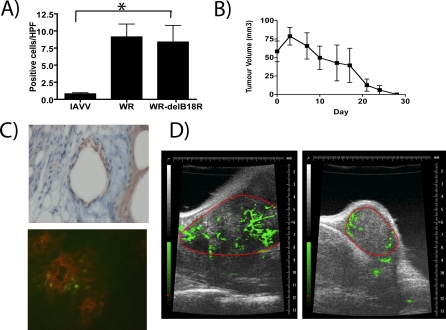
Figure 4. Potential Mechanisms of Tumor Cell Killing Employed by WR-delB18R .
(A) Immunocompetent (C57/B6) mice bearing subcutaneous CMT-93 tumors and treated with a single tail vein injection of 1 × 108 PFU of either psoralen-UV–inactivated WR (IAVV), WR, or WR-delB18R were sacrificed 7 d post-treatment, and CD4-positive cells in tumor sections were scored blind by a pathologist. Average numbers of positive cells per high-powered field (40×) from an average of ten randomly chosen fields from each of three mice treated under each condition are represented (p = 0.035 for IAVV compared to WR-delB18R treated). An asterisk (*) indicates significantly different counts.
(B) Mice treated as in Figure 3C and displaying complete responses were rechallenged with a subcutaneous injection of 5 × 105 CMT-93 cells. Tumor burden was measured by calipers (n = 8 mice).
(C) Mice (C57/B6 bearing subcutaneous CMT-93 tumors) were treated with a single tail vein injection of 1 × 108 PFU of WR-delB18R virus and sacrificed after 24 h. Tumor sections stained for viral coat proteins indicated initial infection of tumor vascular endothelial cells (top), whereas tumors from mice treated as above, but with WR-delB18R expressing GFP (WR-ΔB18RΔTK-GFP), were examined by immunofluorescence following staining with PE-conjugated antibody targeting CD31 (endothelial cells) (bottom; green = viral GFP expression; red = endothelial cell CD31 staining).
(D) Vascular collapse in tumors of mice treated with WR-delB18R. Subcutaneous CMT-93 tumors implanted into C57/B6 mice were examined by ultrasound immediately prior to (left) and 48 h after (right) intravenous treatment with 1 × 108 PFU WR-delB18R. A nonspecific contrast agent was delivered intravenously during ultrasound data acquisition in order to detect tumor vasculature (green); the border of the tumor was manually delineated (red).