Abstract
While anterior cruciate ligament (ACL) reconstruction is readily offered to athletes, non-athletes are often treated conservatively. We carried out a retrospective, cross-sectional analysis study to compare the incidence of meniscal and cartilage injuries in an athlete and non-athlete population in relation to time of presentation since injury. The results were used to assess the need and relevance of ACL reconstruction in the non-athlete population. The study included 1375 patients who underwent ACL reconstruction between 1998 and 2004. These patients were initially broadly divided into two categories: athletes (575) and non-athletes (800). Each category was then sub-divided into four subgroups based on time elapsed between the injury and presentation at our clinic (Group A, 3 months; Group B, 3–12 months; Group C, 1–3 years; Group D, more than 3 years). Arthroscopic findings were documented for medial and lateral meniscus and cartilage injuries, and comparisons were made between the incidence of associated injuries in the corresponding groups. There was a statistically significant increase in the incidence of meniscal injuries and cartilage injuries after 1 year in both the groups. There was no difference in the incidence of meniscal and cartilage injuries in athletes and non-athletes among the corresponding groups. (chi-square test, p = 0.05). These results demonstrate that both athletes and non-athletes are equally susceptible for long-term meniscal and cartilage injuries if ACL reconstruction is not carried out early.
Résumé
Tandis que la reconstruction du ligament croisé antérieur est rapidement proposée aux athlètes, les non athlètes sont souvent traités conservativement. Notre étude compare l’incidence des lésions méniscales et cartilagineuses dans les 2 types de population en fonction du temps écoulé depuis le traumatisme pour apprécier la pertinence de la reconstruction du croisé chez les non-athlètes. L’étude incluait 1375 patients ayant eu une reconstruction du croisé antérieur entre 1998 et 2004. Ils étaient divisés en athlètes (575) et non-athlètes (800). Chaque catégorie était divisée en 4 groupes selon le délai depuis le traumatisme : groupe A < 3 mois, groupe B 3 mois à 1 an, groupe C 1 à 3 ans et groupe D > 3 ans. Les données arthroscopiques notaient l’incidence des lésions cartilagineuses et méniscales dans les différents groupes. Il y avait une augmentation significative des atteintes méniscales et cartilagineuses au-delà d’un an dans les 2 populations. Il n’y avait pas de différence statistique dans l’incidence de ces lésions au sein de chaque groupe chez les athlètes et les non-athlètes (chi-square test, p = 0,05). Ceci montre que les non athlètes développent également des lésions cartilagineuses et méniscales si la reconstruction du ligament croisé antérieur n’est pas faite rapidement.
Introduction
Anterior cruciate ligament (ACL) injuries are one of the most common type of surgically managed sports injury. While there is no doubt about the need for ACL reconstruction in athletes, there are wide differences of opinion on managing ACL injuries in the non-athlete population [2, 7]. Many non-athlete ACL injuries are either missed initially or managed conservatively due to the treating physician presuming that non-athletes do not have a significant degree of instability. However, contrary to this supposition, we have observed in our clinic a high incidence of symptomatic instability and meniscal and cartilage injuries in non-athletes.
ACL deficiency leads to long-term complications, including meniscal tears and articular cartilage damage [5, 9]. Randomised control studies aimed at observing the natural history of ACL insufficient knees are not ethically feasible, as the non-operative group will be denied the obvious advantage of ACL reconstruction. Hence, our decision was to assess the long-term incidence of meniscal and cartilage injuries in ACL insufficient knee in patients presenting at various points of time following the injury.
The aim of the study was to determine whether the incidence of long-term complications of ACL insufficiency, such as meniscal and cartilage injuries, in non-athletes is similar to that of athletes. To this end, we compared the incidence of meniscal and cartilage injuries in athlete and non-athlete populations as a variable of the time between the injury and presentation in our clinic. As such, we were able to assess the need and relevance of ACL reconstruction in the non-athlete population.
Materials and methods
This was a retrospective, cross-sectional analysis which included 1375 patients (1130 males and 245 females) who underwent ACL reconstruction in our clinic between 1998 to 2004. These patients were broadly separated into an ‘athlete’ group (n = 575) and a ‘non-athlete’ group (n = 800). The athlete group included sports persons involved in competitive games as well as people who played recreational sports on a regular basis. The athlete group also included those persons who continued to play despite their ACL insufficiency. The non-athlete group comprised all other patients who were not involved in any kind of sports activities. Patients above 50 years of age, those with bicruciate injuries and those who had previous surgeries were excluded. The most common mode of injury in the athlete group was football, while in the non-athlete group, two-wheeler road traffic accidents were responsible for the majority of cases.
