Abstract
Background:
Cardiovascular risk factors are common in individuals with chronic spinal cord injury (SCI), and their prevalence increases with age. The actual prevalence of overt cardiovascular disease (CVD) in this population has not been well established.
Methods:
Electrocardiograms (ECGs) were examined for abnormalities in 43 individuals with abnormal lipid profiles being followed in the outpatient SCI clinic of our institution. The mean age of the study population of predominantly men was 43 ± 9.9 years and the mean duration of injury 16.6 ± 8 years.
Results:
ECG abnormalities were common and present in 60.5% of participants. ST-T wave abnormalities were the most commonly observed (35%). Evidence of previous myocardial infarction was present in 7% of all individuals and in 12% of those with ECG abnormalities. The only clinical parameter differentiating the group with normal vs abnormal ECG was the duration of injury (19.5 ± 8 y vs 12 ± 5 y; P = 0.0026). Analysis of variance showed that injury duration was the sole predictor of abnormal ECG with 68% accuracy (P = 0.006). Among those with ECG abnormalities, although no significant differences were detected between those with and without evidence of previous myocardial infarction, mean total cholesterol and low-density lipoprotein were higher, and mean high-density lipoprotein was lower. Mean age and injury duration were greater in those with evidence of previous myocardial infarction.
Conclusion:
Although age is an important risk factor for CVD in the population of individuals without disabilities, injury duration is at least as important as age in those with SCI. Our findings support the recommendation that individuals with SCI and abnormal lipids should be screened for CVD regardless of age.
Keywords: Spinal cord injuries, Cardiovascular risk, Lipid profile, Electrocardiogram, Myocardiol infarction
INTRODUCTION
Improvements in health care in the 20th century have significantly improved the life expectancy for individuals living with chronic spinal cord injury (SCI) (1,2). As mortality from infectious causes (eg, urinary tract infection) has decreased, cardiovascular disease (CVD) has emerged as a leading cause of death in individuals with chronic SCI (1,3). Risk factors for CVD are prevalent in these individuals and are believed to be attributable, in part, to involuntary immobilization and abnormal body composition. Documented risk factors seen in persons with SCI include an abnormal lipid profile with particularly low levels of the cardioprotective high-density lipoprotein (HDL) and increased body fat mass with increased insulin resistance and abnormal postprandial glucose metabolism (4,5).
The actual prevalence of coronary artery disease in persons living with SCI and having a significant number of risk factors for CVD has not been well established, although Whiteneck et al reported that the incidence of CVD in the community of individuals with SCI was greater than that observed in the general population (6). They further reported that increased morbidity from CVD was associated with age and/or duration of injury (6). Janssen et al further reported that the risk profile for men with long-standing SCI did not appear to be significantly different than that observed in control subjects without disability (7).
Although abnormal ECGs are routinely found in the period of time surrounding acute SCI (8,9), ECG changes in chronic SCI have not been well studied. Given the increased prevalence of risk factors for CVD in this population, this study was designed to test the potential benefit of screening for electrocardiographic abnormalities in individuals with chronic SCI who have multiple risk factors for CVD, particularly abnormal lipid profiles.
METHODS
Retrospective review of 12-lead ECGs and clinical characteristics were obtained for 43 individuals with risk factors for CVD who presented for routine annual physical examination in the SCI Model System of Care (SCIMSC) Clinics (10) between 1994 and 1999. Criteria for inclusion in the study population were based on the lipid profile. Threshold values for inclusion included total cholesterol (TC) >200 mg/dL, low-density-lipoprotein (LDL) >130 mg/dL, HDL <40 mg/dL or TC to HDL ratio of >5. Individuals with at least 1 abnormal lipid value were included. Individuals who had a history of diabetes mellitus or who were taking hypoglycemic medications were not included in the study. The prevalence of smoking in all participants was approximately 20%.
Electrocardiograms
All electrocardiographic tracings were performed by trained cardiovascular technicians using a General Electric MAC 500 ECG System using standard leads and placements (11–13) and stored in the Marquette MUSE System (14). All studies were performed in the supine position. ECGs were read for accuracy by one of the staff cardiologists. An abnormal ECG was defined as the presence of 1 or more of the following: bundle branch block, conduction delay, signs of right or left ventricular hypertrophy or left atrial enlargement, prolonged QTC interval, or ST-T depression exceeding 0.5 mm and/or pathological Q waves.
