Abstract
Urachal tumours are rare vesical neoplasms. We report a case of urachal adenocarcinoma in a 31-year-old patient.
Keywords: Urachal, Tumour, Vesical, Adenocarcinoma
Urachal tumours are rare vesical neoplasms that represent 0.01% of all cancers. They are histologically classified as either: (i) adenocarcinoma – squamous cell carcinomas which commonly occur in the 5th to 7th decade; and (ii) sarcomas which usually present in younger patients before the age of 40 years. We report a case of urachal adenocarcinoma in a 31-year-old patient.
Case report
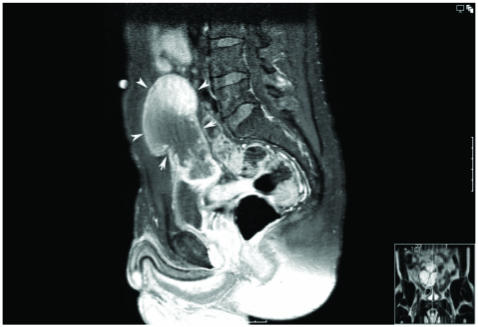
A 31-year-old male was referred on a non-urgent basis from the community with frank haematuria and vague suprapubic pain. Clinical examination revealed an ill-defined midline infra-umbilical mass which was not consistent with an obstructed bladder. A subsequent flexible cystoscopy demonstrated an extrinsic compression defect at the bladder dome, but no mucosal lesion. MRI demonstrated a contrast enhancing lobulated mass extending from the bladder dome to the umbilicus, suspicious for malignancy (Fig. 1). Further staging with CT and bone scan was negative for distal disease.
Figure 1.
MRI contrast-enhanced lobulated mass arising from a vesicourachal diverticulum off the midline bladder dome and extending to the umbilicus (outlined by white arrows).
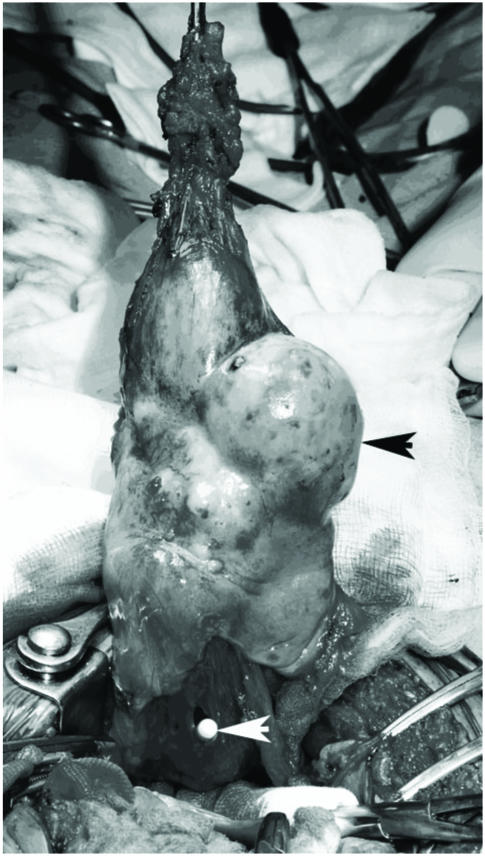
The patient underwent partial cystectomy umbilectomy and excision of urachal tumour (Fig. 2). After ensuring complete excision of the tumour, a small defect of the recti muscles was reinforced with a polypropylene mesh. The patient made an uneventful recovery and was discharged 4 days later. A multidisciplinary meeting decided no further adjuvant treatment was necessary. Histology confirmed a moderately differentiated mutinous adenocarcinoma.
Figure 2.
Multilobulated cyst (black arrow) containing mutinous material with umbilicus and dome of bladder (tip of urethral catheter visible-white arrow).
Discussion
The pathogenesis of urachal tumours is not fully understood. It is believed that urachal carcinomas arise from malignant transformation of columnar or glandular metaplastic epithelium. They lie in the space of Retzius, between transversalis fascia anteriorly and peritoneum posteriorly, extending from the dome of the bladder to the umbilicus. The presence of urachal remnants predispose to its formation and prophylactic excision of benign urachal lesions has been recommended.1
Its response to radiotherapy and chemotherapy is modest and the only therapeutic approach is surgical eradication.2 Resection margins and tumour grade are the most important prognostic factors. This neoplastic embryological remnant has a poor prognosis and is uniformly fatal. This is due to: (i) late presentation of symptoms leading to advanced stage at diagnosis; (ii) a propensity for early local invasion; and (iii) distal metastasis. A systematic review of the literature reveals a 5-year survival rate of less than 20%, although a recent large case series reported 40% of patients with localised and distal disease survived at 5 years.3
Conclusions
Although this tumour has now become a recognisable ‘neoplastic entity’, its origin and pathophysiology remain unknown. Modern therapeutic regimens have offered minimal benefit, especially when unresectable. The question as to whether partial or radical cystectomy is suitable for localised disease is difficult to answer since urachal tumours are rare. Furthermore, within this group, urachal adenocarcinoma is uncommon in those under 40 years. However, in order to evaluate which surgical approach is correct or whether new chemotherapeutic agents will induce objective responses and improve long-term survival requires co-operation between physicians and centres internationally so that larger studies can be conducted. This approach can only benefit patients.
References
- 1.Upadhyay V, Kukkady A. Urachal remnants: an enigma. Eur J Pediatr Surg. 2003;13:372–6. doi: 10.1055/s-2003-44725. [DOI] [PubMed] [Google Scholar]
- 2.Siefker-Radtke AO, Gee J, Shen Y, Wen S, Daliani D, Millikan RE, et al. Multimodality management of urachal carcinoma: the M.D. Anderson Cancer Center experience. J Urol. 2003;169:1295–8. doi: 10.1097/01.ju.0000054646.49381.01. [DOI] [PubMed] [Google Scholar]
- 3.Ashley RA, Inman BA, Sebo TJ, Leibovich BC, Blute ML, Kwon ED, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer. 2006;107:712–20. doi: 10.1002/cncr.22060. [DOI] [PubMed] [Google Scholar]