Each category was further sub-divided into four subgroups – A, B, C and D – based on the time of presentation since injury (refer to Table 1). The mean age at time of injury was 28.4 years for non-athletes and 26.8 years for athletes (range: 16–48 years).
Table 1.
Table showing the group-wise distribution for both the athlete and non-athlete populations
| Sub-groups | Time of presentation | Non-athlete (n) | Athlete (sports injuries) (n) |
|---|---|---|---|
| A | < 3 months | 350 | 137 |
| B | 3 months–1 year | 176 | 176 |
| C | 1–3 years | 162 | 158 |
| D | > 3 years | 112 | 104 |
All of the patients underwent ACL reconstruction with either bone patella tendon bone graft or hamstring grafts. BPTB grafts were preferred for sports persons and those with high-demand activities. Hamstring grafts were preferred for most of the non-athlete injuries. Arthroscopic findings were documented for medial and lateral meniscus and for focal cartilage injuries. Focal cartilage injuries above grade II were included in this study. Statistical analysis of categorical data was carried out using the chi-square test. A p value of 0.05 was considered to be significant.
Results
Table 2 is presented in the form of a master-chart showing the distribution of the meniscal and cartilage injuries in each subgroup.
Table 2.
Master-charta showing the distribution of meniscal and cartilage injuries in each subgroup of the athlete and non-athlete groups
| Sub-groups | Non-athletes | Athletes | ||||||
|---|---|---|---|---|---|---|---|---|
| Percentage with cartilage injury (n) | Percentage with medial meniscal tear (n) | Percentage with lateral meniscal tear (n) | Total no. of patients | Percentage with cartilage injury (n) | Percentage with medial meniscal tear (n) | Percentage with lateral meniscal tear (n) | Total no. of patients | |
| A: < 3 months | 17 (60) | 21 (74) | 36 (126) | 350 | 14 (19) | 31 (42) | 37 (51) | 137 |
| B: 3–12 months | 24 (42) | 31 (55) | 31 (55) | 176 | 9 (25) | 45 (124) | 35 (97) | 276 |
| C: 1–3 years | 27 (44) | 67 (109) | 34 (55) | 162 | 25 (40) | 70 (110) | 48 (76) | 158 |
| D: > 3 years | 55 (62) | 69 (77) | 55 (62) | 112 | 56 (58) | 75 (78) | 50 (52) | 104 |
aColumns are broadly divided into the two broad groups of non-athletes and athletes. The subdivisions in each column for each group denotes different associated injuries. Based on the time since the injury, the rows are divided into four sub-groups, A, B, C and D, representing less than 3 months, 3 months to 1 year, 1–3 years and longer than 3 years, respectively. Values in each cell denote the percentage represented by that sub-group; the values in parentheses are the actual number of patients in each sub-group.
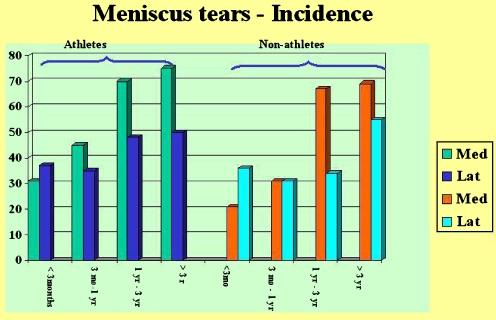
Sub-groups A: < 3 months since injury In those who presented to surgery within 3 months following injury, the incidence of meniscal and cartilage injuries were as follows. In the athlete population, the incidence of medial and lateral meniscal tears was 31 and 37%, respectively; in the non-athlete population, the incidences were 21 and 36%, respectively. The incidence of cartilage injuries was 14% in the athlete population and 17% in the non-athlete population (Fig. 1).
Fig. 1.
Bar diagram showing the incidence of meniscal injuries in athletes and non-athletes in each subgroup
Sub-groups B: 3–12 months since injury The incidences of medial and lateral meniscal tears were 45 and 35% in athletes and 31 and 31% in non-athletes. The incidence of focal cartilage in athletes and non-athletes was 9 and 24%, respectively (Fig. 1).