Laboratory Data
All laboratory analyses were performed by the same clinical laboratory facility (Quest Diagnostics, Inc., Teterboro, NJ). All lipid profiles were performed after an overnight fast. Serum TC and triglyceride (TG) levels were assayed on an automated blood analyzer (Hitachi model T36, Hitachi Model T36, Hitachi, Twinsburg, Ohio). Serum HDL was determined by spectrophotometry, and LDL was calculated by the equation of Friedewald et al (15). The ratio of TC to HDL cholesterol has been demonstrated to be the best predictor of risk for CVD regardless of TC level (16,17), and was therefore computed for each subject.
Statistical Analysis
Stepwise logistic regression was used to assess differences between those with or without ECG abnormalities, and to assess differences between those with evidence of previous myocardial infarction among those with ECG abnormalities. Differences in lipid values, age, and injury duration were assessed with univariate analyses of variance.
RESULTS
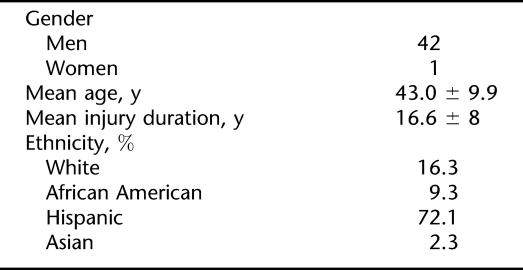
The clinical characteristics of the study population are presented in Table 1. Forty-two participants were men and 1 was a woman. The majority were Hispanic (72%), followed by white (16%), African American (9%), and Asian (2%). Although this distribution of ethnicity (72% Hispanic) is different from the national average (15% Hispanic) (18), it represents the ethnicity of the primary patient population served at this Los Angeles county rehabilitation center. Their mean age was 43 ± 9.9 years and the mean duration of injury was 16.6 ± 8 years. The level and completeness of injury are shown in Table 2. Sixty percent had injury above the T1 level and the remaining 40% had injury at the level below T12. Most had injury classified as neurologically complete (ASIA A) (19). No statistically significant differences in smoking history were noted between the 2 groups.
Table 1.
Clinical Characteristics of the Study Sample
Table 2.
Level and Completeness of SCI, %
Electrocardiographic Findings
Seventeen individuals (39.5%) had normal ECGs. Twenty-six (60.5%) of the participants had abnormal findings, with 1 abnormality present in 20 (46.5%), 2 abnormalities in 4 (9.3%), and 3 abnormalities in 2 persons (4.7%). Table 3 illustrates ECG abnormalities found in the study population. Predominant abnormal findings were ST and T abnormalities, found in 15 (35%), followed by left atrial abnormality in 8 (19%), left ventricular hypertrophy in 6 (14%), and evidence of prior myocardial infarction (MI) with pathological Q waves in 3 (7%). The population was represented in 2 groups: Group 1 with abnormal ECGs and Group 2 with normal ECGs.
Table 3.
Electrocardiographic Abnormalities, %
Laboratory Findings
TC was mildly elevated in both groups. Group 1 (abnormal ECGs) had a mean TC of 204 ± 60 mg/dL, while Group 2 (normal ECG) had a mean TC of 206 ± 39 mg/dL. LDL cholesterol was elevated and similar in both groups (136 ± 36 mg/dL for Group 1 and 136 ± 33 mg/dL for Group 2). HDL cholesterol levels were markedly reduced (27 ± 9 mg/dL in Group 1 and 28 ± 9 mg/dL in Group 2). The ratio of total to HDL cholesterol followed the pattern and was elevated in both groups (8.4 ± 6 in Group 1 and 8 ± 4 in Group 2). No statistically significant differences were noted between groups for any of the values observed.
Age and Duration of Injury
Individuals with abnormal ECGs were slightly older (45 ± 9 y) than those with normal ECGs (41 ± 10 y). This difference between groups did not reach statistical significance. The only clinical parameter to differentiate between groups was the duration of injury. Persons with abnormal ECGs were injured for 19.5 ± 8 years and those with normal ECGs for 12 ± 5 years. The difference was statistically significant at P = 0.0024.
Clinical Correlates of Abnormal ECGs
To assess the influence of clinical parameters on our ECG findings, we performed a stepwise logistic regression analysis. The independent variables included total cholesterol, LDL and HDL cholesterol, ethnicity, level and completeness of neurological deficit (19), age, and duration of injury. Inclusion in either the normal or abnormal ECG group was our dependent variable. Only injury duration was found to be a significant predictor of ECG findings, with 68% accuracy (P = 0.006).
