hunig T. CD28 superagonists put a break on autoimmunity by preferentially activating CD4+CD25+ regulatory T cells. Autoimmun Rev. 2006;5:40–45. doi: 10.1016/j.autrev.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 60.Hoffmann P, Eder R, Kunz-Schughart LA, Andreesen R, Edinger M. Large-scale in vitro expansion of polyclonal human CD4+CD25high regulatory T cells. Blood. 2004;104:895–903. doi: 10.1182/blood-2004-01-0086. [DOI] [PubMed] [Google Scholar]
- 61.Can super-antibody drugs be tamed? Nature. 2006;440:855–856. doi: 10.1038/440855a. [DOI] [PubMed] [Google Scholar]
- 62.Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, et al. Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 2006;355:1018–1028. doi: 10.1056/NEJMoa063842. [DOI] [PubMed] [Google Scholar]
- 63.Beyersdorf N, Balbach K, Hunig T, Kerkau T. Large-scale expansion of rat CD4 CD25 T cells in the absence of T-cell receptor stimulation. Immunology. 2006 doi: 10.1111/j.1365-2567.2006.02455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Legrand N, Cupedo T, van Lent AU, Ebeli MJ, Weijer K, Hanke T, et al. Transient accumulation of human mature thymocytes and regulatory T cells with CD28 superagonist in “human immune system” Rag2−/−γc−/− mice. Blood. 2006;108:238–245. doi: 10.1182/blood-2006-01-0190. [DOI] [PubMed] [Google Scholar]
- 65.Aandahl EM, Michaelsson J, Moretto WJ, Hecht FM, Nixon DF. Human CD4+ CD25+ regulatory T cells control T-cell responses to human immunodeficiency virus and cytomegalovirus antigens. J Virol. 2004;78:2454–2459. doi: 10.1128/JVI.78.5.2454-2459.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cabrera R, Tu Z, Xu Y, Firpi RJ, Rosen HR, Liu C, et al. An immunomodulatory role for CD4+CD25+ regulatory T lymphocytes in hepatitis C virus infection. Hepatology. 2004;40:1062–1071. doi: 10.1002/hep.20454. [DOI] [PubMed] [Google Scholar]
- 67.Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–949. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 68.Liyanage UK, Moore TT, Joo HG, Tanaka Y, Herrmann V, Doherty G, et al. Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol. 2002;169:2756–2761. doi: 10.4049/jimmunol.169.5.2756. [DOI] [PubMed] [Google Scholar]
- 69.Woo EY, Yeh H, Chu CS, Schlienger K, Carroll RG, Riley JL, et al. Cutting edge: Regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. J Immunol. 2002;168:4272–4276. doi: 10.4049/jimmunol.168.9.4272. [DOI] [PubMed] [Google Scholar]
- 70.Luhn K, Simmons CP, Moran E, Dung NT, Chau TN, Quyen NT, et al. Increased frequencies of CD4+ CD25high regulatory T cells in acute dengue infection. J Exp Med. 2007;204:979–985. doi: 10.1084/jem.20061381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Walther M, Tongren JE, Andrews L, Korbel D, King E, Fletcher H, et al. Upregulation of TGF-beta, FOXP3, and CD4+CD25+ regulatory T cells correlates with more rapid parasite growth in human malaria infection. Immunity. 2005;23:287–296. doi: 10.1016/j.immuni.2005.08.006. [DOI] [PubMed] [Google Scholar]