Sub-groups C: 1–3 years since injury Sub-groups C of both the athlete and non-athlete groups showed a steep increase in the incidence of meniscal and cartilage lesions. In the former, the incidence of medial and lateral meniscal tears was 70 and 48%, respectively, and in the latter, it was 67 and 34%, respectively. The incidence of cartilage damage in athletes and non-athletes was 25 and 27%, respectively (Fig. 1).
Sub-groups D: more than 3 years since injury In those who presented beyond 3 years after injury there was a significantly high incidence of cartilage damage. In the athlete group the incidence of medial and lateral meniscal tears was 75 and 50%, respectively, and in the non-athlete group, it was 69 and 55%, respectively. Cartilage damage was observed in 56% of the athletes and 55% of non-athletes (Fig. 1).
Discussion
Severity of initial injury
Most of the sports injuries in this study were the result of pure pivoting movements, whereas injuries suffered by the non-athlete resulted, in particular, from a two-wheeler road traffic accident setup and thus involved various mechanisms of injury, such as crushing, hyperextension, varus and valgus forces.
The relatively high incidence of cartilage injuries in the non-athlete group (17 vs. 14 %) also highlighted the severity of the initial injury in this group. The severity of the primary injury and subsequent disability is one of the main factors for non-athletes to seek early medical help.
Meniscal tears
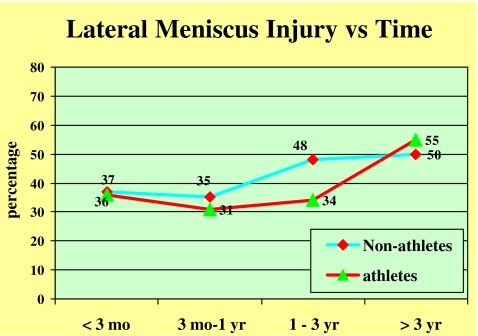
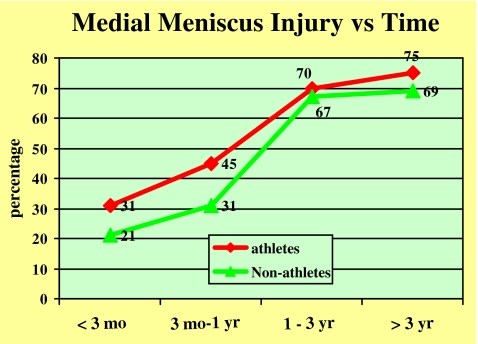
Many studies in the literature report an increased incidence of lateral meniscal injuries relative to medial meniscus ones in patients with ACL insufficiency who present early (less than 1 year) [1, 4, 8, 10]. The incidence of medial meniscal tears increases as the time since the initial injury elapses [5, 9]. Our series also shows a similar pattern of associated injuries. There was a slightly higher incidence of lateral meniscus tears than medial meniscus tears in both groups in those who presented early, while the incidence gradually increased with time since injury in both groups. The incidence of medial meniscal tears rose steeply in both groups who presented very late (over 1 year) (Figs. 2 and 3).
Fig. 2.
Line diagram showing the incidence of lateral meniscal injuries in athletes and non-athletes versus time
Fig. 3.
Line diagram showing the incidence of medial meniscal injuries (percentage) in athletes and non-athletes versus time
These results indicate that primary lateral meniscal tears are slightly more common than medial meniscus ones. The somewhat later increase in the incidence of medial meniscal tears is probably due to secondary tears, which occur as a result of repeated instability episodes. Early reconstruction and stabilisation could have prevented these [11].
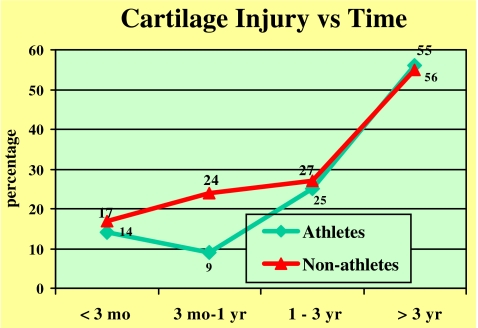
Cartilage damage
Although the non-athlete group showed a slightly higher incidence of cartilage damage in the early sub-groups (up to 1 year), the subsequent increase in incidence reflecting the progression of damage was closely correlated in both the groups. Early osteoarthritic changes, joint space narrowing and osteophyte formation were seen in those who presented many years after the injury in both the groups [6] (Fig. 4).