Three subjects (12%) in the abnormal ECG group had evidence of previous MI. Stepwise logistic regression analysis and analyses of variance were also employed to assess differences between those with and without evidence of MI. Although no significant differences were found, the power to detect differences was clearly compromised by the small sample of those with evidence of MI. Among those with evidence of previous myocardial infarction, total cholesterol (219.6 vs 209.3 mg/dL), LDL (153.6 vs 140.6 mg/dL), and total cholesterol to HDL ratio (8.7 vs 7.0) were higher. Mean HDL (25.3 vs 32.7 mg/dL) was lower, and mean age (51.8 vs 44.4 y) and injury duration (23.2 vs 19.0 y) were greater.
DISCUSSION
The main finding of this study is the impact of injury duration on the cardiovascular system. Individuals with SCI who had at least 2 risk factors for CVD (a finding that is common in men with SCI) and longer injury duration had a significantly higher incidence of abnormal ECGs. This was independent of current age. The most common abnormality observed in this population was the presence of T-wave abnormalities, suggesting possible myocardial ischemia. Although these abnormalities are not diagnostic of coronary artery disease, they are only infrequently seen in the absence of cardiovascular impairment. In a study of New York Life Insurance Company subscribers, Singer and Levinson noted that morbidity was highest in the 40- to 49-year-old age group when T-wave abnormalities were present on ECG, given inclusion of all types of ECG abnormalities (20). The risk of adverse outcomes including mortality was twice that of normal subjects in the first 5 years of follow-up (20).
Similarly, Blocker et al found a greater prevalence of ST depression and T-wave abnormalities in 250 veterans living with SCI, while Prakash et al found a similar prevalence of ECG abnormalities in individuals with SCI when compared to those without SCI, and no prognostic implications of ECG abnormalities (21). Our population possessed a high prevalence of risk factors, and was thus at a higher risk for silent CAD than a randomly selected population of individuals with SCI would be. This difference could possibly explain the different results in our study.
Of note, we did not find clinical characteristics that differentiated significantly between individuals who did and did not have evidence of silent myocardial infarction by ECG; those with such evidence appeared worse than those without such evidence on all parameters. The ECG abnormalities cannot be explained by changes in autonomic function since none of the study participants had recent injury. Changes in autonomic function can result in abnormal cardiac rhythms or changes in ventricular depolarization in individuals with high-level SCI, but these changes are typically confined to the period surrounding acute injury (8,9). To avoid potential influence of body position on ECG findings, we included only those tracings performed in the supine position (11–13,22).
Individuals with SCI are now living longer and thus, similar to the population of individuals without disabilities, will have increased incidence of CVD. Additionally, forced immobility and resultant metabolic changes make individuals with chronic SCI at greater risk for the development of risk factors related to the development of CVD (4). Interestingly, those individuals with the longest duration of injury may be at even higher risk for development of CVD. These individuals should therefore be carefully monitored for the presence of silent ischemia, and physicians caring for individuals with chronic SCI should include ECG in their routine screening procedures.
While age is an important determinant of risk for CVD in persons without disability, for individuals with chronic SCI and with risk factors for CVD, injury duration is at least as important. ECG abnormalities are fairly common in persons with chronic SCI, and the presence of lipid abnormalities should alert the clinician to a possibility of underlying CVD. Risk factors should be assessed, monitored, and treated in individuals with SCI and any duration of injury, independent of age. Based on our findings, particular attention should be paid to individuals with longer duration of injury but youthful enough to make them less suspect for CVD.
CONCLUSION
Our study population differs from those described above because they were preselected to have significant risk factors and thus were at higher risk than the general population for CVD. In these individuals, injury leading to prolonged immobilization and the presence of metabolic abnormalities may play an important role in the development of adverse cardiovascular outcomes. Further research is needed to evaluate the effect of risk factor modification in this population.
Acknowledgments
This material is based upon work supported by the National Institute of Disability and Rehabilitation Research, Office of Special Education and Rehabilitative Services, US Department of Education (grant #H133B0310020).
