ABSTRACT
The increasing incidence of central nervous system (CNS) lymphoma in the general population, especially in young adults with AIDS, should alert the otolaryngologist that in future there will be an even greater incidence of this rare disease. It may be responsible for hearing loss accompanied by other neurological deficits. CNS lymphoma often has a rapidly progressive course. Early diagnosis and rapid therapy are crucial for a better prognosis. We report a case of primary CNS lymphoma involving both internal auditory canals that presented with sudden deafness and disequilibrium accompanied by facial and abducens nerve palsy.
Keywords: Lymphoma, hearing loss, internal auditory canal
Malignant non-Hodgkin's primary central nervous system lymphoma (PCNSL) accounts for 3% of all intracranial tumors.1,2 Risk factors associated with PCNSL include AIDS, immunosuppression for organ transplantation, autoimmune diseases, and congenital immunodeficiencies. Over the past decade the incidence of the PCNSL increased in both immunosuppressed and immunocompetent patients, and developed in up to 6% of patients with AIDS.3
CASE REPORT
A 68-year-old female was referred to our department with bilateral sudden deafness that was associated with tinnitus, disequilibrium, left-sided facial palsy, occipital headache, and diplopia.
Two years previously she had been treated for colon carcinoma by resection followed by adjuvant chemotherapy. There was no evidence of tumor recurrence or metastasis as determined by abdominal computed tomography (CT) scan and chest x-ray.
On examination, she was apyrexial and had no signs suggestive of meningitis. Audiometry confirmed bilateral deafness, and caloric tests demonstrated bilateral loss of vestibular function. Her diplopia was caused by a right sixth nerve palsy. On funduscopy it was evident that she had bilateral edema with hemorrhages around the optic discs.
Routine blood picture and chemistry was normal as was her erythrocyte sedimentation rate (ESR). Serological tests for HIV, toxoplasmosis, borreliosis, and syphilis were negative.
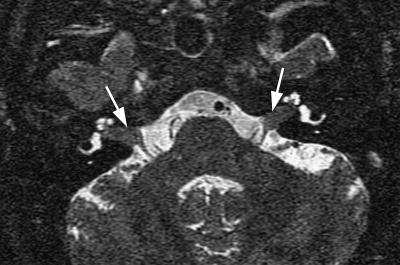
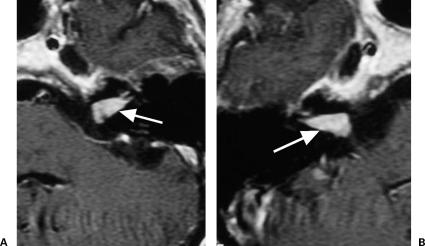
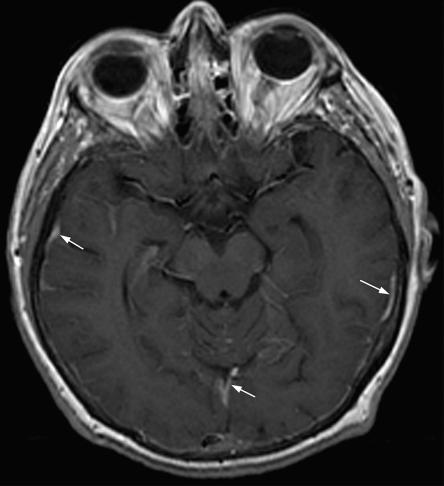
Magnetic resonance imaging (MRI) of the brain revealed symmetrical tumors in both internal auditory canals on T2-weighted images (Fig. 1). These tumors enhanced intensely with gadolinium on T1-weighted images (Fig. 2). There was also generalized enhancement of the supratentorial and infratentorial meninges (Fig. 3).
Figure 1.
Axial T2-weighted magnetic resonance imaging (MRI) revealed tumor formations in both internal auditory canals (arrows).
Figure 2.
Axial T1-weighted magnetic resonance imaging (MRI) with gadolinium. (A) The contrast-enhanced tumor is shown in the left internal auditory canal (arrow). (B) The contrast-enhanced tumor is shown in the right internal auditory canal (arrow).
Figure 3.
Axial T1-weighted magnetic resonance imaging (MRI) with gadolinium revealed generalized enhancement of the meninges (arrows).
At first it was thought that she had meningeal metastases in view of her previous history of colon carcinoma, her age, and clinical and radiological findings. Cytological examination of the cerebrospinal fluid (CSF) obtained by lumbar puncture revealed a central nervous system (CNS) lymphoma. Therapy was started with intrathecal high-dose methotrexate (MTX) in combination with systemic prednisolone (five cycles). This resulted in a reduction of malignant cells in subsequent lumbar punctures but failed to improve either her clinical signs or symptoms. At this stage, the patient refused any further therapy or intervention.