Fig. 4.
Line diagram showing the incidence of cartilage injuries in athletes and non-athletes (percentage) versus time
There was a statistically significant increase in the incidence of meniscal injuries and cartilage injuries after 1 year in both the groups. There was no difference in the incidence of meniscal and cartilage injuries in athletes and non-athletes among the corresponding groups (chi-square test, p = 0.05). This results shows that both athletes and non-athletes are equally susceptible for long-term meniscal and cartilage injuries if ACL reconstruction is not carried out early [3].
Even though we had excluded patients older than 50 years, the effects of age, sex and weight on the distribution of associated injuries were not included in the study. We included only those patients who presented to our clinic. There is a possibility that there are people with chronic ACL deficiency without any symptoms who have not presented for treatment. Meniscal and cartilage injuries can occur either primarily at the time of injury and/or secondarily due to repeated instability episodes. We were unable to differentiate between these injuries and, consequently ascribed the increased incidence of meniscal and cartilage injuries with late presented groups to secondary injuries. These are the limitations of our study.
Conclusion
It is clearly evident from this study that ACL insufficiency leads to cartilage and meniscal injuries, which in turn can lead to early degenerative changes. Although a percentage of the meniscal and cartilage injuries occur at the time of ACL injury itself, the high incidence of these injuries in those who present late indicates that they result from repeated instability episodes.
In this study we found no difference in the progression of injuries in athletes and non-athletes. Hence, we conclude that there should not be any difference in treating these groups and that both groups could benefit from early ACL reconstruction.
The goals of ACL reconstruction are to ensure a stable knee, thereby preventing further secondary injury and forestalling the progression of degenerative changes. In this era of fitness and quality of life, the benefits of functional knee stability should not be denied to anyone solely on the basis of his/her being a ‘non-athlete’.
Contributor Information
Clement Joseph, Phone: +91-9244401100, FAX: +91-422-2213501, Email: arthroscopy_india@yahoo.co.in.
Shirish S. Pathak, Phone: +91-9994283193, Email: drshirishp@yahoo.com
M. Aravinda, Phone: +91-9443753818, Email: aravindam@rediffmail.com
David Rajan, Phone: +91-9443067090, Email: arthroscopy_india@yahoo.co.in.
References
- 1.Cipolla M, Scala A, Gianni E, Puddu G (1995) Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees. Classification, staging and timing of treatment. Knee Surg Sports Traumatol Arthrosc 3:130–134 [DOI] [PubMed]
- 2.Diekstall P, Rauhut F (1999) Considerations for the indications for anterior cruciate ligament reconstruction. Results of conservative versus operative treatment. Unfallchirurg 102:173–181, Mar [DOI] [PubMed]
- 3.Jerre R, Ejerhed L, Wallmon A, Kartus J, Brandsson S, Karlsson J (2001) Functional outcome of anterior cruciate ligament reconstruction in recreational and competitive athletes. Scand J Med Sci Sports 11:342–346, Dec [DOI] [PubMed]
- 4.Kaeding CC, Pedroza AD, Parker RD, Spindler KP, McCarty EC, Andrish JT (2005) Intra-articular findings in the reconstructed multiligament-injured knee. Arthroscopy 21:424–430, Apr [DOI] [PubMed]
- 5.Keene GC, Bickerstaff D, Rae PJ, Paterson RS (1993) The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med 21:672–679, Sep–Oct [DOI] [PubMed]
- 6.Maffulli N, Binfield PM, King JB (2003) Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy 19:685–690, Sep [DOI] [PubMed]
- 7.Nebelung W, Wuschech H (2005) Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy 21:696–702 [DOI] [PubMed]
- 8.Nikolic DK (1998) Lateral meniscal tears and their evolution in acute injuries of the anterior cruciate ligament of the knee. Arthroscopic analysis. Knee Surg Sports Traumatol Arthrosc 6:26–30 [DOI] [PubMed]
- 9.Church S, Keating JF (2005) Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br 87-B:1639–1642 [DOI] [PubMed]
- 10.Seitz H, Marlovits S, Wielke T, Vecsei V (1996) Meniscus lesions after isolated anterior cruciate ligament rupture. Wien Klin Wochenschr 108:727–730 [PubMed]
- 11.Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, Alturfan A(2004) Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. A Knee Surg Sports Traumatol Arthrosc 12:262–270. Epub 2003 Sep 20 [DOI] [PubMed]