REFERENCES
- DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:1411–1419. doi: 10.1016/s0003-9993(99)90252-6. [DOI] [PubMed] [Google Scholar]
- Kemp BJ, Adkins RH. Foreword. Top Spinal Cord Inj Rehabil. 2001;6:vii. [Google Scholar]
- Phillips WT, Kiratli BJ, Sarkarati M, Weraarchakul BA. Effect of spinal cord injury on the heart and cardiovascular fitness. Curr Probl Cardiol. 1996;23:643–715. doi: 10.1016/s0146-2806(98)80003-0. [DOI] [PubMed] [Google Scholar]
- Bauman W, Spungen A, Raza M, et al. Coronary artery disease: metabolic risk factors and latent disease in individuals with paraplegia. Mt Sinai J Med. 1992;59:163–168. [PubMed] [Google Scholar]
- Bauman WA, Adkins RH, Spungen AM, Kemp BJ, Waters RL. The effect of residual neurologic deficit on serum lipoproteins in individuals with chronic spinal cord injury. Spinal Cord. 1998;36:13–17. doi: 10.1038/sj.sc.3100513. [DOI] [PubMed] [Google Scholar]
- Whiteneck G, Charlifue SW, Frankel HL, et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia. 1992;30:617–630. doi: 10.1038/sc.1992.124. [DOI] [PubMed] [Google Scholar]
- Janssen TW, van Oers CA, van Kamp GJ, TenVoorde BJ, van der Woude LH, Hollander AP. Coronary heart disease, risk indicators, aerobic power and physical activity in men with spinal cord injuries. Arch Phys Med Rehabil. 1997;78:697–705. doi: 10.1016/s0003-9993(97)90076-9. [DOI] [PubMed] [Google Scholar]
- Lehmann KG, Lane JG, Piepmeier JM, Batsford WP. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: incidence, time course and severity. J Am Coll Cardiol. 1987;10:46–52. doi: 10.1016/s0735-1097(87)80158-4. [DOI] [PubMed] [Google Scholar]
- Winslow EB, Lesch M, Talano JV, Meyer PR., Jr Spinal cord injuries associated with cardiopulmonary complications. Spine. 1986;11:809–812. doi: 10.1097/00007632-198610000-00014. [DOI] [PubMed] [Google Scholar]
- US Department of Education. Guide to US Department of Education Programs. Washington, DC: Department of Education; 2006. [Google Scholar]
- American College of Cardiology. Tenth Bethesda Conference of the American College of Cardiology: Optimal Electrocardiography. J Am Coll Cardiol. 1978;41:111–191. [Google Scholar]
- American Heart Association Electrocardiography Committee. AHA Committee Report: recommendations for standardization of leads and of specifications for instruments in electrocardiography and vectorcardiography. Circulation. 1975;52:11–31. doi: 10.1161/01.cir.35.3.583. [DOI] [PubMed] [Google Scholar]
- Bailey JJ, Berson AS, Garson AJ, Horan LG, Macfarlane PW, Mortara DW. Recommendations for standardization and specification in automated electrocardiography: bandwidth and digital signal processing. A Report for Health Professionals by an ad hoc Writing Group of the Committee on Electrocardiography and Cardiac Electrophysiology of the Council on Clinical Cardiology, American Heart Association. Circulation. 1990;81:730–739. doi: 10.1161/01.cir.81.2.730. [DOI] [PubMed] [Google Scholar]
- General Electric Healthcare. ECGenius: MUSE Cardiology Information System. http://www.gehealthcare.com/usen/cardiology/diagnostic_ecg/docs/ECGenius.pdf#search=%22Marquette%20Muse%20System%22. Accessed October 8, 2006.
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- Kannel WB, Wilson PWF. Efficacy of lipid profiles in prediction of coronary disease. Am Heart J. 1992;124:768–774. doi: 10.1016/0002-8703(92)90288-7. [DOI] [PubMed] [Google Scholar]
- Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH. A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med. 1994;325:373–381. doi: 10.1056/NEJM199108083250601. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Population Distribution by Race/Ethnicity. StateHealthFacts.org. http://www.statehealthfacts.org/comparebar.jsp?ind=68cat=1. Accessed March 5, 2007.
- American Spinal Injury Association. International Standards for Neurological Classification of Spinal Injury Patients. J Spinal Cord Med. 2003;26(Suppl 1):550–556. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- Singer RB, Levinson L. Medical Risks: Patterns of Mortality and Survival. Lanham, MD: Lexington Books; 1976. [Google Scholar]
- Blocker WP, Merrill JM, Krebs MA, Cardus DP, Ostermann HJ. An electrocardiogaphic survey of patients with chronic spinal cord injury. Am Correct Ther J. 1983;37:101–104. [PubMed] [Google Scholar]
- Shapiro W, Berson AS, Pipberger HV. Differences between supine and sitting Frank-lead electrocardiograms. J Electrocardiol. 1976;9:303–308. doi: 10.1016/s0022-0736(76)80021-0. [DOI] [PubMed] [Google Scholar]