DISCUSSION
Acute onset or rapidly progressive bilateral sensory-neural hearing loss is usually caused by inflammatory processes like meningitis and bacterial and viral neuritis. Less frequently, neoplastic diseases can also be responsible for bilateral sudden deafness.
Diffuse large cell lymphoma of B-cell origin is the most common subtype of PCNSL that primarily involves the CNS. This malignancy can mimic several neurological diseases. The clinical picture is sometimes similar to cerebrovascular disease or encephalitis with multiple cranial nerve palsies. Symptoms usually include focal neurological deficits (73%), neuropsychiatric symptoms (28%), seizures (9%), and increased intracranial pressure (3%). The most common sites of involvement are the frontal lobe, temporoparietal lobe, and basal ganglia. Multiple intracranial lesions can be present in 25 to 44% of the patients.4 Bilateral involvement of the internal auditory canal in PCNSL is very rare. A review of the literature revealed three reports of PCNSL presenting with bilateral symmetric cerebellopontine angle tumors.5,6,7
The imaging method of choice is MRI with gadolinium, which usually shows either space-occupying lesions or diffusely infiltrating masses with intense contrast enhancement in T1-weighted images. In cases with diffuse leptomeningeal involvement, generalized postcontrast enhancement of the meninges would be present. The definitive diagnosis can be made with the help of a surgical biopsy. In cases of leptomeningeal or ventricle involvement, CSF cytology with selective immunostains can be quite reliable.8
To confirm the diagnosis of PCNSL, systemic lymphoma must be ruled out. Fewer than 5% of patients with CNS lymphoma have systemic disease at presentation.1,2
The median survival rate without therapy is ~14 months.2,3 The main therapy for PCNSL is focused on high-dose intrathecal chemotherapy with MTX accompanied by systemic steroids, using radiation as a deferred alternative. The role of surgery is to obtain adequate biopsy samples for diagnosis (if it is not obtainable with CSF cytology). However, in solitary lesions, extensive surgical removal may improve survival.1
CONCLUSION
The increasing incidence of PCNSL in the general population, and especially in young adults with AIDS, should alert neuro-otologists and neurosurgeons about the increasing incidence of such rare tumors in the internal auditory canal and cerebellopontine angle (CPA). Not every young patient with bilateral tumors in the internal auditory canal has neurofibromatosis type 2. Due to the critical and rapidly progressive course of the disease, rapid establishment of the diagnosis and immediate induction of chemotherapy are vitally important.
REFERENCES
- Angeli S I, Brackmann D E, Xenellis J E, et al. Primary lymphoma of the internal auditory canal: case report and review of the literature. Ann Otol Rhinol Laryngol. 1998;107:17–21. doi: 10.1177/000348949810700104. [DOI] [PubMed] [Google Scholar]
- Gumerlock M K, Neuwelt E A. In: Dana BW, editor. Malignant Lymphomas, Including Hodgkin's Disease: Diagnosis, Management, and Special Problems. Boston: Kulwer Academic Publishers; 1993. Primary cerebral lymphoma. pp. 111–126.
- Hochberg F H, Miller D C. Primary central nervous system lymphoma. J Neurosurg. 1988;68:835–853. doi: 10.3171/jns.1988.68.6.0835. [DOI] [PubMed] [Google Scholar]
- Tomlinson F H, Kurtin P J, Suman V J, et al. Primary intracerebral malignant lymphoma: a clinicopathological study of 89 patients. J Neurosurg. 1995;82:558–566. doi: 10.3171/jns.1995.82.4.0558. [DOI] [PubMed] [Google Scholar]
- Jaiswal A K, Mahapatra A K, Sharma M C. Primary central nervous lymphoma presenting as bilateral cerebellopontine angle lesions: a rare case report. J Clin Neurosci. 2004;11:328–331. doi: 10.1016/S0967-5868(03)00110-3. [DOI] [PubMed] [Google Scholar]
- Garth R J, Coddington R, Brightwell A P. Primary cerebral lymphoma presenting with bilateral cerebellopontine angle lesions. J Laryngol Otol. 1993;107:937–939. doi: 10.1017/s0022215100124843. [DOI] [PubMed] [Google Scholar]
- Larner A J, D'Arrigo C, Scaravilli F, et al. Bilateral symmetrical enhancing brainstem lesions: an unusual presentation of primary CNS lymphoma. Eur J Neurol. 1999;6:721–723. doi: 10.1046/j.1468-1331.1999.660721.x. [DOI] [PubMed] [Google Scholar]
- Schmitt-Graff A, Pfitzer P. Cytology of cerebrospinal fluid in primary malignant lymphomas of the central nervous system. Acta Cytol. 1983;27:267–272. [PubMed] [Google Scholar]